A lady in her early 30s recently came to see me complaining of a stone in her shoe. At first I proceeded to check that the sign in the window hadn't changed to say cobbler, instead of physiotherapist! I returned, rather relieved to observe that a waiting room filled with individuals with orthopedic ailments, but confounded with this very strange complaint from Karen the runner. I had to hear more. Chiropractic injury specialist, Dr. Alexander Jimenez examines the case.
Karen went on to detail a three-month history of pain between her second and third metatarsals. It started for no apparent reason. She had been running quite a little down the mountains of northern England, but this was nothing unusual for her and she'd never previously had issues. She could not pinpoint any other changes except one -- she was practicing her bridal dance with Paul, her fiancé. They wanted to dance salsa, also Karen admitted to a particular weakness for high-heeled dance shoes. Right, I thought possibly there was a loading along with a footwear issue here. By this stage, I was beginning to feel less anxious about the possibility of being expected to resole all of her shoes.
Further questioning revealed that Karen's pain had a burning quality that had first started coming on after about an hour of either running or dance but was now appearing within about 10 minutes of her wearing any kind of shoe that wasn't completely flat. She was not sure, but she felt that it had begun to hurt between her third and forth toes as well. These clues were leading me down the route of considering a nerve (nerve) element for her pain, especially when she clarified a „weird tingling somewhere in my feet . It appeared to be worsening both in intensity, distribution and irritability. She was otherwise in excellent health.
Evaluation proved tricky as Karen's foot wasn't debilitating the morning she came in to visit me and nothing I could do could reproduce her symptoms, much to her dismay and my disappointment. She was my very first appointment of the day. So I asked her to go home, pick up her heels and wear them that day and come back to see me after work, when (hopefully) her symptoms might resurface.
As it was, Karen hobbled in at 6pm. She had decided to make sure her foot hurt by wearing the offending Manolo Blahniks all day and going for a run at lunchtime. Suffice to say, this made my job a lot easier and she received a gold star for being such a dedicated patient!
Evaluation this time revealed that her pain was replicated by doing a heel raise -- a manouver which induced her to keep weight through extended metatarso- phalangeal (MTP) joints. As soon as I palpated the plantar part of her foot at the second and third interdigital spaces (between second to third and third to fourth toes), she jumped with her familiar pain, which now extended into her feet. I was able neither to palpate any unusual lumps nor elicit a click (called Mulder's sign) when I squeezed the metatarsal heads. This can sometimes happen if there's nerve swelling and also a proliferation of scar tissue adjacent to the metatarsal heads.
If the pain had still been hard to localize, I would have considered referring Karen to a sports doctor for them to inject a local anesthetic within the interdigital area to see whether this could relieve her pain, albeit for a brief period. As it was, this measure was not necessary as Karen managed to pinpoint exactly the space between her third and fourth metatarsals, only distal to her fourth MTP joint. She was also experiencing pain at the second interdigital space, although this was less intense.
I was fairly comfortable at this stage with the identification of interdigital neuroma, more commonly called Morton's metatarsalgia. I did want some plain-film X-rays to show me what state the MTP joints were in, however. I asked Karen to avoid running, dance only in flat shoes and to plunge her feet in ice water for 10 to 20 minutes a couple of times every day. And I asked her to see her GP with a view to getting a prescription for some anti- inflammatory medications.
I made her some temporary metatarsal load reliefs from podiatry felt and put these in her shoes. These are meant to distribute the weight-bearing load across all her MTP joints, but not only the irritated ones. She was due to see me in three days, ideally with her X-rays and at less pain. This also gave me three days to refresh my memory on your foot's neural anatomy!
