Tailbone pain begins in the coccyx, which is located at the bottom of the spine's sacrum.
Coccydynia (kŏk′sĭ-dĭn′ē-ə) is the term for pain in the coccyx, or tailbone.
Sitting and leaning back could be very uncomfortable.
However, pretty much everybody responds well to conservative treatment.
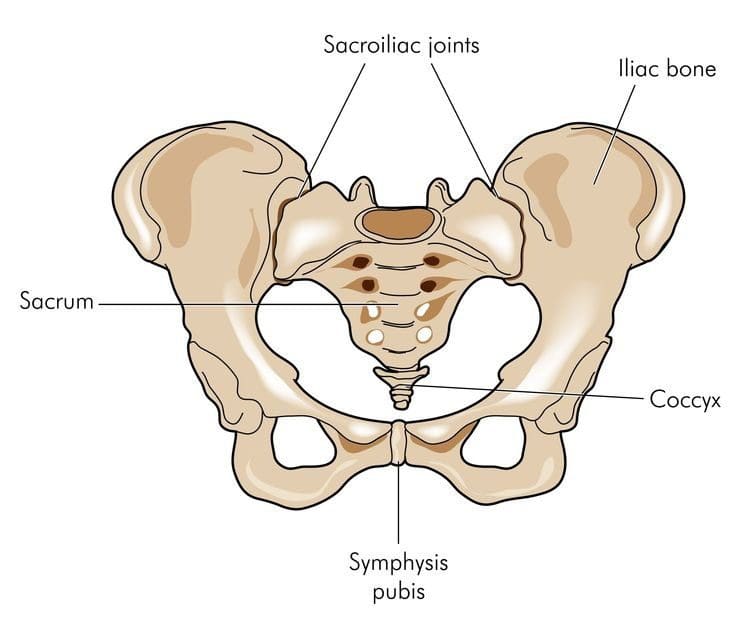
Spinal Anatomy of the Coccyx
The coccyx, or tailbone, is the lowest area of the spine. It sits right below the sacrum.The tailbone is made up of 3 to 5 small bones fused together by around age 30.
The coccyx helps support our weight while sitting.
Risk Factors
The prevalence of coccydynia is still unknown, but medical research has found that the condition affects:- Adolescents
- Adults
- Women
- People that are overweight
Women are affected five times more than men, which is likely due to injuries from childbirth.
Also, a woman's coccyx is farther back than the male counterpart. This makes it more vulnerable to trauma.
Obesity causes coccydynia because of the extra weight/pressure on the coccyx, which alters how a person sits.
Causes
There are several causes, the most common are:Trauma from:
- Falling
- Getting bumped/hit
- Bike riding
- Rowing
Activities like these can bruise, break, and even dislocate the tailbone.
If this happens there could be painful inflammation and muscle spasms in the tailbone area.
Other possible causes:
Bone spurs: A small bone spur on the lowest part of the coccyx can pinch the surrounding area, and cause pain and discomfort while sitting.Joint instability: Sacrococcygeal joint (which connects the coccyx and sacrum) allows too much or too little movement.
- Osteoarthritis
- Infection
- Metastatic cancer
- Chordomas
- Arachnoiditis
- Lower back pain
- Sciatica
- Infection
- Pilonidal cysts (skin infection)
- Fractured bone
Diagnosing
A doctor utilizes medical history and physical exam to diagnose coccydynia.Imaging scans are usually not necessary, but a doctor may order:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
- Bone
- Nerve
- Tissue
Medical history is important, a doctor wants to know if a
- Fall
- Accident
- Recent trauma
A physical exam is next in line along with symptoms.
The pain is usually localized in the tailbone, making it straightforward to diagnose.
A doctor will want to know if the pain strikes when sitting or leaning back and which is worse.
A doctor might ask the patient to point to where they're feeling the pain.
Pointing could be enough for the doctor to tell if the pain is coccydynia when compared to other low back pain conditions.
The doctor will want to palpate the tailbone area for signs of inflammation.
Non-surgical Treatment
Conservative treatment is extremely effective for coccydynia.Ninety percent of people experience pain reduction using non-surgical means or any medical intervention.
It is first treated with noninvasive methods:
- Ice or heating pad can help provide immediate, short-term relief.
- Donut/Wedge cushion provides extra padding taking the pressure off the coccyx when sitting. These cushions are available at pharmacies.
- Avoid sitting for long times, like a long flight will help prevent additional pain and injury.
- Rest is very important to help avoid further injury during recovery.
If the medication doesn't work then a doctor may try cortisone injection or local spine blocker to send strong medicine directly to the tailbone area.
Surgical Procedure
If none of the conservative treatments work then surgery could be the next step.The procedure is called a coccygectomy, which means the removal of the tailbone.
A surgeon will discuss the procedure in great detail before it is performed.
These risks include:
- Infection
- Hematoma (abnormal collection of blood outside an artery or vein)
- Perineal hernia (weakened pelvic muscles)
Chronic Coccydynia
A small portion of people can develop chronic coccydynia, which means the pain lasts for more than 2 months.Chronic coccydynia can take a major toll on the quality of life. Talk to a doctor if symptoms are not resolving.
They may refer you to a doctor that specializes in coccydynia management.
Protecting the Tailbone
There is no exact way or method to prevent coccydynia.However, reducing the risk of tailbone pain can be achieved by using caution when participating in sports like:
- Skating - Ice, Inline, and Roller
- Biking
- Horseback riding
Severe Back Pain Chiropractic Treatment El Paso, TX
Gale Grijalva suffered from severe back pain as a result of an automobile accident injury. Where it was once very difficult to go about her regular daily tasks, Gale Grijalva is now able to participate in physical activities she wasn't able to engage in before thanks to Dr. Alex Jimenez, a chiropractor in El Paso, TX. Gale Grijalva describes how patient Dr. Jimenez is and she discusses how thoroughly he's been able to help her, including answering any concerns she may have. Gale Grijalva also experienced results through rehabilitation.
Severe chronic back pain is a serious, recurring condition that affects a person's everyday life. Back pain lasting over three months is considered chronic. The spine is an essential component of the body. Severe chronic back pain might be the backbone's manner of telling the body that there is an issue. The spine is composed of bony vertebrae, soft spinal discs, facet joints, tendons, ligaments, and tendons. Within the bony vertebral artery lies the spinal cord, the delicate but effective nerve pathway of the central nervous system.
NCBI Resources
Before you run screaming in horror to the medicine cabinet, one of the best reasons to participate in chiropractic treatment is that it helps reduce the chance of a recurrence. By working on the total body and getting it in the best shape possible, the patient is stronger and more balanced to handle their workload and other strenuous activities. Chiropractors also impart advice on how to minimize the chances of re-aggravating the lower back.Millions of people suffer from back pain each year, and some never visit a chiropractor. Those who do choose chiropractic treatment are privy to treatment that reduces their pain, increases healing, shortens their downtime and lessens their chances of a recurrence. If over the counter medication and ice packs haven’t worked within a few days, it’s time to make an appointment for a consultation with a licensed chiropractor. You will be happy you did.