Muscular energy techniques, or METs, are considered to be some of the most valuable tools any healthcare professional can have and there are several reasons for it. METs have a wide application range and essential modifications can be made for each of them for a variety of injuries and/or conditions. Muscular energy techniques also represent an important aspect of rehabilitation. Furthermore, METs are both gentle and effective. But most importantly, METs actively involve the patient in the recovery process. Unlike other types of treatment therapies, the patient is involved in every step, contracting at the appropriate time, relaxing at the appropriate time, engaging in eye movement, and even breathing when instructed by the healthcare professional.
Muscular energy techniques have been used with other treatment modalities, such as the McKenzie method, to improve the outcome measures of injuries or conditions. The following research study demonstrates clinical and experimental evidence on the impact of the McKenzie method with METs for low back pain, one of the most common complaints affecting spine health. The purpose of the article is to educate and advice patients with low back pain on the use of METs with the McKenzie method.
Impact of McKenzie Method Therapy Enriched by Muscular Energy Techniques on Subjective and Objective Parameters Related to Spine Function in Patients with Chronic Low Back Pain
Abstract
- Background: The high incidence and inconsistencies in diagnostic and therapeutic process of low back pain (LBP) stimulate the continuing search for more efficient treatment modalities. Integration of the information obtained with various therapeutic methods and a holistic approach to the patient seem to be associated with positive outcomes.The aim of this study was to analyze the efficacy of combined treatment with McKenzie method and Muscle Energy Technique (MET), and to compare it with the outcomes of treatment with McKenzie method or standard physiotherapy in specific chronic lumbar pain.
- Material/Methods: The study included 60 men and women with LBP (mean age 44 years). The patients were randomly assigned to 1 of 3 therapeutic groups, which were further treated with: 1) McKenzie method and MET, 2) McKenzie method alone, or 3) standard physiotherapy for 10 days. The extent of spinal movements (electrogoniometry), level of experienced pain (Visual Analogue Scale and Revised Oswestry Pain Questionnaire), and structure of the spinal discs (MRI) were examined prior to the intervention, immediately thereafter, and 3 months after the intervention.
- Results: McKenzie method enriched with MET had the best therapeutic outcomes. The mobility of cervical, thoracic, and lumbar spine normalized at levels corresponding to 87.1%, 66.7%, and 95% of respective average normative values. Implementation of McKenzie method, both alone and combined with MET, was associated with a significant decrease in Oswestry Disability Index, significant alleviation of pain (VAS), and significantly reduced size of spinal disc herniation.
- Conclusions: The combined method can be effectively used in the treatment of chronic LBP.
- MeSH Keywords: Low Back Pain, Manipulation, Chiropractic, Manipulation, Spinal
Background
Low back pain (LBP) is the most prevalent form of musculoskeletal disorder. According to published statistical data, 70–85% of people experience LBP at some stage of their lives [1–7]. Only 39–76% of the patients recover completely after an acute episode of pain, suggesting that a considerable fraction of them develop a chronic condition [8].
The goals of physiotherapy in patients with chronic LBP include elimination of pain, restoration of the lost extent of movements, functional improvement, and improvement of the quality of life. These objectives are achieved by various protocols of exercise, manipulation, massage, relaxation techniques, and counselling. Although numerous previously published studies have dealt with various therapeutic modalities of LBP, the evidence of their efficacy is highly inconclusive [9–12]. At present the management of chronic LBP still raises many controversies. Inconsistency of established diagnoses and implemented protocols of management points to the importance of the problem in question. Despite extensive research, the issue of spinal pain management still constitutes a challenge for physicians, physiotherapists, and researchers [8,13].

McKenzie method is 1 of many treatment modalities of LBP. It is a system of mechanical diagnosis and management of spinal pain syndromes, based on comprehensive and reproducible evaluation, knowledge of symptoms patterns, directional preference, and centralization phenomenon. This method is focused on the spinal disc disorders [14]. McKenzie method is based on the phenomenon of movement of the nucleus pulposus inside the intervertebral disc, depending on the adopted position and the direction of the movements of the spine. The nucleus pulposus that is exposed to the pressure from both surfaces of the vertebral bodies takes the shape of a spherical joint. This means that it has the ability to perform 3 rotary movements in all directions and has 6 degrees of freedom of movement. The nucleus pulposus performs the movements of flexion, extension, lateral bend (left and right), rotation (right and left), linear displacement (slip) along the sagittal axis, linear displacement along the transverse axis and the separation or approximation along the vertical axis [15].Numerous studies have shown that during forward bend of the spine it is possible to observe extension of the rear surface of the fibrous ring, compressing of the front part of the intervertebral disc and the shift of nucleus pulposus to the dorsal side. When stretching, the mechanism is the opposite [16].
The musculoskeletal system is vital for the maintenance of the balanced tension of the body. Musculofascial disorders can be associated with various problems, pain, or even loss of some motor function. Muscle Energy Techniques (MET) are among the most popular therapeutic modalities aimed at the improvement of elasticity in contractile and non-contractile tissues [17].
High incidence, inconsistencies in diagnostic and therapeutic process, and huge costs associated with the management of chronic spinal disorders stimulate the continuing search for more efficient treatment modalities. This requires the knowledge of neurophysiological processes, proper interpretation of pain, identification of unfavorable motor and postural patterns, holistic approach to the patient, and integration of the information obtained with various therapeutic methods [18].

The aim of this study was to analyze the efficacy of combined treatment with McKenzie method and MET, and to compare it with the outcomes of treatment with McKenzie method or standard physiotherapy in chronic lumbar pain. We evaluated the effect exerted by each of the interventions on the extent of movements, level of experienced pain, and structure of the spinal discs as assessed by means of magnetic resonance imaging.