Forefoot Anatomy
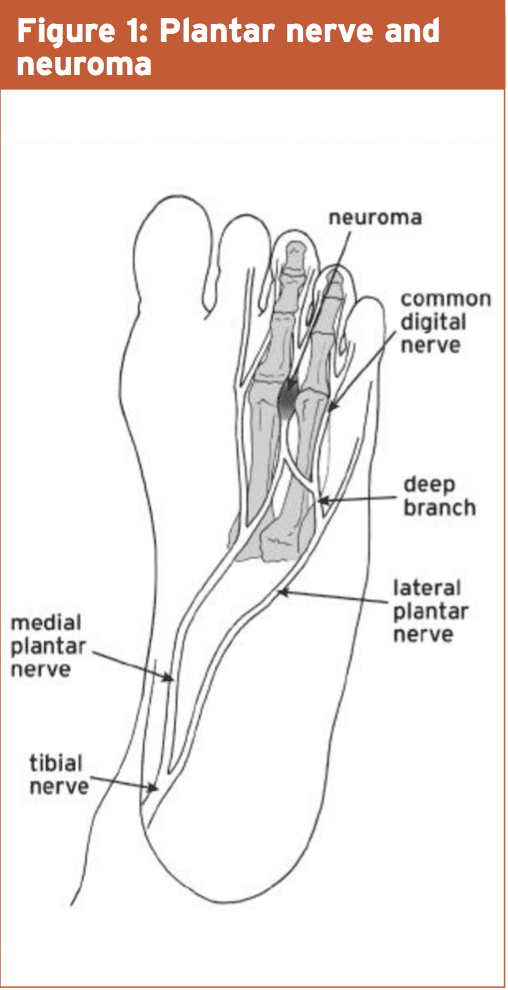
The posterior tibial nerve courses down the medial aspect of the tibia. Just about at the talocalcaneal joint or in the tarsal tunnel, just above the tip of the medial malleolus, the nerve divides into the medial and lateral plantar nerves. These then course their own ways through the plantar (underneath) surface of the foot, splitting several times to eventually form a network of interdigital nerves that provide sensation to the toes (see Fig 1, below). There is a huge degree of crossover of these nerves, making it often difficult to identify which one is causing the symptoms.
Causes Of Interdigital Neuritis
Although often referred to as a neuroma, Morton's metatarsalgia is not usually a true neuroma, but more of a chronic irritation of a nerve, characterized by intra-neural swelling and excessive extra-neural scar tissue formation. A true neuroma is actually a tumor, pathophysiologically different from that which we're dealing with in this example. Some ideas have been put forward regarding the origin of the problem. Some have stated it is the end result of poorly-fitting (usually too small) footwear compressing the interdigital space and all of its contents. Some say it's more to do with faulty biomechanics resulting in degeneration at the MTP joints and chronic synovitis. Others think injury is likely to be the main cause, leading to scarring and thickening of a damaged nerve sheath. Actually, the clinician will often find a combination of these issues.In Karen's case no joint degeneration showed up on X-ray, but there was a degree of laxity in her third MTP joint, leading to the suspicion of a plantar plate accident at some point in her past. Karen was a former dancer, so this was indeed a possibility. The plan of management we had decided upon appeared to have dampened her pain down significantly. She felt that the anti inflammatory medications were especially helpful, giving additional weight to the theory that the pathology was an active and inflammatory one, most likely kept by loading that the joints in expansion (as seen in high heels and just prior to push-off when running).
Management
Karen was especially keen to pursue conservative (non-surgical) options. The inflammation brought on by loading the loose MTP joint was further distending the joint, rendering it even less stable and more prone to inflammatory processes. Clearly the dual methods of loading and inflammation were perpetuating every other, thus we had to interrupt the cycle.Karen had to accept this, particularly in the short term, she'd have to take steps to decrease load through the third and second metatarsal joints. We also had to reduce the severe inflammation. Karen carried on together with the anti- inflammatory medications under the advice of her GP for another week and continued to ice her feet. She wore shoes with a wider toe box, allowing her transverse arch be under less strain. I left some metatarsal relief bars out of high-density, low-profile foam, placing these under the insoles of three pairs of her shoes. I put them slightly towards the heel of the metatarsal heads, which prevented the MTP joints in hyperextending.
I also did some manual treatment to ensure Karen' back and forefoot joints were suitably mobile and gave her some intrinsic muscle strengthening exercises. We were able to prevent the need for corticosteroid injections and surgery, although these choices were open to us if the conservative route failed.
Surgery could be aimed at excising built-up scar tissues and is often successful, but only if the underlying biomechanical problems are fixed. I saw Karen twice more over the following three weeks, during which time we could re-introduce her to running. This was initially on the flat after which she was slowly exposed to the increasing toe extension that operating on hills demands. She weaned herself off her meds, but would prophylactically take a few as she returned to dancing salsa. She'd need to take wearing marginally lower heels as a result of her symptoms, but said she'd prefer this compromise to having to hobble around for the remainder of her life with a pebble stuck in the sole of her foot!