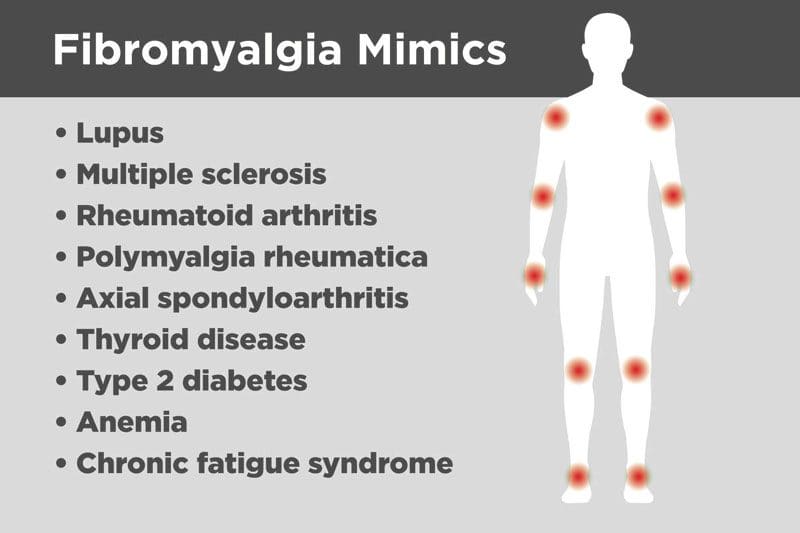
A fibromyalgia diagnosis involves the process of eliminating other disorders and conditions with similar symptoms. It can be difficult to diagnose fibromyalgia. There is no common exam or test that a doctor can use to definitively diagnose fibromyalgia. The elimination process is utilized because of several other conditions with similar symptoms. These include:
- Rheumatoid arthritis
- Chronic fatigue syndrome
- Lupus
It can take some time when an individual first notices symptoms and actually being diagnosed with fibromyalgia, which can be frustrating. Doctors have to become detectives, working hard to find the right cause of pain and other symptoms. Developing the right diagnosis is necessary to create an optimal treatment plan.
Fibromyalgia Diagnosis Criteria
- Pain and symptoms based on the total number of painful areas
- Fatigue
- Poor sleep
- Thinking problems
- Memory problems
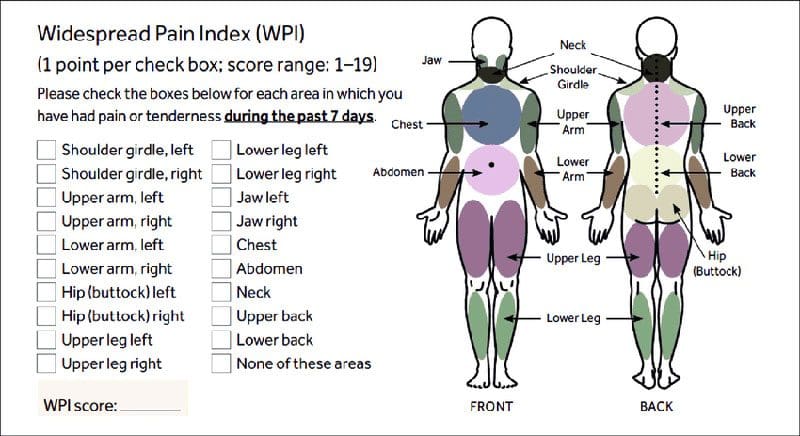
In 2010, a study was published that updated the diagnostic criteria for fibromyalgia. The new criteria remove the emphasis on tender point examination. The 2010 criteria's focus is more on the widespread pain index or WPI. There is an item checklist about where and when an individual experiences pain. This index is combined with a symptom severity scale, and the end result is a new way to classify and develop a fibromyalgia diagnosis.
Diagnostic Process
Medical History
A doctor will look at an individual's complete medical history, asking about any other conditions present and family condition/disease history.
Symptoms Discussion
The most common questions asked by a doctor are where it hurts, how it hurts, how long it hurts, etc. However, an individual should offer as much or added details of their symptoms. Diagnosing fibromyalgia is very dependent on the report of the symptoms, so it is important to be as specific and accurate as possible. A pain diary, which is a record of all symptoms that present will make it easier to remember and share information with the doctor. An example is giving information on trouble sleeping, with a feeling of tiredness a majority of the time, and headache presentation.
Physical Examination
A doctor will palpate or apply light pressure with the hands around the tender points.

Other Tests
As previously stated symptoms can be very similar to other conditions like:
- Rheumatoid arthritis
- Hypothyroidism
- Ankylosing spondylitis
A doctor wants to rule out any other conditions, so they will order various tests. These tests are not to diagnose fibromyalgia but to eliminate other possible conditions. A doctor could order:
Anti-nuclear antibody - ANA test
Anti-nuclear antibodies are abnormal proteins that can present in the blood if an individual has lupus. The doctor will want to see if the blood has these proteins to rule out lupus.
Blood count
By looking at an individual's blood count, a doctor will be able to develop other possible causes for extreme fatigue like anemia.
