Chiropractor, Dr. Alexander Jimenez looks at the mechanics of neck injury and assessment techniques.
Nearly half the people will experience Neck pain at some stage during their lives, and also with sport accounting for about 10% of all neck injuries(1), the cervical spine is a place that warrants more focused attention than it currently gets. The incidence of neck injuries in sport is regarded as rising, and it is unquestionably partly due to improvements in injury reporting and monitoring. However the gain in the physicality of sport and the growth of ‘extreme sports’ are departing untrained necks at greater risk of harm.
Working at the sport of skeleton (in which Neck injuries are common in skeleton, and so a clear motivation would be to protect against this. However, neck training isn’t just about injury-risk mitigation; at a sport where the gold medal can be picked by a single hundredth of a second, training aimed at reinforcing the neck so that it may keep the athlete’s chin off the ice, may be the difference between the standing on the podium or applauding in the stands.
So as to reduce the danger of injury, the Neck needs to be specifically and strategically educated to make sure its tolerance is greater than the loads it’s exposed to. But before this training program being implemented, it’s important to correctly assess the cervical spine in a comprehensive assessment and screening procedure. It is this that is going to be the focus of this first article of the two-part string on neck injury and the cervical spine.
How Do Necks Get Injured?
Neck injuries are unsurprisingly most Prevalent in motorsports, in addition to high impact, collision sports like rugby. The reasons for this injury profile include:- Acute force exposure through axial loading
- Direct blows
- Unexpected acceleration/deceleration
Another neck injury that could occur from These can be either compressive or distractive in character and are most common in tackling sports, or as a result of a fall from a height in which the neck is sloping bent and the shoulder girdle depressed.
Stingers are a result of a downward traction Clinicians will need to get a high index of suspicion of spinal cord trauma after any compression or distraction harm, and this serious consequence and has to be cleared with a thorough on-field assessment before the athlete being moved.
‘Whiplash Associated Disorders’ (WAD)
Are commonly seen in the general population. But they can frequently occur in sports between sudden acceleration and deceleration, and may also occur following a blow to the trunk or head(4). A combination of neck pain, headaches, temporal mandibular dysfunction and also referred pain/ neurological disorders are the result of the forces transferred to the throat causing sudden, uncontrolled movement, which results in damage to the anterior and posterior arrangement of the cervical spinal column.The cervical spine is not just prone to acute Injuries however. Chronic pressure exposure from maintained static positions (such as in sports like archery) or constant exposure to gravitational (G) or vibration forces tend to be implicated in the development of overuse symptoms. As with any area of the human body, athletes that are unable to attenuate the forces they are exposed to through their neck will be in a greater risk of injury or dysfunction.
The unwanted effects of continual G-force Exposure include dizziness, disorientation, altered vision, reduced co-ordination, in addition to neck pain(5). Any of these side effects can not only reduce operation, but also set athletes and opponents at risk, particularly if travelling at high speeds!
Much of the research in this area has Been carried out by military air forces, tracking the effect of G-force on pilots.
G force also needs to be considered in Contact sports, where collisions between gamers may expose athletes to drives equivalent of those experienced in an auto crash(6). Long-term exposure to G-force is advised to leave athletes at increased risk of vertebral disc degeneration, therefore exposure ought to be monitored closely(7). This is commonplace in the sphere of cccupational health and safety, where machinery operators have limitations on time exposed to vibrational forces to minimise permanent harm.
