Fibromyalgia is a condition that causes pain throughout the whole body. It causes sleep problems, fatigue, and mental/emotional distress. It affects around four million adults in the United States. Individuals with Fibromyalgia tend to be more sensitive to pain. This is referred to as abnormal/altered pain perception processing. Research currently leans towards a hyperactive nervous system as one of the most plausible causes.
Symptoms and Related Conditions
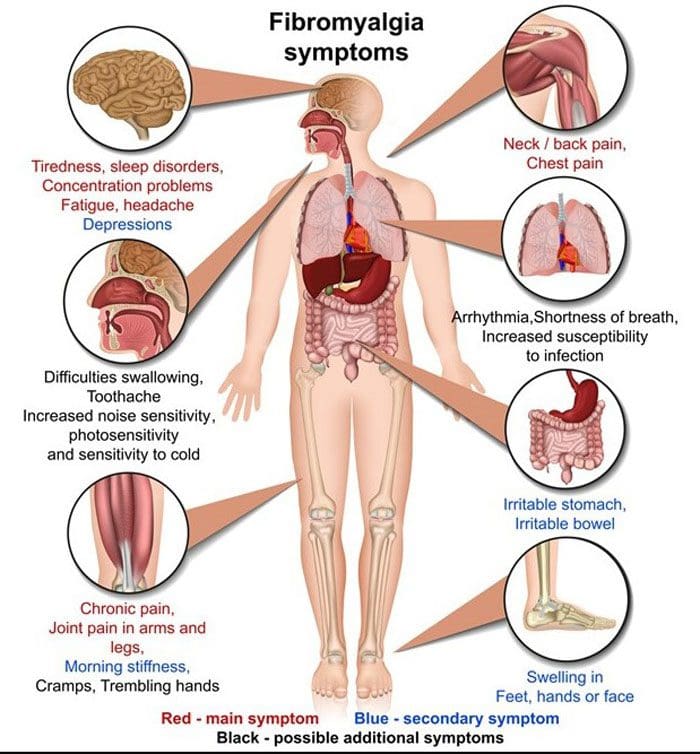
Individuals with fibromyalgia/fibromyalgia syndrome/FMS may have:
- Fatigue
- Sleep issues
- Headaches
- Concentration, Memory issues, or Fibro Fog
- Stiffness
- Tender points
- Pain
- Numbness and tingling in hands, arms, legs, and feet
- Anxiety
- Depression
- Irritable bowel syndrome
- Urinating issues
- Abnormal menstrual cramps
Altered Central Pain Processing
Central sensitization means that the central nervous system, made up of the brain and spinal cord, processes pain differently and more sensitively. For example, individuals with Fibromyalgia could interpret physiological stimuli, like heat, coldness, pressure, as pain sensations. Mechanisms that cause altered pain processing include:
- Pain signal dysfunction
- Modified opioid receptors
- Substance P increase
- Increased activity in the brain where pain signals are interpreted.
Pain Signal Dysfunction
When a painful stimulus is felt, the brain signals the release of endorphins, the body's natural painkillers that block the transmission of pain signals. Individuals with Fibromyalgia could have a pain-blocking system that is altered and/or not functioning correctly. There is also the inability to block repetitive stimuli. This means that the individual keeps feeling and experiencing the stimuli even as they try to block them out, suggesting a failure in the brain to filter out irrelevant sensory information.
Modified Opioid Receptors
Research has found that individuals with fibromyalgia have a reduced number of opioid receptors in the brain. Opioid receptors are where endorphins bind so the body can use them when necessary. With fewer available receptors, the brain is less sensitive to endorphins, as well as opioid pain medication like:
- Hydrocodone
- Acetaminophen
- Oxycodone
- Acetaminophen
Substance P Increase
Individuals with fibromyalgia have been found to have elevated levels of substance P in their cerebrospinal fluid. This chemical is released when a painful stimulus is detected by the nerve cells. Substance P is involved with the body's pain threshold, or the point when a sensation turns into pain. High levels of substance P could explain why the pain threshold is low in individuals with fibromyalgia.
Increased Activity in the Brain
Brain imaging tests, like magnetic resonance imaging or MRI, have shown that fibromyalgia is associated with greater than regular activity in areas of the brain that interpret pain signals. This can suggest that pain signals are overwhelming those areas or that the pain signals are being processed dysfunctionally.
Triggers
Certain factors can trigger a flare-up. These include:
- Diet
- Hormones
- Physical stress
- Too much exercise
- Not enough exercise
- Psychological stress
- Stressful events
- Sleep Patterns changed
- Treatment changes
- Temperature changes
- Weather changes
- Surgery
Chiropractic
Chiropractic focuses on whole-body wellness. 90% of the central nervous system goes through the spinal cord. A misaligned vertebral bone can create interference and irritation on the nerves. Fibromyalgia is a condition related to the hyperactivity of the nerves; therefore, any vertebral subluxations will complicate and aggravate fibromyalgia symptoms. By realigning the misaligned vertebrae releases the stress off of the spinal cord and spinal nerve root. That is why individuals with fibromyalgia are recommended to add a chiropractor to their healthcare team.
Body Composition
Dietary Supplement Quality Guide
The information herein is not intended to replace a
one-on-one relationship with a qualified health care professional, licensed
physician, and is not medical advice. We encourage you to make your own health
care decisions based on your research and partnership with a qualified health
care professional. Our information scope is limited to
chiropractic, musculoskeletal, physical medicines, wellness, sensitive health
issues, functional medicine articles, topics, and discussions. We provide and
present clinical collaboration with specialists from a wide array of
disciplines. Each specialist is governed by their professional scope of
practice and their jurisdiction of licensure. We use functional health &
wellness protocols to treat and support care for the injuries or disorders of
the musculoskeletal system. Our videos, posts, topics, subjects, and insights
cover clinical matters, issues, and topics that relate to and support, directly
or indirectly, our clinical scope of practice.* Our office has made a reasonable
attempt to provide supportive citations and has identified the relevant
research study or studies supporting our posts. We
provide copies of supporting research studies available to regulatory boards
and the public upon request.
We understand that we cover matters that require an
additional explanation of how it may assist in a particular care plan or
treatment protocol; therefore, to further discuss the subject matter above,
please feel free to ask Dr. Alex
Jimenez or contact us at 915-850-0900.
Dr.
Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed in: Texas & New Mexico*
References
Clauw, Daniel J et al. "The science of fibromyalgia." Mayo Clinic proceedings vol. 86,9 (2011): 907-11. doi:10.4065/mcp.2011.0206
Cohen H. Controversies and challenges in fibromyalgia: a review and a proposal. Ther Adv Musculoskelet Dis. 2017 May;9(5):115-27.
Garland, Eric L. "Pain processing in the human nervous system: a selective review of nociceptive and biobehavioral pathways." Primary care vol. 39,3 (2012): 561-71. doi:10.1016/j.pop.2012.06.013
Goldenberg DL. (2017). Pathogenesis of fibromyalgia. Schur PH, (Ed). UpToDate. Waltham, MA: UpToDate Inc.
Kamping S, Bomba IC, Kanske P, Diesch E, Flor H. Deficient modulation of pain by a positive emotional context in fibromyalgia patients. Pain. 2013 Sep;154(9):1846-55.




