Discitis is typically caused by an infection that grows in one of the spine’s vertebral bones and possibly in the intervertebral discs. Discitis is usually a bacterial infection, but it can be viral.
Discitis affects around 1 out of every 100,000 people. This means that it is not a common spinal disease. Discitis can occur in adults and children, however, it is more common in children.
- Discitis mostly occurs in the low back region of the spine
- Followed by the neck region
- Finally the middle-back region
It accompanies vertebral osteomyelitis. Both types of infections share many of the same symptoms/characteristics. Although these are uncommon conditions, they can produce severe symptoms affecting an individual's quality of life. This is why early diagnosis and treatment are essential.
Discitis Causes
There are two recognized causes of discitis. The rarest form comes from a prior surgical or diagnostic procedure. This usually happens when a needle or other tool/device transfers the infection. The other is the more common, and it is known as spontaneous discitis. Here the infection develops from a bacterial or viral organism that travels to the disc/s via the blood supply from another part of the body.
When an infection starts somewhere else and then travels to the disc, it is called transient bacteremia, which is bacteria in the bloodstream that has a short life. Ear infections along with skin infections are perfect examples of infections that can lead to transient bacteremia and discitis.
After a disc becomes infected, it can be quite difficult for the body to fight the infection. The disc/s are the largest avascular organs in the body, which means they do not have their own blood supply. The discs get their nutrition and blood supply, which includes the white blood cells for fighting infections, from the vertebral endplates.
Because the discs lack the resources to fight infections on their own, there is a struggle when trying to protect against infection. Because discitis is usually caused by an infection that developed in another area of the body, individuals with medical conditions are at a higher risk for developing discitis. These conditions include:
- Diabetes
- A.I.D.S
- Cancer
- Chronic kidney disease
Symptoms
Intense back pain that starts gradually is the distinctive characteristic symptom of discitis. The pain is usually localized to the area where the infection is located. This means that the pain doesn't radiate or spread out like other types of back pain conditions.
Diagnosis
A doctor, spine specialist, or chiropractor will review medical history and symptoms with the individual. A fever is normally not present once the infection is inside the disc, along with the white blood cell count being normal.
However, the erythrocyte sedimentation rate increases. This is a blood test that examines how fast red blood cells fall to the bottom of a tube. The faster that they fall to the bottom, the more likely there is inflammation somewhere in the body.
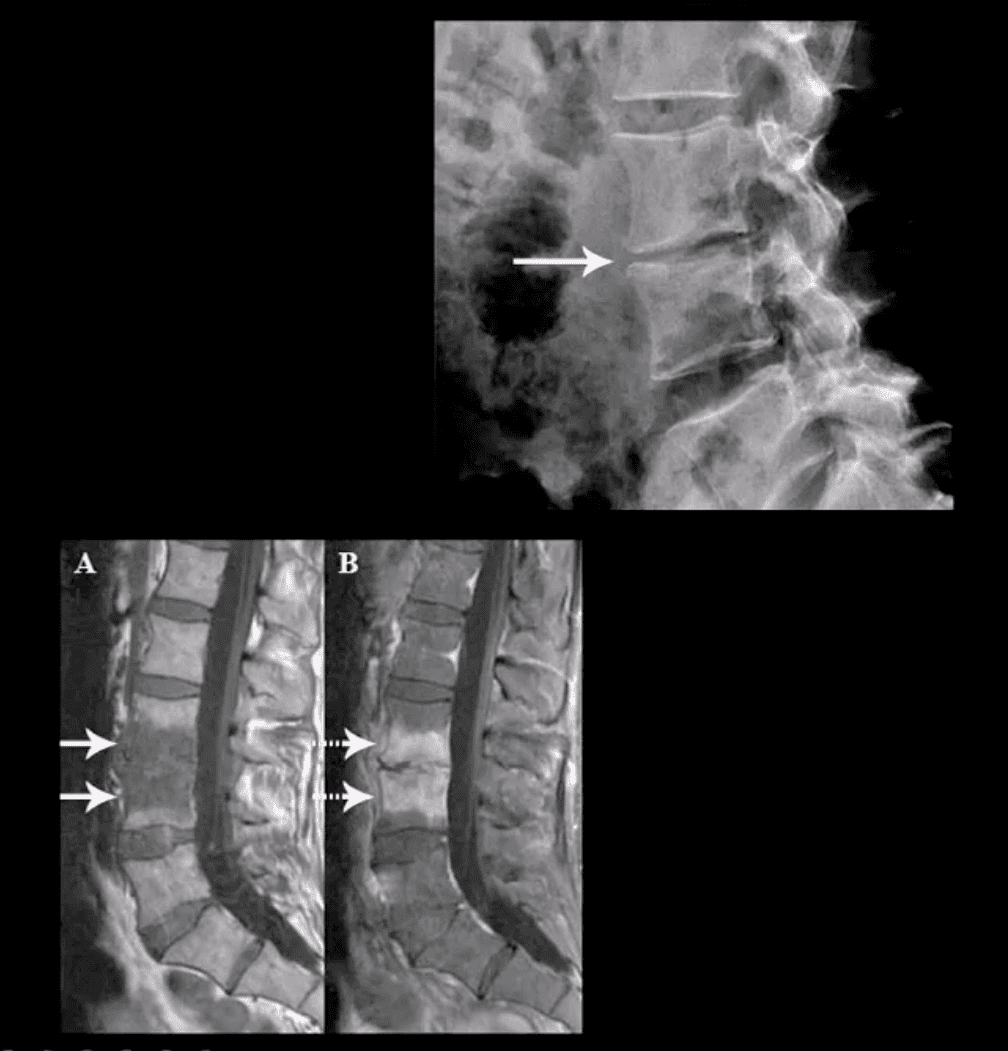
Blood tests can be utilized during diagnosis, however, the most accurate diagnostic tool to confirm discitis is magnetic resonance imaging or MRI that shows if an infection is present.
Treatment
Treatment can be challenging. This is because of the fact that the discs do not have a blood supply, and medications/antibiotics travel through the blood. It is treatable and is usually done within a six to eight-week course of antibiotics intravenously or through an IV.