Assessing The Neck
In all sporting surroundings, basic neck Strength and range should be assessed to provide baselines, and also to help return to game planning — exactly as we’d use following any other peripheral joint harm. Cervical movement and musculature is Complex (see Figure 1), with endothelial levels leading to varying degrees of overall neck motion. The change of orientation of the cervical vertebral tissues of the mid to lower cervical spine allow for rotation, flexion and extension. However, this also isolates lateral flexion into the upper portion of the cervical spine. When deciding baseline array of movement it is important to recognize that this generally decreases with age therefore ‘normal’ range will vary between tutors and is likely to change within an athlete’s career.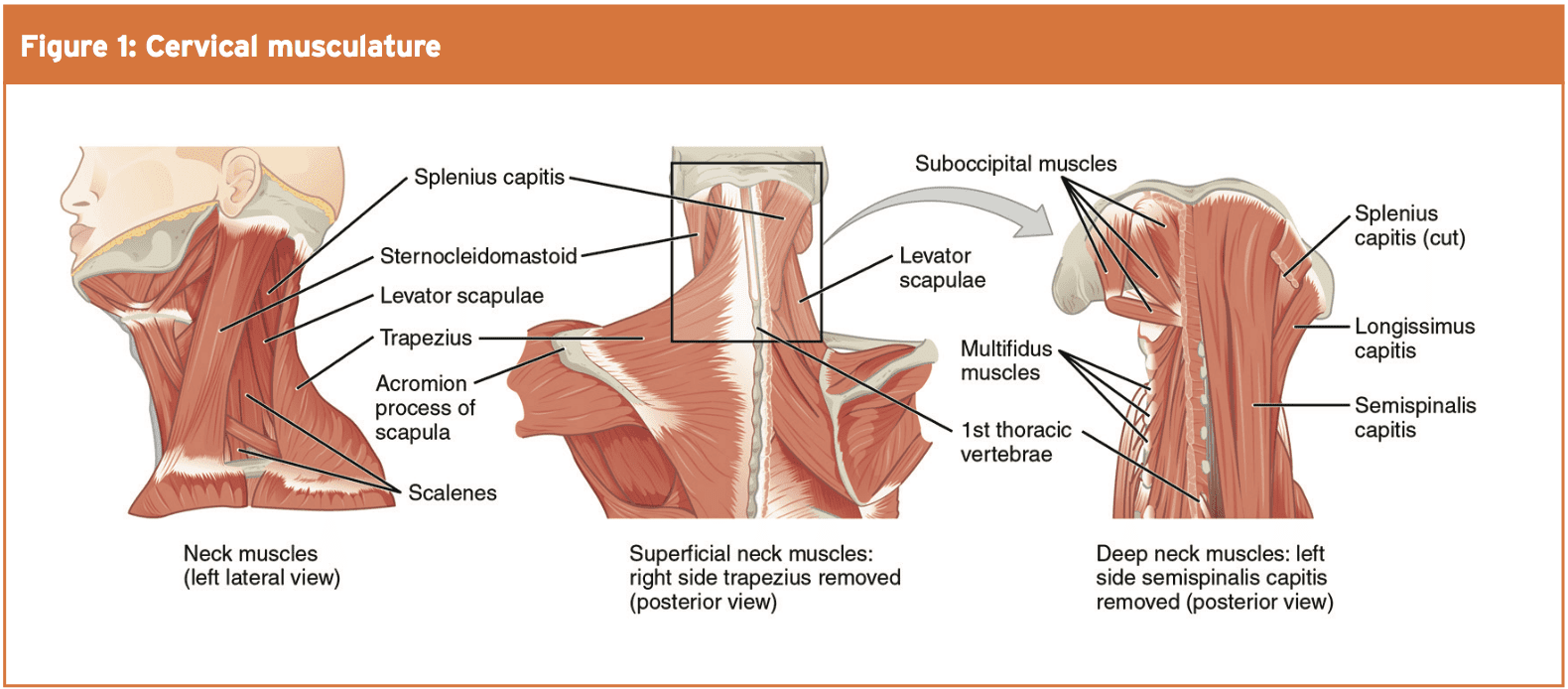
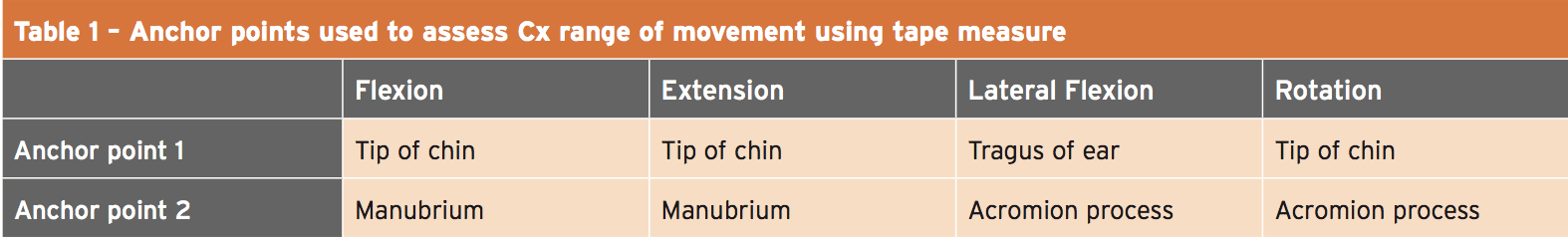