Material and Methods
Patients
The randomized study included 60 men and women with mean age of 44 years. All individuals were diagnosed by a specialist physician and referred for rehabilitation. The protocol of the study was approved by the Local Bioethical Committee of the Poznan University of Medical Sciences (decision no. 368/0). All patients were diagnosed with chronic spinal pain persisting for longer than 1 year. The inclusion criteria of the study were: 1) documented magnetic resonance imaging (MRI) of the spine, 2) confirmed protrusion or bulging in the lumbosacral spine, 3) intermittent lumbosacral pain, 4) projection of pain to the buttock or thigh, 5) unilateral character of the symptoms. The exclusion criteria were: 1) confirmed extrusion or sequestration of nucleus pulposus of the spinal disc, 2) symptoms manifesting below the knee, 3) history of spinal surgery, 4) structural disorders of spinal discs in more than 2 spinal segments, 5) evident stenosis of the spinal canal, 6) focal lesions of the spinal cord, and 7) spondylolisthesis.
Patients showed great interest and all completed the study.
Protocol
The following tests were used to determine the baseline (i.e. pre-intervention) parameters of the studied patients: 1) electrogoniometric determination of the extent of movement in all spinal segments and angular values of physiological curvatures, 2) Oswestry questionnaire, and 3) Visual Analogue Scale (VAS). Subsequently, the patients were randomly assigned to 1 of 3 therapeutic groups (20 persons each), which were further treated with: 1) McKenzie method and MET, 2) McKenzie method alone, 3) standard physiotherapy. Each of the 3 therapeutic protocols included 10 daily sessions, performed during 5 consecutive weekdays. 24 hours following the last therapeutic session, the same parameters as at the baseline were determined by the investigator blinded to the treatment assignment. Moreover, all patients were subjected to repeated magnetic resonance.
Therapeutic Intervention
McKenzie group One session lasted 30 minutes. On the basis of the McKenzie spinal pain classification, the derangement syndrome was diagnosed in all patients [14]. The therapy included hyperextension techniques, hyperextension with self-pressure or pressure by the therapist, and hyperextensive mobilization. These techniques were applied in the sagittal plane, following the rule of force progression [14]. Moreover, the patients were asked to self-perform the therapeutic procedure at home (5 cycles per day with 2-hour intervals, 15 repetitions each).
McKenzie + MET group The classic McKenzie method enriched with Muscle Energy Technique was implemented. McKenzie protocol in both groups (McKenzie McKenzie + MET) was the same. All patients in this therapeutic group were also diagnosed with the derangement syndrome. A technique of post-isometric relaxation was used at the end of each therapeutic session. It was characterized by the following parameters: 1) time of contraction equal to 7–10 seconds, 2) intensity of contraction corresponding to 20–35%, 3) beginning in the intermediate extent of movement for a given patient, 4) 3 seconds of interval between consecutive contraction phases, 5) 3 repetitions, 6) contraction of antagonist muscle at the terminal phase of the procedure, 7) passive return to the baseline position. The procedure involved relaxation of the erector spinae muscle group and was performed in a sitting position. The exercise was performed in an anterior and lateral flexion, and in rotation. The therapy involved bilateral parts of the erector spinae so as to balance the muscular tension [17]. The duration of 1 combined session was 40 minutes. Patients treated with the combined method were also asked to exercise at home (5 cycles per day with 2-hour intervals, 15 repetitions each).
Standard treatment group Individuals randomized to this therapeutic group were treated with classical massage, laser therapy, and transcutaneous electrical nerve stimulation (TENS) applied to the lumbosacral region. Additionally, the patients were asked to perform general exercises strengthening spinal and abdominal muscles (once a day at home). The exercises were to be performed for 15 minutes, in a prone, supine, and lateral position. The aim of the training was to strengthen the muscles stabilizing the pelvic girdle, i.e. the erector spinae, quadratus lumborum, rectus abdominis, oblique abdominal, gluteal, and iliopsoas muscles. The classical massage lasted 20 minutes. The laser therapy was conducted with a contact technique with Lasertronic LT-2S device. The duration of laser therapy was 80 seconds (2×40 s). The treatment was applied on both sides of the spinous processes of the lumbar spine. The parameters of the procedure were as follows: energy 32 J, power of radiation 400 mW, wavelength 810 nm, continuous mode. TENS electrotherapy was performed with Diatronic DT-10B device. The electrodes were placed on both sides of the lumbosacral spine. The parameters of the TENS procedure were as follows: duration 15 minutes, frequency 50 Hz, current 20–30 mA (subjectively adjusted), duration of a single impulse 50 microseconds. The total time per session=36 min 20 sec + 15 min as home exercises once a day.
Evaluation of Therapeutic Effect
Electrogoniometry The extent of movements and the angles of spinal curvatures were determined with tensiometric Penny & Giles electrogoniometer in Boocok’s modification [19], which prevents potential measurement bias associated with shifting skin and soft tissues in relation to bones. The electrogoniometer enables linear measurement with a bias no greater than 1°. The measurements were taken according to Lewandowski’s methodology [20]. The reliability of these measurements was previously verified by Szulc et al.21 The reference values used in our study were calculated on the basis of Lewandowski’s measurements taken in a group of about 20 000 individuals [20].
Revised Oswestry pain questionnaire The degree to which the dysfunction of the lumbar spine limited the performance of the activities of daily living was determined with the Revised Oswestry Pain Questionnaire [22,23]. We used the revised version of the questionnaire as it is the only variant of this instrument which examines the changes in the level of lumbar pain. The survey was conducted twice, prior to and after the therapy.
Visual analogue scale (VAS) To verify the efficacy of the therapy, the participants were examined with the visual analogue scale (VAS) at the baseline (prior to the intervention) and 24 hours after completing the treatment [24].
Magnetic resonance imaging The degree of degeneration of the spinal discs and the therapeutic outcome were verified on magnetic resonance imaging performed prior to and after the intervention, at the same time of the day. The examination was conducted in sagittal and axial planes, and used T1- and T2-weighted images. The displacement of the nucleus pulposus was expressed in mm. The methodology of examination was described previously by Fazey et al. [25].
Statistical Analysis
Statistical analysis was conducted with Statistica 10.0 software. Bivariate analysis of variance (AVOVA) with 1 intergroup factor (type of intervention) and 1 intragroup factor (measurement prior to intervention, 24 hours and 3 months after the intervention) was used to analyze the differences in studied parameters resulting from the type of the implemented therapy, and to verify the efficacy of various therapeutic protocols. The significance of differences in multiple comparisons was verified with the Scheffé’s post-hoc test.
