A variety of health issues can cause common symptoms which may make it difficult for people to determine the source of their pain and discomfort. Because sciatica is a collection of symptoms rather than a single condition, sciatic nerve pain can often be a frequent symptom for many health issues. The purpose of the following article is to demonstrate the differences between true sciatica and painful symptoms associated with other health issues, such as ischiofemoral impingement.
What is Sciatica?
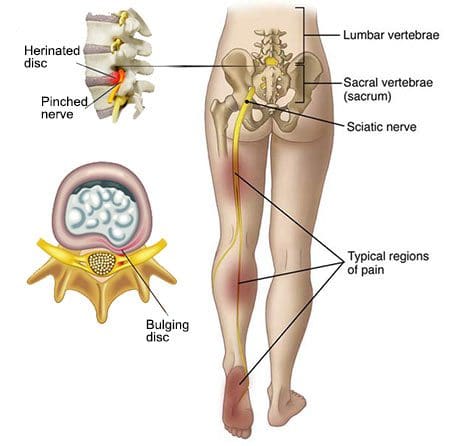
Sciatica is characterized as pain, tingling sensations, and numbness, due to compression or impingement anywhere along the length of the sciatic nerve. The sciatic nerve is the largest nerve in the human body and it stretches from the lower back through the hips and buttocks, down into the legs and feet. Sciatica can affect one or both sides of the human body.
Symptoms
The characteristic symptoms of sciatica can range from mild to severe where the sciatic nerve pain is described as a dull ache to pain or as a sharp, searing, or electric-like pain. Symptoms differ from one person to another. By way of instance, some people may experience shooting pain while some people may only experience tingling sensations and/or numbness.
The common symptoms of sciatica, also known as sciatic nerve pain, include:
- Radiating pain along the length of the sciatic nerve
- Discomfort, tingling sensations, and numbness
- Muscle weakness in the lower back, hips, legs, and feet
- A combination of pain, discomfort, tingling sensations and numbness
- Painful sensations on one or both sides of the human body
Causes
Sciatica commonly occurs when an underlying health issue results in the compression or impingement of the sciatic nerve in the lower back. A bulging or herniated disk is one of the most common causes of sciatica. However, a variety of other underlying health issues can cause sciatica and determining what causes sciatica is necessary for proper treatment.
The most common causes of sciatic nerve pain, or sciatica, include:
- Bulging disk
- Herniated disk
- Degenerative disk disease
- Bone spur osteophytes, or bone spurs
- Spinal stenosis
- Piriformis Syndrome
- Arthritis
Treatments
Sciatica will often resolve on its own over several weeks. Healthcare professionals recommend the use of over-the-counter drugs and/or medications, ice or heat packs on the affected areas, stretches, and exercise, among other alternative treatment options to help reduce sciatica. If symptoms worsen or do not resolve on their own, seek immediate medical attention.
People with mild or moderate sciatica may find relief from any of the following treatments, including:
- Ice or heat therapy
- Stretches and exercises
- Physical therapy
- Chiropractic care
- Acupuncture
- Alexander technique or Feldenkrais method
- Yoga
- Drugs and/or medications
If these approaches do not help reduce sciatica, the patient may need to take one or more imaging tests, such as an X-ray or magnetic resonance imaging (MRI), to diagnose the source of their symptoms. It's important to note that sciatica is a collection of symptoms rather than a single condition. Sciatica may be caused by a variety of underlying health issues.
What is Ischiofemoral Impingement?