Cervical assortment of movement is radiological examination; however due to cost, this is technique is unlikely to be feasible in the sporting environment. Many clinicians commonly ‘eyeball’ neck motion, but there are in fact a number of more reliable and affordable tools that can be used and raise intra-rater reliability. (see Table 1)
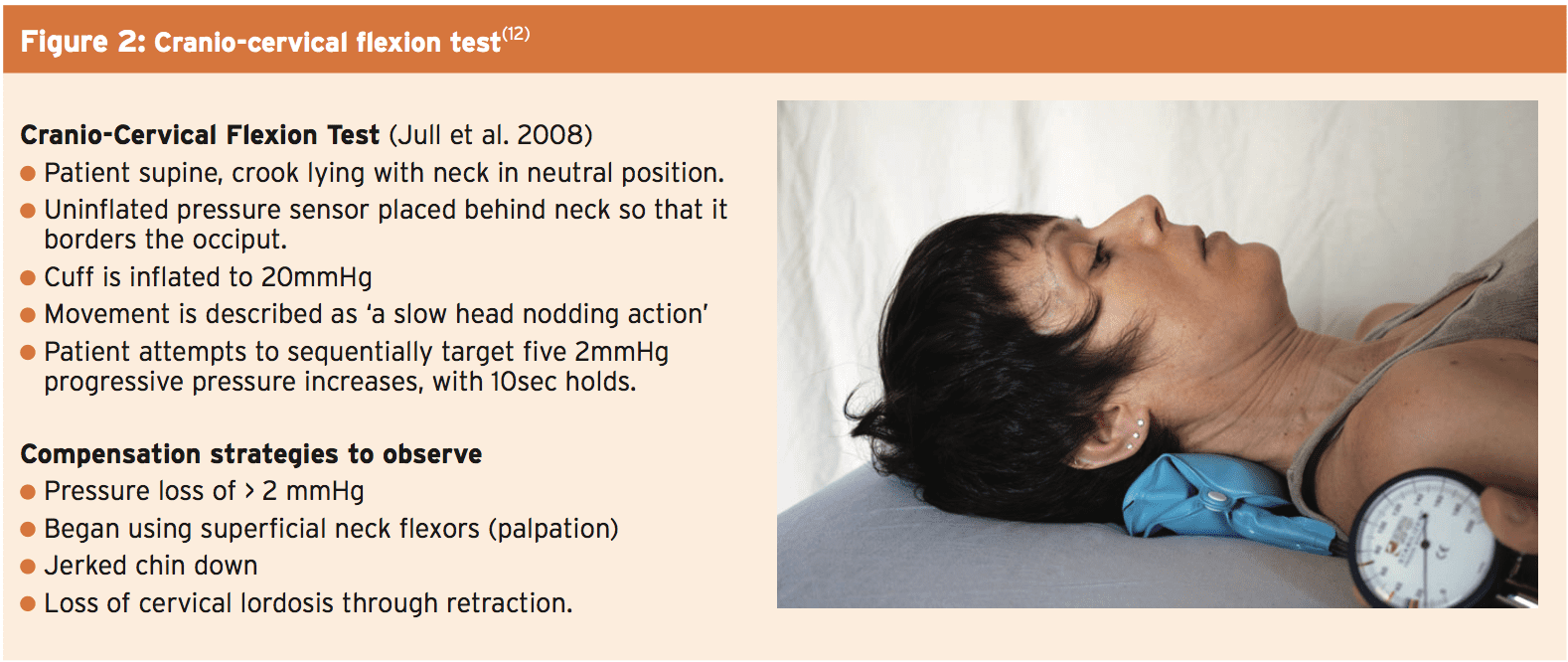
The primary stabilizers of the neck are Collectively known as the deep neck flexors (DNFs — longus capitus, longus colli, rectus capitis anterior and rectus capitis lateralis(8). The most frequent assessment used to measure the activation and endurance of this DNFs is that the craniocervical flexion test and evaluated with a biofeedback device (see Figure 2). This evaluation is a useful baseline assessment, and can recognize weakness and movement control dysfunctions. One drawback nevertheless is that it lacks normalized data(9).
