Spinal meningitis does not just affect the brain. Most think of meningitis as a brain disease, but it can also affect the spine. We will discuss learning how to recognize it and find the right treatment to fix it within the spinal cord. Spinal meningitis can be a potentially deadly infection of the meninges. This is the protective tissue that covers the brain and spinal cord.
It can be caused by viruses, bacteria, or fungi that are transmitted from person to person by sneezing, talking, and sharing food. Viruses and pathogens that cause other infections, like the mumps and measles, can also cause meningitis. The lining around the brain and the spine are connected, which means that infection can travel from one area to another, or remain in the brain or the spine.
The Meninges
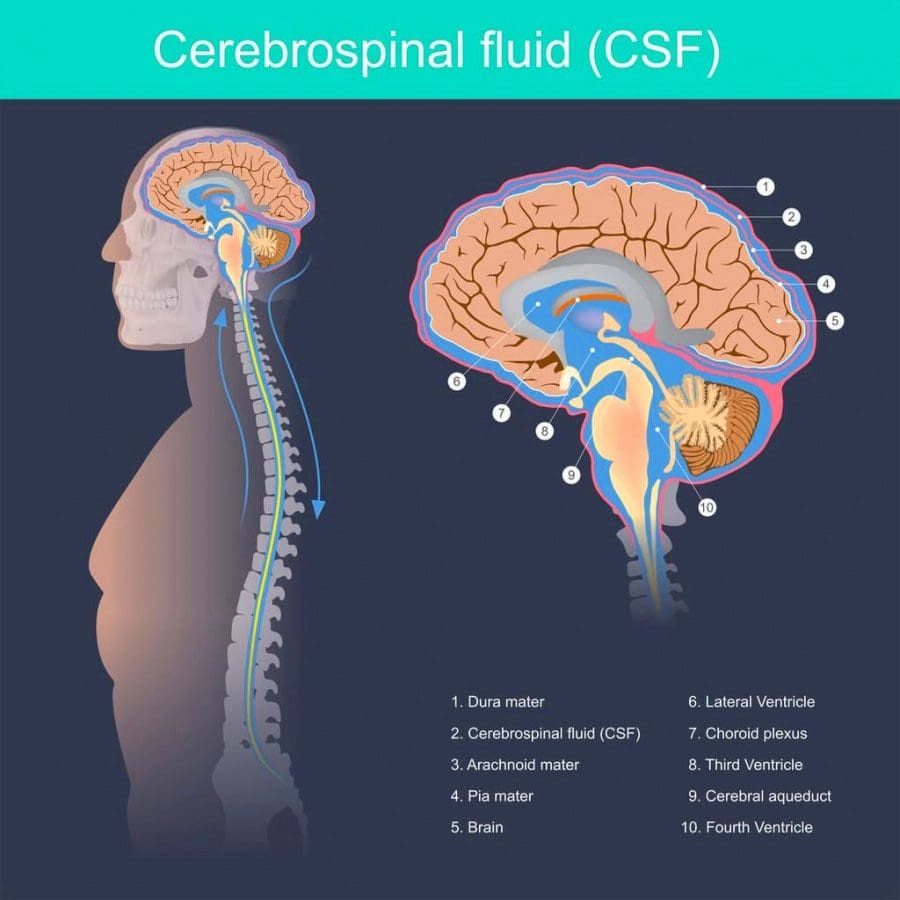
Meninges are the protective membranes that surround the brain and spinal cord. They are made up of three layers:
- Dura mater is the thick and tough outer layer
- Arachnoid mater is the middle layer made up of strands of connective tissue
- Pia mater is the inner layer of cells
Spinal meningitis can develop when a virus, bacteria, or pathogen invade the meninges layers. This causes the immune system to react trying to remove the invading bacteria etc, which causes inflammation. These organisms usually take up residence in the nose and throat and never cause problems. Most individuals that come into contact with these viruses never get sick.
The reason for this is because the body produces fighting antibodies before the pathogens can invade the meninges. Others, possibly from age or underlying conditions, where they are not able to produce enough or any antibodies, makes them vulnerable to the illness. When the brain and spine's tissue/s get infected with any one of these pathogens, the tissue swells, which constricts proper blood flow to the brain.