Dr. Alex Jimenez's Insight
Low back pain is a common symptom that can be treated in a number of ways. Chiropractic care is one of the most common alternative treatment options for LBP, however, healthcare professionals have started using other treatment modalities to help improve symptoms of low back pain. Physical therapy and exercise have commonly been used together, alongside well-known treatment modalities, to help speed up the patient's recovery process. The research study aims to determine how the McKenzie method and muscular energy techniques can improve low back pain and promote overall health and wellness. As a doctor of chiropractic, the positive effects of physical therapy and exercise is reflected on the recovery of patients.
Results
The significant effects of bivariate interaction (method × time) suggest that the implemented therapeutic methods exerted variable time-dependent effect on the functional parameters of the spine, Oswestry questionnaire scores, values of visual analog scale, and the results of magnetic resonance imaging in patients with chronic low back pain.
Data on the mobility of various spinal segments prior to the intervention, and 24 hours and 3 months after the intervention suggests that the implementation of McKenzie method enriched with MET was reflected by better therapeutic outcome compared to classical McKenzie method and standard physiotherapy. Mobility of various spinal segments in all axes and planes improved significantly as a result of the therapy with McKenzie method enriched in MET. In contrast, the least pronounced improvement of spinal mobility was documented in the case of standard physiotherapy (Tables 1–3).
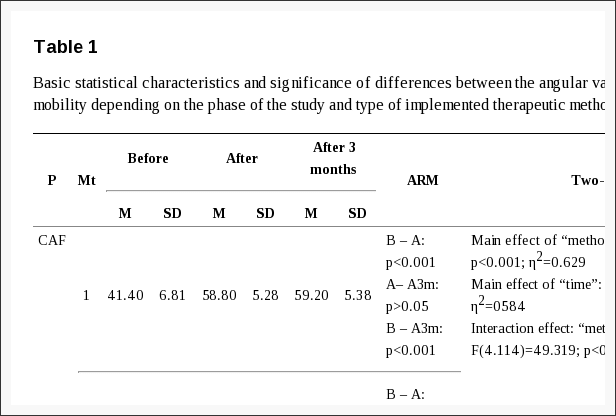
Table 1: Basic statistical characteristics and significance of differences between the angular values of the cervical spine mobility depending on the phase of the study and type of implemented therapeutic method.
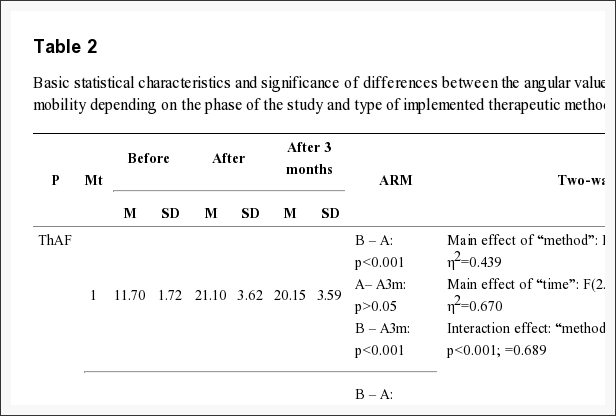
Table 2: Basic statistical characteristics and significance of differences between the angular values of the thoracic spine mobility depending on the phase of the study and type of implemented therapeutic method.
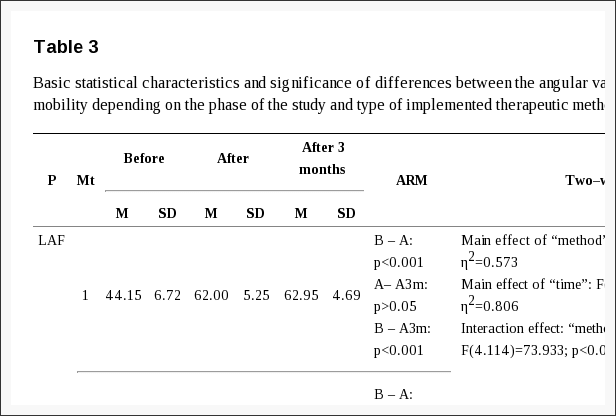
Table 3: Basic statistical characteristics and significance of differences between the angular values of the lumbar spine mobility depending on the phase of the study and type of implemented therapeutic method.
The analysis of the anterior flexion of the cervical spine revealed that the improvement of mobility was most pronounced in McKenzie + MET group (Δ%=42.02). The lack of significant difference between the measurement taken immediately after the intervention and 3 months thereafter suggests that the therapeutic effect was persistent. Less pronounced, albeit significant, improvement of the mobility was also documented in the case of McKenzie method alone (Δ%=14.79); also this effect persisted after 3 months. In contrast, no significant changes in the extent of anterior flexion of the cervical spine were documented in the group subjected to standard physiotherapy (Figure 1).
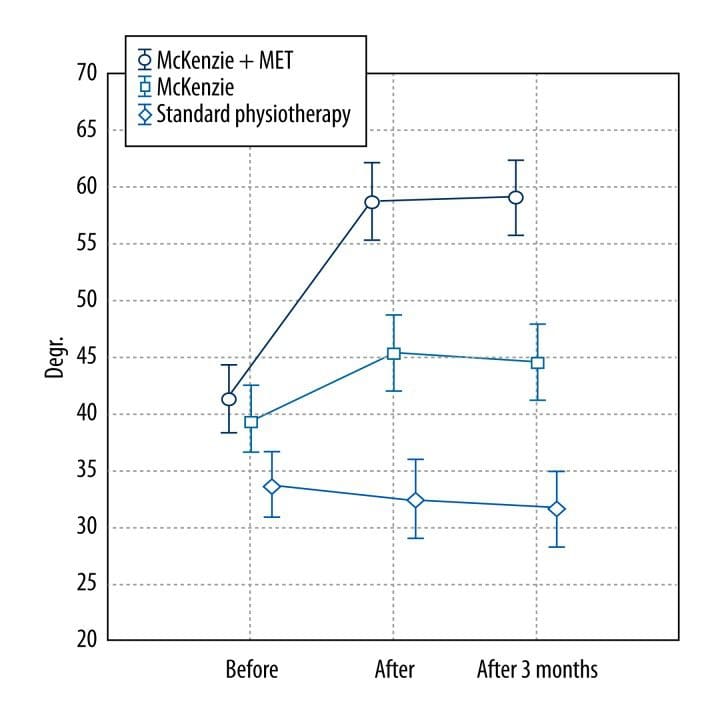
Figure 1: Mean angular values of the anterior flexion of the cervical spine determined at various phases of the study in patients treated with three different therapeutic methods (McKenzie method + MET, McKenzie method alone, standard physiotherapy).