Research tells us that the action of this Stabilizers is considerably decreased and delayed in anyone with neck pain(10), and consequently this is an excellent starting point in most neck rehabilitation to regain stability. Postural examination is also a key part of neck assessment. The primary purpose of the neck would be to maximize head position and equivalent displacement of the weight of the mind (3-6kg) is vital in decreasing overload to the stabilizing muscles. Segarra et al describe a battery of dependable tests to aid assessment of cervical movement control dysfunctions such as neck function at four point kneeling and with upper limb movement(11).
Prime Movers
Assessed in several of ways including using isokinetic and isometric dynamometers, and could be used with measuring muscle activity utilizing EMG studies to increase validity. Cervical extension is stronger than flexion in general population studies, while lateral side flexion is often coupled with extension using a bias to the subject’s dominant side. In athletes that rely on a dominant side bias (eg racquet and throwing sports) for operation gain, this asymmetry should be recognized but not always be viewed as damaging. In the athletic surroundings without Access to isokinetic and EMG gear, baseline strength could be set with a handheld dynamometer, ideally attached to minimize assessor bias. Decisions on which ranges should be tested should remain consistent and adapt for sport certain positions if required.To make sure the information is normalized the following considerations should be made:
- Torso stabilized
- Minimized lower limb involvement (eg Feet on wobble pillow)
- Establish ideal ranges which strength will Be measured at/through
- Standardized warm up and testing protocols
Neck Injuries & Concussion
Clinicians should have a high amount of It follows from this neck assessment ought to be performed in all athletes after concussion or head trauma. As study into concussion grows there is more focus on the association together with neck strength. Collins et al concluded that neck strength was a significant predictor of concussion amongst a large sample of high school athletes and although further research is needed, revealed positive outcomes in reducing concussion danger from adopting neck strengthening applications(14).Summary
Cervical injuries can occur in a range of Sporting environments in the end result of Serious injury through axial loading, Prolonged place exposure, whiplash and External forces such as vibrations and G forces. All cervical assessments need to rule out severe spinal injury and concussion, And also include range of movement Consideration also needs to be made for the Remainder of the kinetic chain — in particular the Shoulder girdle — due the high correlation Involving dysfunctions of the 2 areas.References
1. Current Review Musculoskeletal Medicine 2008. 1(3-4) 175 – 179
2. Clinical Sports Medicine 2003. 22 (427-443)
3. Clinical Sports Medicine 2003. 21:493–500
4. British Journal of Sports Medicine 2012 46(9):662-663
5. Aviat Space Environ Med 2005. 76:496–500
6. Int J Sports Physiol Perform. 2015. Sep;10(6):681-6
7. Aviat Space Environ Med 2013. 84:734–8
8. Physical Therapy 2005. 85:1349-1355
9. Physiotherapy Research Int 2010. 15; 144-149
10. Spine 2004. 29(19):2108-14
11. Manual Therapy 2015. 20: 570-579
12. J Manip Physiol Ther 2008. 31:525-533
13. Journal of Orthopaedic & Sports Physical Therapy 2012. 42(6):552-558
14. Journal of Primary Prevention 2014. 35: 309-319