Types of Spinal Meningitis
The most common types of spinal meningitis in the United States include:
Viral meningitis
Viral meningitis is caused by enteroviruses, which are common viruses that enter the body through the mouth and travel to the brain and tissues where multiplication ensues. There are other viruses that can also cause meningitis. These include:
- Viruses that cause mumps
- Herpesviruses - like Epstein-Barr, measles, influenza, West Nile
- Lymphocytic choriomeningitis virus from rodents
Any of these viruses can spread to the meninges, causing spinal meningitis to develop. This is a less severe type than bacterial meningitis.
Bacterial meningitis
This is the type where dangerous bacteria invade the meninges. Individuals are at higher risk as this type can be fatal if not treated. Common types of bacterial meningitis include:
- Haemophilus influenzae - can cause severe infection/s of the lining of the brain, spinal cord, and the blood.
- Pneumococcal meningitis - is caused by the bacterium Streptococcus pneumonia and is the most common form of bacterial meningitis.
- Meningococcal meningitis - also known as meningococcal disease, is a less common type. This type is caused by the bacterium Neisseria meningitides. Around 2,600 people in the U.S. are affected yearly.
Symptoms
Viral or bacterial spinal meningitis can cause a range of symptoms, including:
- Neck and back stiffness
- Muscle weakness
- Headache
- Drowsiness
- Fatigue
- Fever
- Double vision
- Sensitivity to light
- Nausea
- Vomiting
- Hearing difficulty
- Confusion
- Seizures
- Rash
Symptoms are often far more pronounced with the bacterial form. This is because it’s associated with more inflammation, compared to the viral type.
Complications
Depending on the type whether viral or bacterial the results can be serious, leading to:
- Permanent brain damage
- Permanent organ damage
- Stroke
- Loss of hearing
- Loss of limbs
- Death
Anyone who experiences symptoms of meningitis should see a doctor immediately for diagnosis and treatment options.
The risk for Spinal Meningitis
Getting spinal meningitis depends on various factors like:
- Age
- Immune system status
- If the individual lives in a group environment
- Children younger than five
- Individuals with weakened immune systems from taking medication/s for other conditions
- Recent organ/bone marrow transplants
- Babies younger than 1-month-old along with weakened immune systems are more likely to experience severe illness
These are factors that could increase the risk of viral meningitis. Fortunately, most cases are not serious and in children's cases, most recover in one to two weeks. Meningitis can also occur very rarely after spine surgery where the lining around the dura is torn with an infection happening at the same time.
Diagnosis
Detecting spinal meningitis a doctor will utilize:
- Blood tests
- Imaging tests
- Spinal tap to test the cerebrospinal fluid which surrounds the brain and spinal cord.
- The fluid is collected and sent to a lab, where it is analyzed for bacteria or viruses.
Treatment
Antiviral medication can help with certain types of viral meningitis with other meds for treating meningitis symptoms. Doctors recommend bed rest, proper fluids, and medication for fever relief and headache relief. This is for viral meningitis.
Antibiotic medications can treat bacterial spinal meningitis. It is commonly treated with intravenous antibiotics in a hospital setting. Unfortunately, around ten percent of children with bacterial meningitis die from it yearly. Even with immediate antibiotic treatment a child's body can become overwhelmed by the bacteria/organism. The Meningococcus bacteria can create a toxin that invades the blood. This can be fatal for a child or adolescent within hours. This is why it’s highly recommended to prevent bacterial meningitis than to treat it once it's active.
Contagious
Proper hygiene like hand washing, not sharing food, beverages, utensils, or body care products like lip salve/balm can help stop the spread of bacterial and viral meningitis.
Chiropractors On Metabolic Syndrome & Inflammation
Dr. Alex Jimenez’s Blog Post Disclaimer
The scope of our information is limited to chiropractic, musculoskeletal, physical medicines, wellness, and sensitive health issues and/or functional medicine articles, topics, and discussions. We use functional health & wellness protocols to treat and support care for injuries or disorders of the musculoskeletal system. Our posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate and support directly or indirectly our clinical scope of practice.*
Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. We understand that we cover matters that require an additional explanation as to how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. The provider(s) Licensed in Texas& New Mexico*