Also, the analysis of changes in the degree of thoracic and lumbar spine anterior flexion revealed variability in the outcomes of the studied methods (Figures 2, 3).
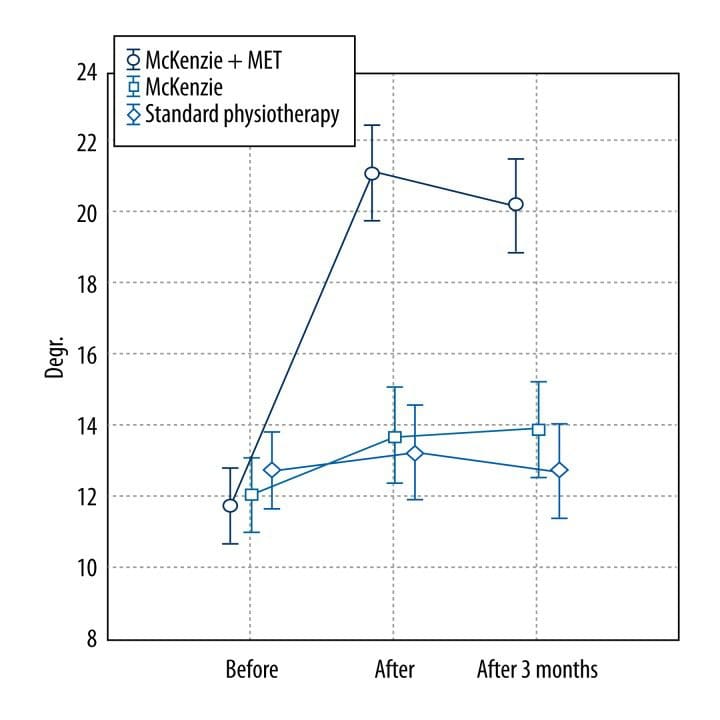
Figure 2: Mean angular values of the anterior flexion of the thoracic spine determined at various phases of the study in patients treated with three different therapeutic methods (McKenzie method + MET, McKenzie method alone, standard physiotherapy).
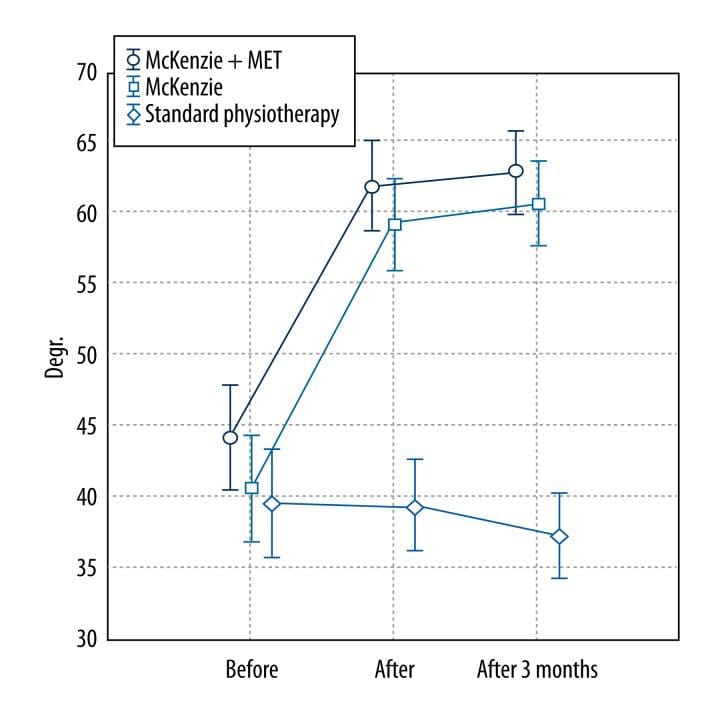
Figure 3: Mean angular values of the anterior flexion of the lumbar spine determined at various phases of the study in patients treated with three different therapeutic methods (McKenzie method + MET, McKenzie method alone, standard physiotherapy).
The greatest improvement of the mobility, equal to Δ%=80.34 and Δ%=40.43 in the thoracic and lumbar segment, respectively, was documented in the McKenzie + MET group. The lack of significant difference between the measurements of both the segments taken immediately after the intervention and 3 months thereafter suggests that the therapeutic effect was persistent (Tables 2, 3). The changes in the remaining functional spinal parameters followed a similar pattern and are summarized in Tables 1–3.
The degree of mobility in various spinal segments observed after implementation of studied therapeutic methods was compared with respective average normative values published by Lewandowski [20[ (Figures 4–6). Implementation of McKenzie method enriched with MET was reflected by the most pronounced improvement in the spinal mobility, which fit within the respective normative ranges. The functional parameters of cervical, thoracic, and lumbar spine normalized at levels corresponding to 87.1%, 66.7%, and 95% of respective average normative values.
