Sagittal Fluid Sensitivity
- Sagittal Fluid Sensitive MR slice showing large synovial popliteal (Baker's) cyst (above top image) and sizeable synovial effusion (above bottom image)
- Note multiple patchy dark signal areas on both images, representing fibrinoid inflammatory deposits aka "rice bodies" a characteristic MRI feature of RA
Management Rheumatological Referral & DMARM
- Conservative management followed by operative care in complicated cases of tendon ruptures and joints dislocations
- Supplemental reading:
- Diagnosis and Management of Rheumatoid Arthritis - AAFP
- https://www.aafp.org/afp/2011/1201/p1245.html
Septic Arthritis (SA)
- Septic arthritis - d/t bacterial or fungal contamination of the joint. SA may cause rapid joint destruction and requires prompt Dx and antibiotic administration
- Joints affected: large joints with rich blood supply (knee 50%>hips>shoulders).
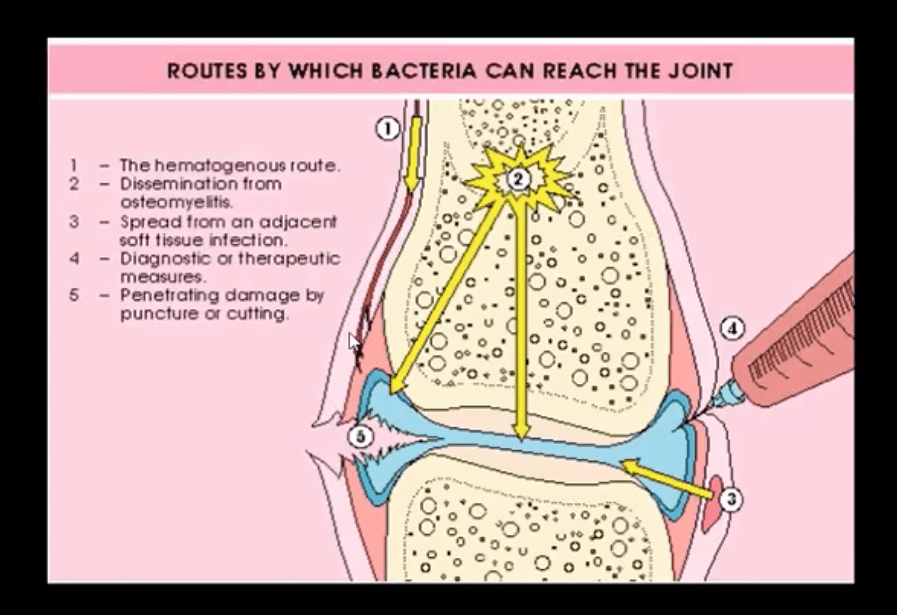
- Routs of Infection:
- 1) Hematogenous is m/c
- 2) Spread from an adjacent site
- 3) Direct implantation (e.g., trauma, iatrogenically)
- Patients at risk: children, diabetics, immunocompromised, pre-existing joint damage/inflammation, e.g., RA, etc.
- I.V. drug users are particularly at risk and also may contaminate atypical joints "the S joints" SIJ, SCJ, Symphysis pubis, ACJ, etc.