IV administered antibiotics could require treatment on an outpatient basis. The entire course of antibiotics must be completed in its entirety in order to manage the discitis. A doctor could also prescribe a spinal brace to help stabilize the spine and reduce pain. A brace can limit movement, however, it will help ensure proper healing.
Spinal Infections
Spinal infections can present spontaneously or as secondary conditions, e.g. after a surgical procedure. Spinal infections can affect different structures, like the:
- Vertebral column or the bones of the spine
- Intervertebral disc space, which is the cushion-gel structures between the vertebrae
- Spinal canal
Here are some facts about the occurrence and prevalence of different infections of the spine:
- Vertebral osteomyelitis is the most common type of infection. It affects an estimated 27,000 to 66,000 people a year.
- Epidural abscess is an infection inside the spinal canal that affects up to two cases per 10,000 in hospital admissions around the U.S. It is pretty common in individuals with vertebral osteomyelitis or discitis. Eighteen percent of those individuals can develop this infection. However, it is more common in people fifty and older.
- Discitis, as aforementioned is a pretty uncommon condition. Although, treatment has advanced, around twenty percent of individuals with this infection do not survive.
Infection Risk Factors
There are certain factors that increase the risk of developing an infection. These factors include:
- Arthritis
- Diabetes
- Drug addiction
- Immunosuppression, which can come from Acquired Immunodeficiency Syndrome or medical treatment for tumors
- Malnutrition
- Obesity
- Organ transplant
- Recent urinary tract instrumentation
- Smoking
Symptoms and Diagnosis
Symptoms from a spinal infection can vary. However, continuous back pain with no history of trauma or injury. Usually, there is a delay in the diagnosis for an infection of the spine because of the:
- Subtle nature of the symptoms
- Individual's belief that the pain is not serious
- Absence of body-wide symptoms like a fever
Lab results can also complicate the diagnostic process, as they can be misleading. There could be normal white blood cell counts, x-rays that show no abnormalities, and a sensitive diagnostic test like a bone scan might not show that an individual is positive until a week later.
An erythrocyte sedimentation rate is a valuable screening test when it comes to spinal infections. The test can measure inflammation and infection in the body. If a spinal infection is suspected, an MRI could be the most reliable tool to confirm early diagnosis.
Health & Immunity Series
NCBI Resources
Dr. Alex Jimenez’s Blog Post Disclaimer
The scope of our information is limited to chiropractic, musculoskeletal, physical medicines, wellness, and sensitive health issues and/or functional medicine articles, topics, and discussions. We use functional health & wellness protocols to treat and support care for injuries or disorders of the musculoskeletal system. Our posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate and support directly or indirectly our clinical scope of practice.*
Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. We understand that we cover matters that require an additional explanation as to how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. The provider(s) Licensed in Texas& New Mexico