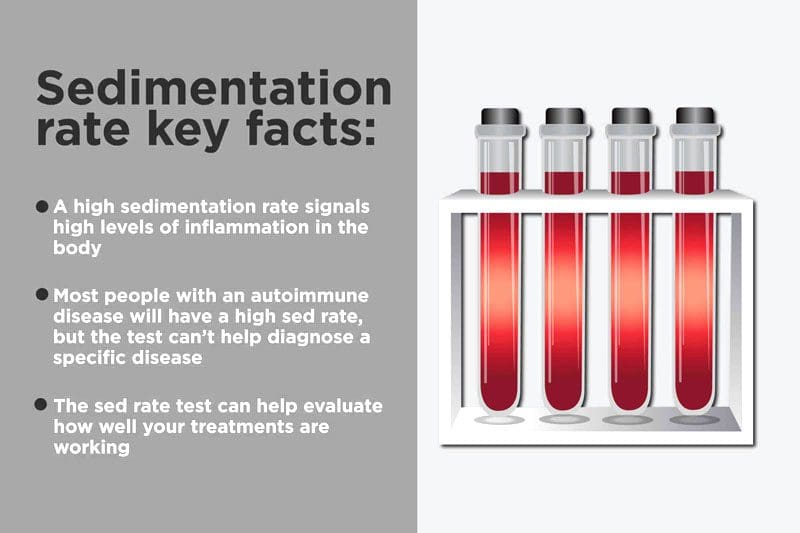
Erythrocyte sedimentation rate - ESR
An erythrocyte sedimentation rate test measures how quickly red blood cells fall to the bottom of a test tube. In individuals with a rheumatic disease like rheumatoid arthritis, the sedimentation rate is higher. The red blood cells fall quickly to the bottom. This suggests that there is inflammation in the body.
Rheumatoid factor - RF test
For individuals with an inflammatory condition like rheumatoid arthritis, a higher level of the rheumatoid factor can be identified in the blood. A higher level of RF does not guarantee that the pain is caused by rheumatoid arthritis, but doing an RF test will help the doctor explore a possible RA diagnosis.
Thyroid tests
Thyroid tests will help a doctor rule out thyroid problems.
Final Note Fibromyalgia Diagnosis
Again, diagnosing fibromyalgia can take awhile. A patient's job is to be proactive in the diagnostic process. Be sure you understand what the results will tell and how that specific test will help figure out the cause of the pain. If you don't understand the results, keep asking questions until it makes sense.
InBody
Body composition and Diabetes Connection
The body needs a balance of lean body mass and fat mass to function properly/optimally and maintain overall health. The balance can be disrupted in overweight and obese individuals because of excess fat. Individuals that are overweight should focus on improving body composition by reducing fat mass while maintaining or increasing lean body mass. Balanced body composition can reduce the risk of diabetes, other obesity-related disorders, and a positive effect on metabolism. Metabolism is the breaking down of foods for energy, the maintenance, and repair of body structures.
The body breaks down the food nutrients/minerals into elemental components and directs them to where they need to go. Diabetes is a metabolic disorder meaning it changes the way the body makes use of the nutrients, in such a way that the cells are unable to utilize digested glucose for energy. Without insulin, the glucose cannot get into the cells, so it ends up lingering in the blood. When the glucose can’t make its way out of the blood, it builds up. All the excess blood sugar can potentially be converted to triglycerides and stored as fat. With an increase in fat mass, hormone imbalances or systemic inflammation can happen or progress. This increases the risk for other diseases or conditions. A buildup of fat and diabetes are associated with increased risk for:
- Heart attacks
- Nerve damage
- Eye problems
- Kidney disease
- Skin infections
- Stroke
Diabetes can even cause the immune system to become impaired. When combined with poor circulation to the extremities, the risk of wounds, infections, can lead to amputation of the toes, foot/feet, or leg/s.
Dr. Alex Jimenez’s Blog Post Disclaimer
The scope of our information is limited to chiropractic, musculoskeletal, physical medicines, wellness, and sensitive health issues and/or functional medicine articles, topics, and discussions. We use functional health & wellness protocols to treat and support care for injuries or disorders of the musculoskeletal system. Our posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate and support directly or indirectly our clinical scope of practice.*
Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. We understand that we cover matters that require an additional explanation as to how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. The provider(s) Licensed in Texas& New Mexico*
References
American College of Rheumatology. Fibromyalgia. 2013. http://www.rheumatology.org/Practice/Clinical/Patients/Diseases_And_Conditions/Fibromyalgia/. Accessed December 5, 2014.
Living with Fibromyalgia: Mayo Clinic Proceedings. (June 2006) “Improvement in Fibromyalgia Symptoms With Acupuncture: Results of a Randomized Controlled Trial” https://www.sciencedirect.com/science/article/abs/pii/S0025619611617291
What Are Common Fibromyalgia Symptoms and How Does It Cause Back Pain?: Clinical Biomechanics. (July 2012) “Functional capacity, muscle strength and falls in women with fibromyalgia” https://www.sciencedirect.com/science/article/abs/pii/S0268003311003226