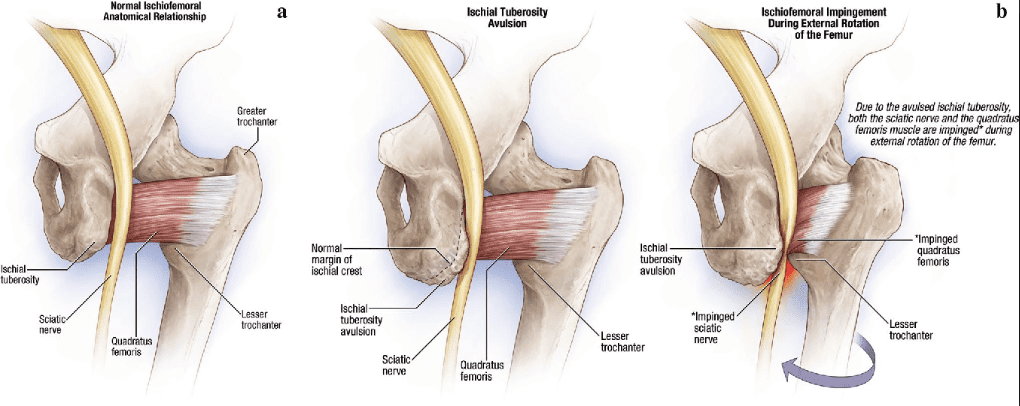
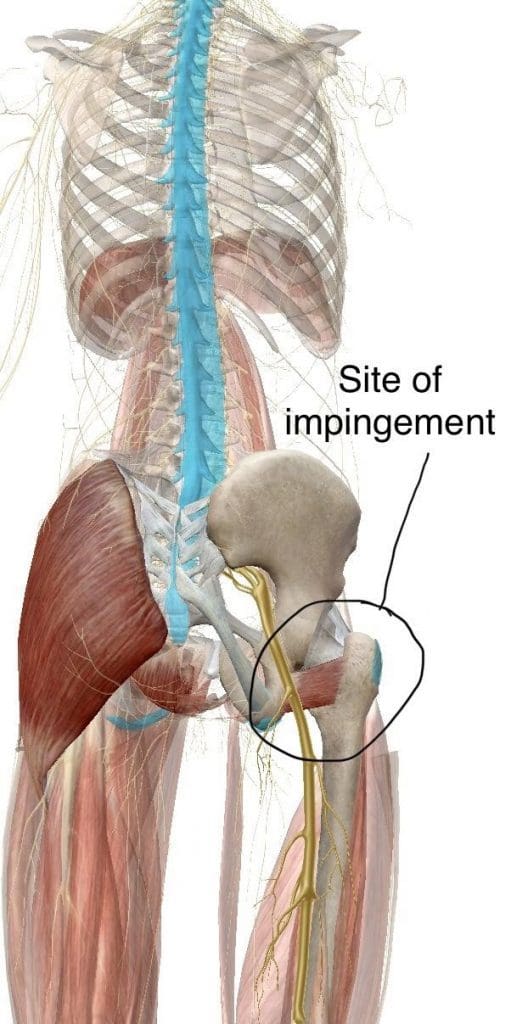
Ischiofemoral impingement syndrome is a condition which occurs when the ischium and the head of the femur experience excessive amounts of pressure, generally due to trauma, overuse, or surgery. The trauma, overuse, or surgery, can also cause bone spurs to grow along the ischium. This gives the bones an abnormal shape which makes them no longer fit together.
Because these don’t fit properly together anymore, the bones may then start to rub against each other during movement causing friction which can damage the joint and cause painful symptoms. As friction worsens, the pain may also increase and restrict movements. The symptoms for ischiofemoral impingement may vary and treatment can also depend on symptoms.
Symptoms
The main symptom of ischiofemoral impingement syndrome is hip pain. The pain from this underlying health issue may start off as mild, however, it can often worsen as the rubbing of the bones causes more damage and inflammation. Ischiofemoral impingement syndrome can feel similar to a pulled hamstring but the pain is generally closer to the buttocks.
Causes
Ischiofemoral impingement occurs due to excess friction between the top of the thighbone, or the femur, and the hip bone, or the ischium. These two bones generally touch in a way which allows them to move without causing pain, however, trauma, overuse, and surgery can ultimately damage the bone. Moreover, if the damage causes a bone spur to grow on the hip or femur, as described above, the extra piece of bone can cause more damage and make the condition worse.
People who experience pain in the hips, buttocks, or groin that does not go away, should seek immediate medical attention to determine the underlying cause of their symptoms. Several of the symptoms associated with ischiofemoral impingement syndrome may be similar to other health issues, including sciatica, muscle, ligament and tendon tears, or fractures. A healthcare professional can perform a diagnosis to rule out ischiofemoral impingement as well as these other conditions.
Diagnosis
To diagnose an ischiofemoral impingement, the healthcare professional may perform a physical exam. During the evaluation, doctor may feel specific areas in the hips to determine the presence of an ischiofemoral impingement. If the healthcare professional suspects you may have ischiofemoral impingement syndrome, they may request additional imaging tests, such as an X-ray or MRI, to confirm the diagnosis. Treatment will depend on the diagnosis of the source of the symptoms.