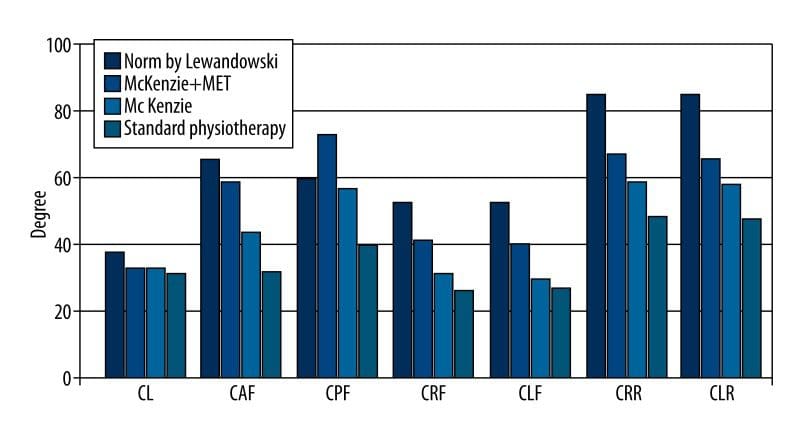
Figure 4: Functional parameters of the cervical spine (CL – cervical lordosis; CAF – cervical anterior flexion; CPF – cervical posterior flexion; CRF – cervical right flexion; CLF – cervical left flexion; CRR – cervical right rotation; CLR – cervical left rotation) – comparison between values determined in patients treated with three different therapeutic methods and respective normative values published by Lewandowski.
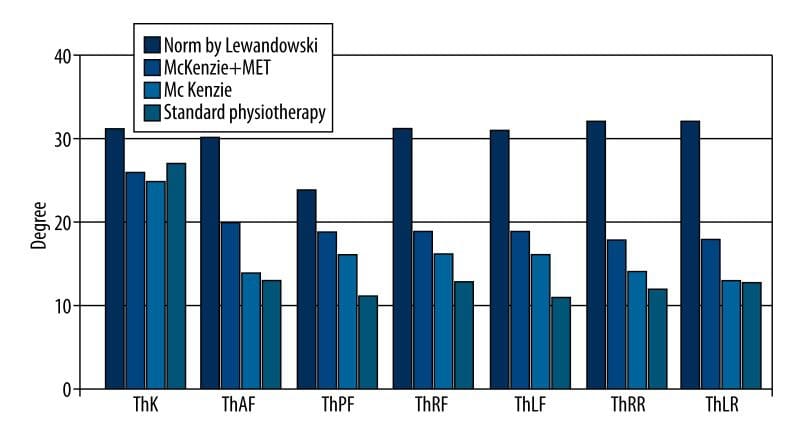
Figure 5: Functional parameters of the thoracic spine (ThK – thoracic kyphosis; ThAF – thoracic anterior flexion; ThPF – thoracic posterior flexion; ThRF – thoracic right flexion; ThLF – thoracic left flexion; ThRR – thoracic right rotation; ThLR – thoracic left rotation) – comparison between values determined in patients treated with three different therapeutic methods and respective normative values published by Lewandowski.
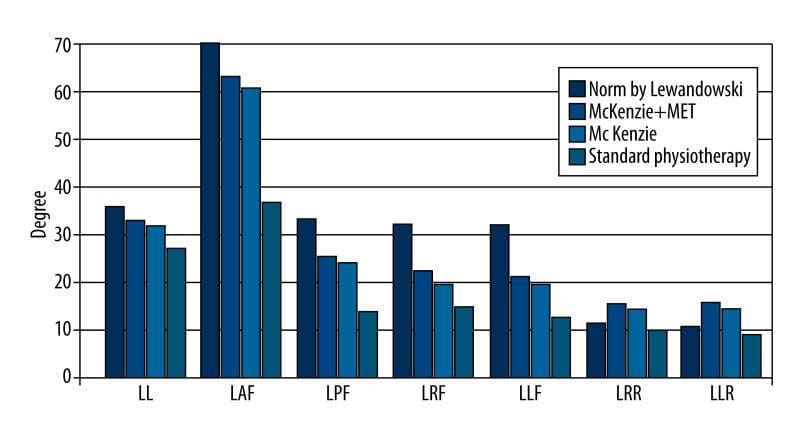
Figure 6: Functional parameters of the lumbar spine (LL – lumbar lordosis; LAF – lumbar anterior flexion; LPF – lumbar posterior flexion; LRF – lumbar right flexion; LLF – lumbar left flexion; LRR – lumbar right rotation; LLR – lumbar left rotation) – comparison between values determined in patients treated with three different therapeutic methods and respective normative values published by Lewandowski.
Irrespective of the therapeutic method and timing of measurement, the angular values of all spinal curvatures fit within the respective normative values and no significant inter- and intragroup differences were documented (Table 4).
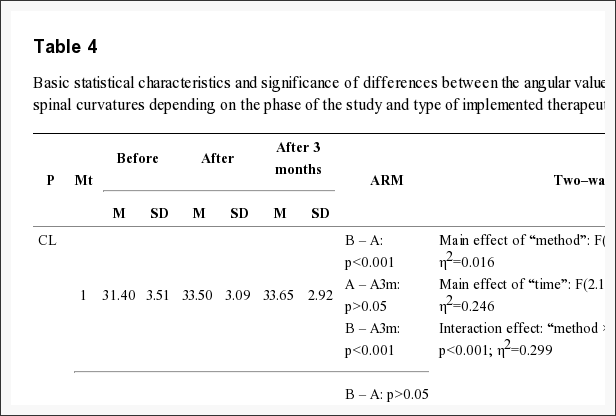
Table 4: Basic statistical characteristics and significance of differences between the angular values of the physiological spinal curvatures depending on the phase of the study and type of implemented therapeutic method.
The scores of Oswestry questionnaire also differed depending on the type of implemented intervention. Implementation of McKenzie method, both alone and combined with MET, was reflected by a significant decrease in Oswestry Disability Index. No significant differences were documented between the outcomes of these 2 methods. In contrast, standard physiotherapy had the least pronounced effect on the Oswestry Disability Index (Table 5).
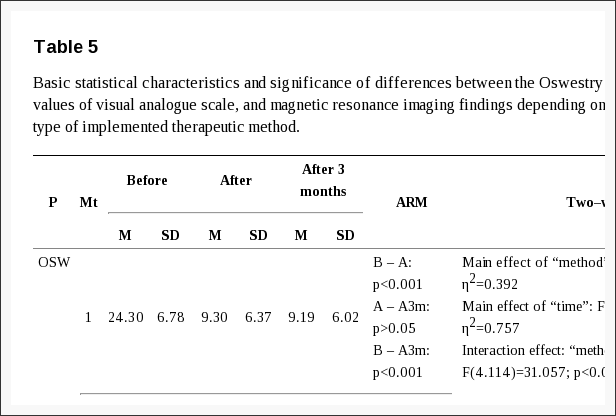
Table 5: Basic statistical characteristics and significance of differences between the Oswestry questionnaire scores, values of visual analogue scale, and magnetic resonance imaging findings depending on the phase of the study and type of implemented therapeutic method.