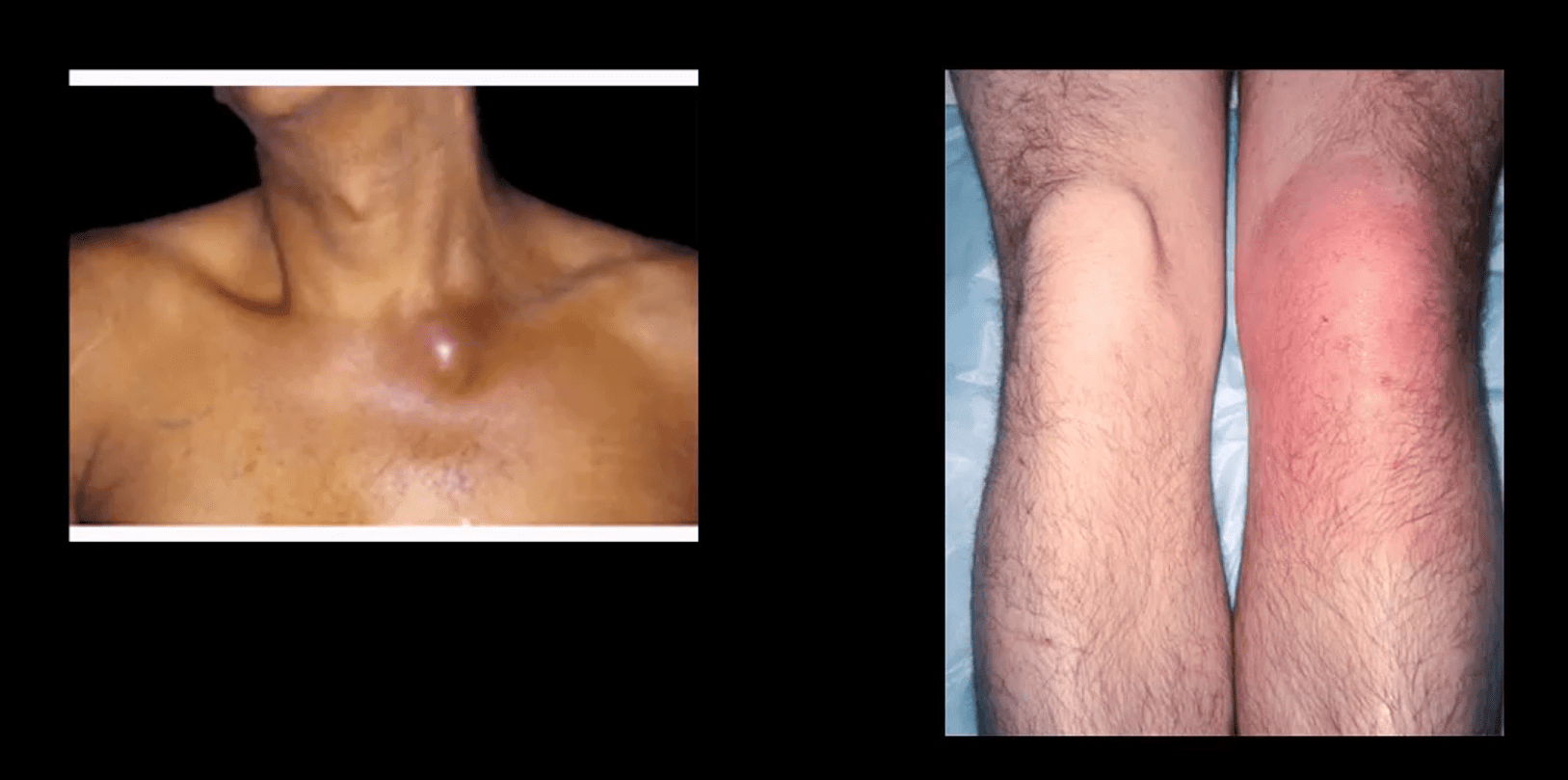
- Clinically: may vary and depends on host immune response and bacterial virulence. May present with rapid onset or exacerbation of pre-existing joint pain, swelling, limitation of ROM. General signs of malaise, fever, fatigue and elevated ESR, CRP, Leucocytosis may be present.