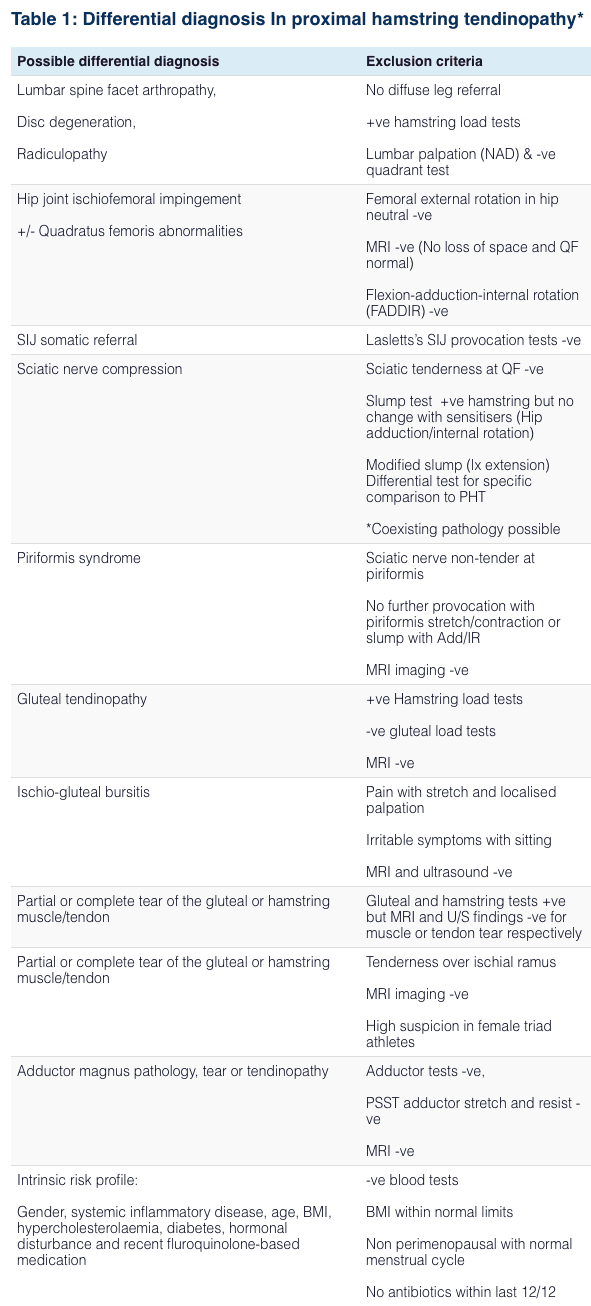
Ischiofemoral Impingement Syndrome is quite an uncommon diagnosis for hip and groin pain – thus it is important that more common conditions like those listed below, are ruled out by a qualified Medical Professional, Chiropractor or Physiotherapist before considering it as a diagnosis:
- Lumbar disc disease
- Spinal stenosis
- Bursitis
- Osteoarthritis
- Rheumatoid arthritis
- Cancer
- Inguinal hernias
- Inguinal lymphadenopathy
- Menstrual conditions
- Urinary tract problems
- Pelvic inflammatory diseases
- Femoroacetabular impingement/piriformis syndromes
Treatments
There is no single treatment which can be utilized to help improve ischiofemoral impingement syndrome. The healthcare professional might recommend a variety of alternative conservative treatment options. By way of instance, they may restrict physical activities or they may recommend rest as well as prescribe drugs and/or medications to help ease the symptoms.
There are many dynamic treatment protocols that can assist in these diagnoses.
If alternative treatment options do not help improve the ischiofemoral impingement, the healthcare professional may also recommend the utilization of injections which contain pain medicine and/or steroids to help control the pain. If neither of these treatment approaches helps relieve the symptoms, the healthcare professional may also recommend surgery.
Due to the rarity of Ischiofemoral Impingement, treatment for the condition has varied on a case by case basis. However, conservative treatment is broadly recommended as a first line approach to resolving the condition. Current conservative treatment strategies in the literature for Ischiofemoral Impingement Syndrome include:
- Nonsteroidal anti-inflammatory drugs and Gabapentin for pain associated with quadratus femoris muscle and sciatic nerve irritation
- Heat, Ultrasound, and Interferential current therapies applied around the hip area.