The analysis of visual analogue scale values suggests that both McKenzie method enriched with MET and classical McKenzie method produced the strongest therapeutic effects, i.e. alleviation of pain. Implementation of both these methods was reflected by marked augmentation of experienced pain, without any significant intergroup differences. In contrast, standard physiotherapy reduced pain to a minimal extent, and no significant differences were observed between VAS scores obtained prior to and after this intervention (Table 5).
Magnetic resonance imaging performed prior to and after the intervention confirmed that McKenzie method enriched with MET produced the best therapeutic outcome manifested by a reduced size of spinal disc herniation. Smaller, albeit significant, improvement of this parameter was also documented in the case of classical McKenzie method. These 2 therapeutic methods did not differ significantly in terms of the post-intervention size of the spinal disc herniation. In contrast, no reduction in the size of the spinal disc herniation was documented after implementation of standard physiotherapy (Table 5).
Discussion
The number of studies validating the efficacy of combined therapeutic methods and techniques is sparse [3,21,26,27]. Wilson et al. [26] concluded that MET is an optimal adjunct technique for other therapeutic modalities [26].
Many studies confirmed the positive effects of McKenzie method [28–36]. Similarly, a body of evidence confirms the therapeutic value of MET [37–44]. Moreover, positive outcomes of both these techniques were documented in patients with spinal pain, including LBP [45,46]. However, to the best of our knowledge, none of the previous studies verified whether the combination of these methods improves the therapeutic outcome.
Noticeably, both the therapies are based on different concepts and involve different therapeutic techniques. The McKenzie method is oriented at the management of all structural abnormalities of the spinal discs. The aim of this therapy is to eliminate pain and normalize function of the affected spinal segment [14]. Therefore, McKenzie method focuses on the treatment of spinal disc pathologies as the principal cause of pain. Takasaki et al. [35] documented positive changes in the spinal disc, i.e. the resolution of herniation, in patient treated with McKenzie method.
However, various injuries and other medical conditions, as well as repetitive negative motor pattern, are also reflected by the disorders of the musculofascial system. This can be reflected by the development of certain compensatory mechanisms, accumulation of muscular tension, motor limitation, and functional disorders [17,40,42]. In contrast, the treatment of the musculofascial system is not included in the concept of McKenzie method. Therefore, the aim of including the muscle energy techniques in the proposed protocol of combined therapy was to potentiate its therapeutic effect through the relaxation and stretching of contracted musculature, strengthening of weakened muscles, reduction of passive muscular tension, improvement of joint mobility, and normalization of motor function [26,43].
The differences observed with regards to the mobility of various spinal segments prior to and after the intervention point to better therapeutic outcome of the combined methods. Noticeably, improved mobility was documented not only in the lumbar spine but also in the cervical and thoracic segment. Therefore, the implementation of MET improved the scope of the combined method (McKenzie + MET) as compared to the classical McKenzie method. Our findings suggest that musculofascial disorders may to a large extent be responsible for limited spinal mobility in patients with chronic LBP. In their papers on the therapeutic effects of manual therapy, Pool et al. [12] and Zaproudina et al. [47] emphasize the importance of limitations in spinal mobility as a sensitive marker of pathological changes.
The magnetic resonance findings documented in patients treated with combined McKenzie method and MET suggest that this combination has no negative effect on the size of spinal disc herniation (Figure 7). This confirms the safety of MET and plausibility of its application in patients with spinal disc pathologies [26]. Of note, relatively large subjective and objective improvements were achieved despite the short duration of the treatment, which included only 10 sessions throughout a 2-week period.
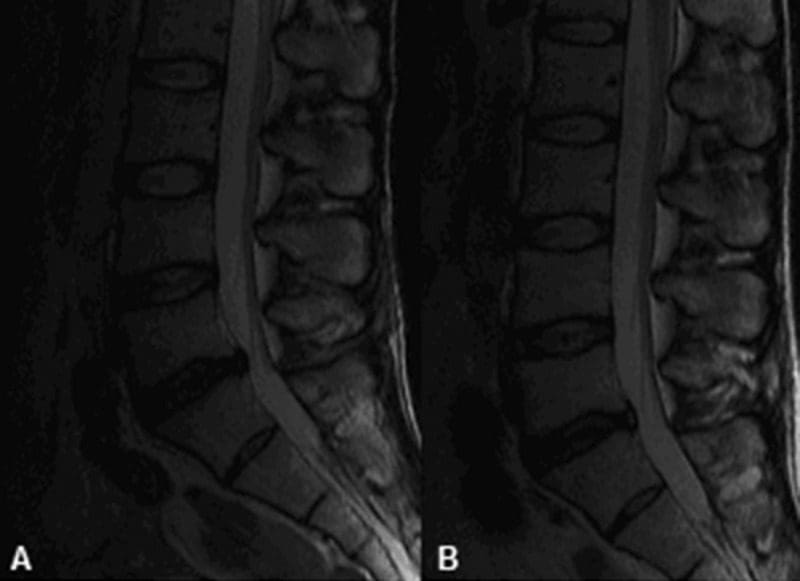
Figure 7: Magnetic resonance images of the structural changes of the L5–S1 spinal disc: (A) prior to, and (B) after the combined therapy (McKenzie method + MET).
Furthermore, control electrogoniometry conducted 3 months after the intervention confirmed the persistent effect of the combined treatment. Moreover, a slight improvement was documented in the case of some functional parameters examined immediately after the intervention and 3 months thereafter. Perhaps, this phenomenon reflected proper education of our patients and further prophylactic self-exercising according to McKenzie method.