- N.B. Diabetics and immunocompromised may present with fewer manifestations and lack of fever d/t declining immune response
- Dx: clinical, radiological and laboratory. Arthrocentesis may be necessary for culture, cell count and purulent synovial examination
- Management: I.V. antibiotics
- Imaging Dx: begins with radiography but in the early stage most likely will be unremarkable. MRI can be sensitive and help with early identification of joint effusion, bone edema, etc. US may be helpful in the superficial joints and in children. US helps with needle guidance. Bone scintigraphy may be used occasionally if MRI is contraindicated
Routes of Joint Contamination
- 1. Hematogenous (M/C)
- 2. Spread from the adjacent site
- 3. Direct inoculation
- M/C organism-Staph aureus
- N.B Gonococcal infection may be a top differential in some cases
- IV drug users: Pseudomonas, candida
- Sickle cell: Salmonella
- Animal (cats/dogs) bites: Pasteurella
- Occasionally fungal contamination may occur
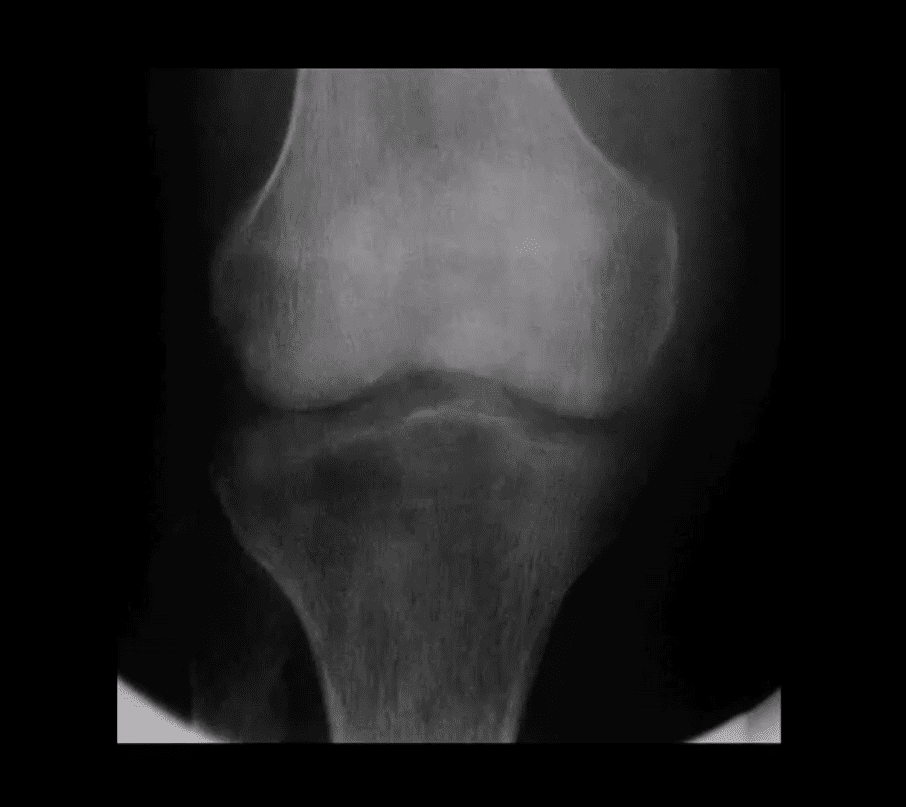
Radiography
- Initially non-specific ST/joint effusion, obscuration/distortion of fat planes. Because it takes 30% of compact and 50-75% trabecular bone to be destroyed before seen on x-rays, radiography is insensitive to some of the early changes. MR imaging is the preferred modality
- If MRI is not available or contraindicated. Bone scintigraphy with Tc-99 MDT can help
- In children, US preferred to avoid ionizing radiation. In children, US can be more sensitive than in adults due to lack of bone maturation
Radiographic Dx
- Early findings are unrewarding. Early features may include joint widening d/t effusion. Soft tissue swelling and obscuration/displacement of fat planes
- 1-2 weeks: periarticular and adjacent osseous changes manifesting as patchy demineralization, moth-eaten, permeating bone destruction, loss, and indistinctness of the epiphyseal "white cortical line" with an increase in soft tissue swelling. MRI may be helpful with early Dx.