- Deep Specialized Myofascial protocols can be used.
- An individually prescribed exercise program by a Physiotherapist or joint specialist targeting muscles like the quadriceps femoris, piriformis in order to adequately reduce pain and increase the range of motion in the hip joint.
- CT-guided steroid and local anesthetic injection around the QFM may provide pain relief
Surgical intervention in order to correct/decompress anatomical pathology such as that first described by Johnson in 1977 is reserved for cases that do not respond to conservative therapy. Potential surgical interventions include excision of the lesser trochanter (in those experiencing pain post hip surgery), and more recent/popular peri-articular endoscopic decompression around the hip 2,7. Further research is required to better understand Ischiofemoral Impingement Syndrome – its causes, at-risk populations, and optimal management strategies- both conservative and surgical. As this condition is not yet widely recognized and understood.
Differential Diagnosis In Proximal Hip Pain Syndroms
Sciatica, or sciatic nerve pain, commonly characterized by pain and discomfort, tingling sensations, and numbness, can be a common symptom for a variety of underlying health issues, such as ischiofemoral impingement. Because sciatica is well-known as a collection of symptoms, rather than a single condition or disorder, patients with sciatic nerve pain should seek immediate medical attention to determine if their painful symptoms are caused by another underlying health issue. Treatment for both sciatica and ischiofemoral impingement will depend on the symptoms and diagnosis. There are many treatment options for these complex cases - Dr. Alex Jimenez D.C., C.C.S.T. Insight
The article above demonstrates the differences between true sciatica and painful symptoms associated with other health issues, such as ischiofemoral impingement, to help provide a diagnosis and treatment. The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topic Discussion: Severe Sciatica
Back pain is one of the most prevalent causes of disability and missed days at work worldwide. Back pain attributes to the second most common reason for doctor office visits, outnumbered only by upper-respiratory infections. Approximately 80 percent of the population will experience back pain at least once throughout their life. Your spine is a complex structure made up of bones, joints, ligaments, and muscles, among other soft tissues. Injuries and/or aggravated conditions, such as herniated discs, can eventually lead to symptoms of sciatica, or sciatic nerve pain. Sports injuries or automobile accident injuries are often the most frequent cause of painful symptoms, however, sometimes the simplest of movements can have these results. Fortunately, alternative treatment options, such as chiropractic care, can help ease sciatic nerve pain, or sciatica, through the utilization of spinal adjustments and manual manipulations, ultimately improving pain relief.
Formulas for Methylation Support

XYMOGEN’s Exclusive Professional Formulas are available through select licensed health care professionals. The internet sale and discounting of XYMOGEN formulas are strictly prohibited.
Proudly, Dr. Alexander Jimenez makes XYMOGEN formulas available only to patients under our care.
Please call our office in order for us to assign a doctor consultation for immediate access.
If you are a patient of Injury Medical & Chiropractic Clinic, you may inquire about XYMOGEN by calling 915-850-0900.
For your convenience and review of the XYMOGEN products please review the following link.*XYMOGEN-Catalog-Download
* All of the above XYMOGEN policies remain strictly in force.
References
Singer, Adam D., Ty K. Subhawong, Jean Jose, Jonathan Tresley, and Paul D. Clifford. “Ischiofemoral impingement syndrome: a meta-analysis.” Skeletal radiology 44, no. 6 (2015): 831-837
Johnson, K. A. “Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases.” JBJS 59, no. 2 (1977): 268-269
Spencer-Gardner, Luke, Asheesh Bedi, Michael J. Stuart, Christopher M. Larson, Bryan T. Kelly, and Aaron J. Krych. “Ischiofemoral impingement and hamstring dysfunction as a potential pain generator after ischial tuberosity apophyseal fracture non-union/malunion.” Knee Surgery, Sports Traumatology, Arthroscopy 25, no. 1 (2017): 55-61
Lee, Soyoung, Inhwan Kim, Sung Moon Lee, and Jieun Lee. “Ischiofemoral impingement syndrome.” Annals of rehabilitation medicine 37, no. 1 (2013): 143