Chronic low back pain (CLBP) has a multifactorial etiology [18], and as such requires multimodal treatment. The evidence of therapeutic effects should not be limited to the diagnostic imaging, but mostly be reflected by functionality of a patient, level of experienced pain, extent of movements, and normalization of motor function.
Conclusions
The following conclusions can be formulated on the basis of our findings:
- Comparison of the subjective and objective outcomes of 3 therapeutic methods – standard physiotherapy, McKenzie method alone, and McKenzie method combined with MET – in patients with chronic low back pain suggests that the combined method is the most effective.
- The use of the combined method (McKenzie + MET) exerts a positive effect on structural (resolution of spinal disc herniation documented on MRI) and functional parameters (improved mobility of various spinal segments), improves the quality of life, and reduces the level of experienced pain.
Acknowledgements
The study was conducted under the auspices of the University School of Physical Education in Poznan. The authors express their gratitude to the owners of the Private Rehabilitation Practice “Antidotum” for consent to perform the study in their facility.
Footnotes
- Source of support: The study was supported by the resources from the Ministry of Science and Higher Education for the statutory activity of the Department of Anatomy of the University School of Physical Education in Poznan
- Conflict of interest: None declared.
In conclusion, the research study demonstrating clinical and experimental evidence on the impact of the McKenzie method with METs for low back pain, one of the most common complaints affecting spine health, concluded that the combined treatment modalities were effectively used in the improvement of chronic low back pain. The purpose of the article was to educate and advice patients with low back pain on the use of METs with the McKenzie method. Furthermore, the use of the combined treatment modalities demonstrated a positive effect on structural and functional parameters, improving the patient's quality of life and reducing the level of pain they experienced. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
References
1. Drozda
K, Lewandowski J, Górski P. Back pain in lower and upper secondary
school pupils living in urban areas of Poland. The case of Poznan. Ortopedia, Traumatologia, Rehabilitacja. 2011;13(5(6)):489–503. [PubMed]
2. Drozda K, Lewandowski J. Epidemiology of back pain among secondary school pupils in Poznan. Fizjoterapia Polska. 2011;4(1):31–40.
3. Dunsford
A, Kumar S, Clarke S. Integrating evidence into practice: use of
McKenzie-based treatment for mechanical low back pain. J Multidiscip Healthc. 2011;4:393–402. [PMC free article] [PubMed]
4. Joud A, Petersson IF, Englund M. Low back pain: epidemiology of consultations. Arthritis Care Res (Hoboken) 2012;64:b1084–88. [PubMed]
5. Lewandowski
J, Szulc P, Boch-Kmieciak J, et al. Epidemiology of low back pain in
students of physical education and physiotherapy. Studies in Physical Culture and Tourism. 2011;18(3):265–69.
6. Pereira
LM, Obara K, Dias JM, et al. Comparing the Pilates method with no
exercise or lumbar stabilization for pain and functionality in patients
with chronic low back pain: systematic review and meta-analysis. Clin Rehabil. 2012;26:10–20. [PubMed]
7. Werneke
MW, Hart D, Oliver D, et al. Prevalence of classification methods for
patients with lumbar impairments using the McKenzie syndromes, pain
pattern, manipulation, and stabilization clinical prediction rules. J Man Manip Ther. 2010;18:197–204. [PMC free article] [PubMed]
8. da C Menezes Costa L, Maher CG, Hancock MJ, et al. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012;184:E613–24. [PMC free article] [PubMed]
9. Borges TP, Greve JM, Monteiro AP, et al. Massage application for occupational low back pain in nursing staff. Rev Lat Am Enfermagem. 2012;20:511–19. [PubMed]
10. Cherkin
DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types
of massage and usual care on chronic low back pain: a randomized,
controlled trial. Ann Intern Med. 2011;155:1–9. [PMC free article] [PubMed]
11. Kilpikoski
S, Alèn M, Paatelma M, et al. Outcome comparison among working adults
with centralizing low back pain: Secondary analysis of a randomized
controlled trial with 1-year follow-up. Adv Physiother. 2009;11:210–17.
12. Pool
JJ, Ostelo RW, Knol DL, et al. Is a behavioral graded activity program
more effective than manual therapy in patients with subacute neck pain?
Results of a randomized clinical trial. Spine. 2010;35:1017–24. [PubMed]
13. Frankel BS, Moffett JK, Keen S, et al. Guidelines for low back pain: changes in GP management. Fam Pract. 1999;16:216–22. [PubMed]
14. McKenzie R, May S. The lumbar spine: mechanical diagnosis and therapy. 2nd ed. Waikanae: Spinal Publications; 2003.
15. Kanpandji AI. Anatomia funkcjonalna stawów. Tom 3.6 ed. Wrocław: Elsevier Urban & Partners; 2010. [in Polish]
16. Alexander
LA, Hancock E, Agouris I, et al. The response of the nucleus pulposus
of the lumbar intervertebral discs to functionally loaded positions. Spine. 2007;32(14):1508–12. [PubMed]
17. Chaitow L. Muscle energy techniques. 3rd ed. Edinburgh: Churchill Livingstone; 2006.
18. O’Sullivan P. It’s time for change with the management of non-specific chronic low back pain. Br J Sports Med. 2012;46:224–27. [PubMed]
19. Boocock MG, Jackson JA, Burton AK, et al. Continuous measurement of lumbar posture using flexible electrogoniometers. Ergonomics. 1994;37:175–85. [PubMed]
20. Lewandowski J. Formation
of physiological curvatures and segmental mobility of the human spine
aged from 3 to 25 years in electrogoniometric studies. 1st ed. Poznan: AWF Poznan; 2006.