- Late features: complete joint destruction and ankyloses
- N.B. Septic arthritis may progress rapidly within days and requires early I.V. antibiotic to prevent major joint destruction
T1 & T2 Knee MRI
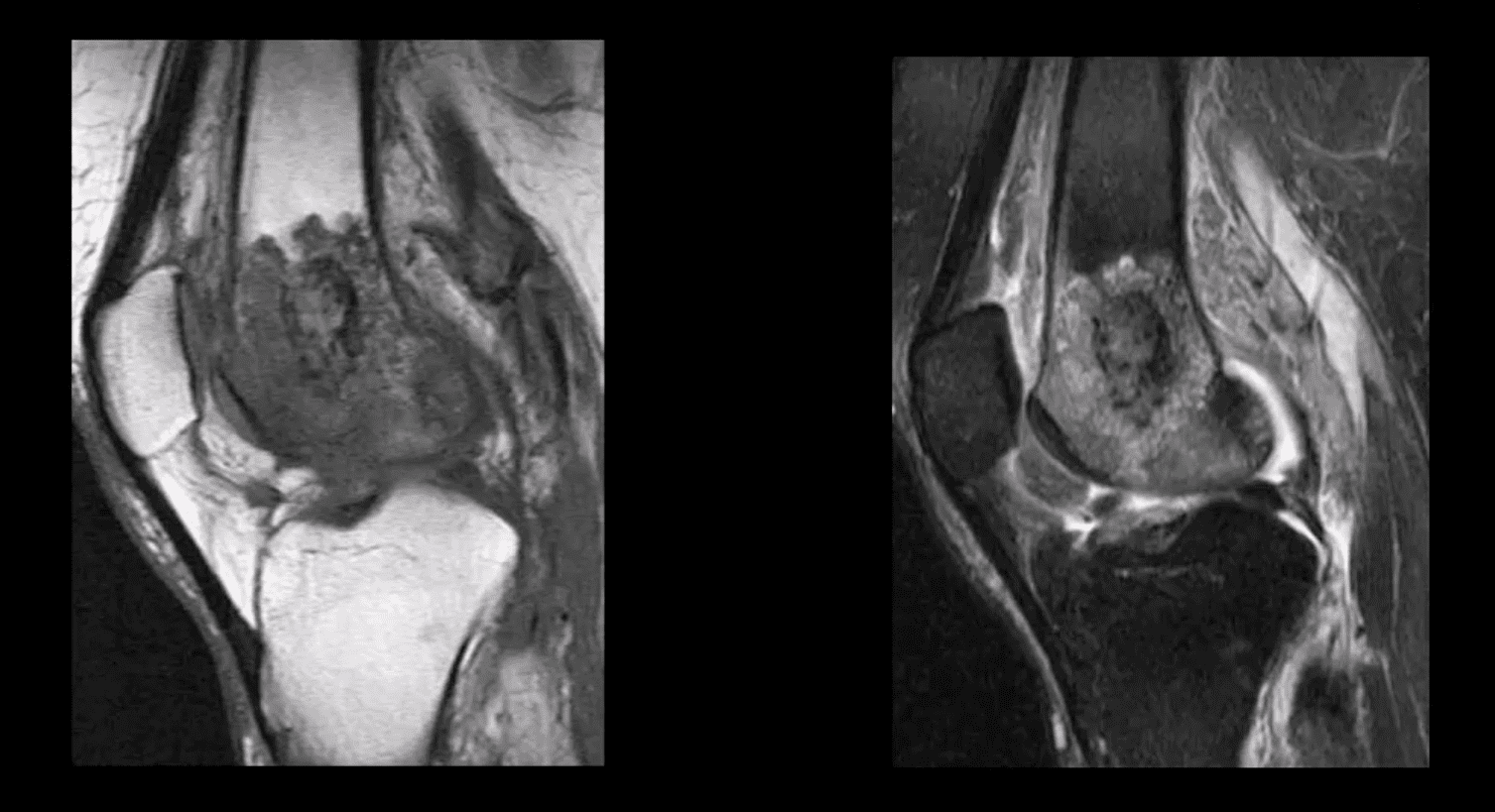
- T1 (above left) and T2 fat-sat sagittal knee MRI slices reveal loss of normal marrow signal on T1 and increase on T2 due to septic edema. Bone sequestrum d/t osteomyelitis progressing into septic arthritis is noted. Marked joint effusion with adjacent soft tissue edema is seen. Dx: OSM and septic arthritis
- Imaging may help the Dx of the septic joint. However, the final Dx is based on Hx, physical examination, blood tests and most importantly synovial aspiration (arthrocentesis)
- Synovial fluid should be sent for Gram staining, culture, glucose testing, leukocyte count, and differential determination
- ESR/CRP may be elevated
- Synovial fluid: WBC can be 50,000-60,000/ul, with 80% neutrophils with depleted glucose levels Gram stain: in 75% gram-positive cocci. Gram staining is less sensitive in gonococcal infection with only 25% of cultures +
- In 9% of cases, blood cultures are the only source of pathogen identification and should be obtained before antibiotic treatment
- Articles: https://www.aafp.org/afp/2011/0915/p653.html
- https://www.aafp.org/afp/2016/1115/p810.html
Crystal-Induced Knee Arthritis
- Crystalline arthritis: a group of arthropathies resulting from crystal deposition in and around the joint.