21. Szulc
P, Lewandowski J, Marecki B. Verification of selected anatomic
landmarks used as reference points for universal goniometer positioning
during knee joints mobility range measurements. Med Sci Monit. 2001;7:312–15. [PubMed]
22. Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25:2940–52. [PubMed]
23. Hicks
GE, Manal TJ. Psychometric properties of commonly used low back
disability questionnaires: are they useful for older adults with low
back pain? Pain Med. 2009;10:85–94. [PMC free article] [PubMed]
24. Mudgalkar
N, Bele SD, Valsangkar S, et al. Utility of numerical and visual
analog scales for evaluating the post-operative pain in rural patients. Indian J Anaesth. 2012;56:553–57. [PMC free article] [PubMed]
25. Fazey PJ, Takasaki H, Singer KP. Nucleus pulposus deformation in response to lumbar spine lateral flexion: an in vivo MRI investigation. Eur Spine J. 2010;19(11):1115–20. [PMC free article] [PubMed]
26. Wilson
E, Payton O, Donegan-Shoaf L, et al. Muscle energy technique in
patients with acute low back pain: a pilot clinical trial. J Orthop Sports Phys Ther. 2003;33:502–12. [PubMed]
27. Bronfort
G, Goldsmith CH, Nelson CF, et al. Trunk exercise combined with spinal
manipulative or NSAID therapy for chronic low back pain: a randomized,
observer-blinded clinical trial. J Manipulative Physiol Ther. 1996;19:570–82. [PubMed]
28. Bybee
RF, Olsen DL, Cantu-Boncser G, et al. Centralization of symptoms and
lumbar range of motion in patients with low back pain. Physiother Theory Pract. 2009;25:257–67. [PubMed]
29. Chen
J, Phillips A, Ramsey M, et al. A case study examining the
effectiveness of mechanical diagnosis and therapy in a patient who met
the clinical prediction rule for spinal manipulation. J Man Manip Ther. 2009;17:216–20. [PMC free article] [PubMed]
30. Garcia
AN, Gondo FL, Costa RA, et al. Effects of two physical therapy
interventions in patients with chronic non-specific low back pain:
feasibility of a randomized controlled trial. Rev Bras Fisioter. 2011;15:420–27. [PubMed]
31. Hosseinifar
M, Akbari M, Behtash H, et al. The effects of stabilization and
Mckenzie exerciseson transverse abdominis and multifidus muscle
thickness, pain, and disability: A randomized controlled trial in
nonspecific chronic low back pain. J Phys Ther Sci. 2012;25:1541–45. [PMC free article] [PubMed]
32. Mbada
CE, Ayanniyi O, Ogunlade SO, et al. Influence of Mckenzie protocol and
two modes of endurance exercises on health-related quality of life of
patients with long-term mechanical low-back pain. Pan Afr Med J. 2014;17(Supp 1):5. [PMC free article] [PubMed]
33. Garcia
AN, da Cunha Menezes Costa L, Hancock MJ, et al. Efficacy of the
McKenzie method in patients with chronic nonspecific low back pain: a
protocol of randomized placebo-controlled trial. Phys Ther. 2015;95:267–73. [PubMed]
34. Schenk RJ, Jozefczyk C, Kopf A. A randomized trial comparing interventions in patients with lumbar posterior derangement. J Man Manip Ther. 2003;11:95–102.
35. Takasaki
H, May S, Fazey PJ, et al. Nucleus pulposus deformation following
application of mechanical diagnosis and therapy: a single case report
with magnetic resonance imaging. J Man Manip Ther. 2010;18:153–58. [PMC free article] [PubMed]
36. Williams
B, Vaughn D, Holwerda T. A mechanical diagnosis and treatment (MDT)
approach for a patient with discogenic low back pain and a relevant
lateral component: a case report. J Man Manip Ther. 2011;19:113–18. [PMC free article] [PubMed]
37. Chugh
R, Kalra S, Sharma N, et al. Effects of muscle energy techniques and
its comparison to self stretch of bilateral ankle plantarflexors on
performance of balance scores in healthy elderly subjects. Physiother Occup Ther J. 2011;4:61–71.
38. Fryer G, Ruszkowski W. The influence of contraction duration in muscle energy technique applied to the atlanto-axial joint. J Osteopath Med. 2004;7:79–84.
39. Fryer
G, Pearce AJ. The effect of muscle energy technique on corticospinal
and spinal reflex excitability in asymptomatic participants. J Bodyw Mov Ther. 2013;17(4):440–47. [PubMed]
40. Gugliotti
M. The use of mobilization, muscle energy technique, and soft tissue
mobilization following a modified radical neck dissection of a patient
with head and neck cancer. Rehabil Oncol. 2011;29:3–8.
41. Kűčűkşen
S, Yilmaz H, Sallı A, Uğurlu H. Muscle energy technique versus
corticosteroid injection for management of chronic lateral
epicondylitis: Randomized controlled trial with 1-year follow-up. Arch Phys Med Rehabil. 2013;94:2068–74. [PubMed]
42. Moore
SD, Laudner KG, McLoda TA, et al. The immediate effects of muscle
energy technique on posterior shoulder tightness: a randomized
controlled trial. J Orthop Sports Phys Ther. 2011;41:400–7. [PubMed]
43. Rajadurai V. The effect of muscle energy technique on temporomandibular joint dysfunction: a randomized clinical trail. Asian J Sci Res. 2011;4:71–77.
44. Shadmehr
A, Hadian MR, Naiemi SS, et al. Hamstring flexibility in young women
following passive stretch and muscle energy technique. J Back Musculoskelet Rehabil. 2009;22:143–48. [PubMed]
45. Day
JM, McKeon P, Nitz A. The efficacy of cervical/thoracic active range of
motion for detecting changes associated with individuals receiving
muscle energy techniques. Phys Ther Rev. 2010;15:453–61.
46. Day JM, Nitz AJ. The effect of muscle energy techniques on disability and pain scores in individuals with low back pain. J Sport Rehabil. 2012;21:194–98. [PubMed]
47. Zaproudina
N, Hietikko T, Hanninen OO, et al. Effectiveness of traditional bone
setting in treating chronic low back pain: a randomised pilot trial. Complement Ther Med. 2009;17:23–28. [PubMed]
Additional Topics: Sciatica
Sciatica is referred to as a collection of symptoms rather than a single type of injury or condition. The symptoms are characterized as radiating pain, numbness and tingling sensations from the sciatic nerve in the lower back, down the buttocks and thighs and through one or both legs and into the feet. Sciatica is commonly the result of irritation, inflammation or compression of the largest nerve in the human body, generally due to a herniated disc or bone spur.