- 2-m/c: Monosodium urate crystals (MSU) and Calcium Pyrophosphate Dehydrate crystals (CPPD) arthropathy
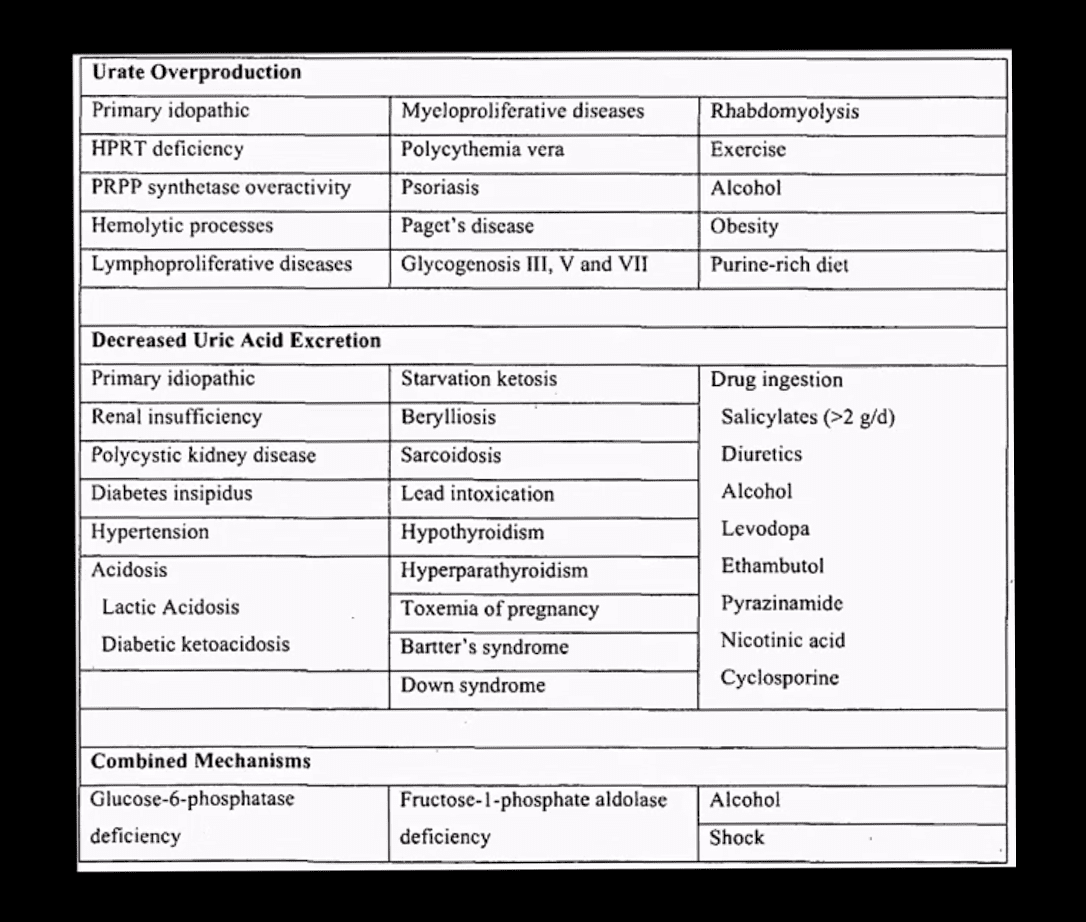
- Gout: MSU deposition in and around joints and soft tissues. Elevated levels of serum uric acid (UA) (>7mg/dL) caused by overproduction or under-excretion of uric acid
- Once UA reached/exceeded 7mg/dL, it will deposit in the peripheral tissues. Primary gout: disturbed metabolism of nucleic acids and purines break down. Secondary gout: increased cell turnover: Psoriasis, leukemia, multiple myeloma, hemolysis, chemotherapy, etc.
- Gout presents with 5-characteristic stages:
- 1)asymptomatic hyperuricemia (years/decades)
- acute attacks of gouty arthritis (waxes and wanes and lasts for several years)
- Interval phase between attacks
- Chronic tophaceous gout
- Gouty nephropathy
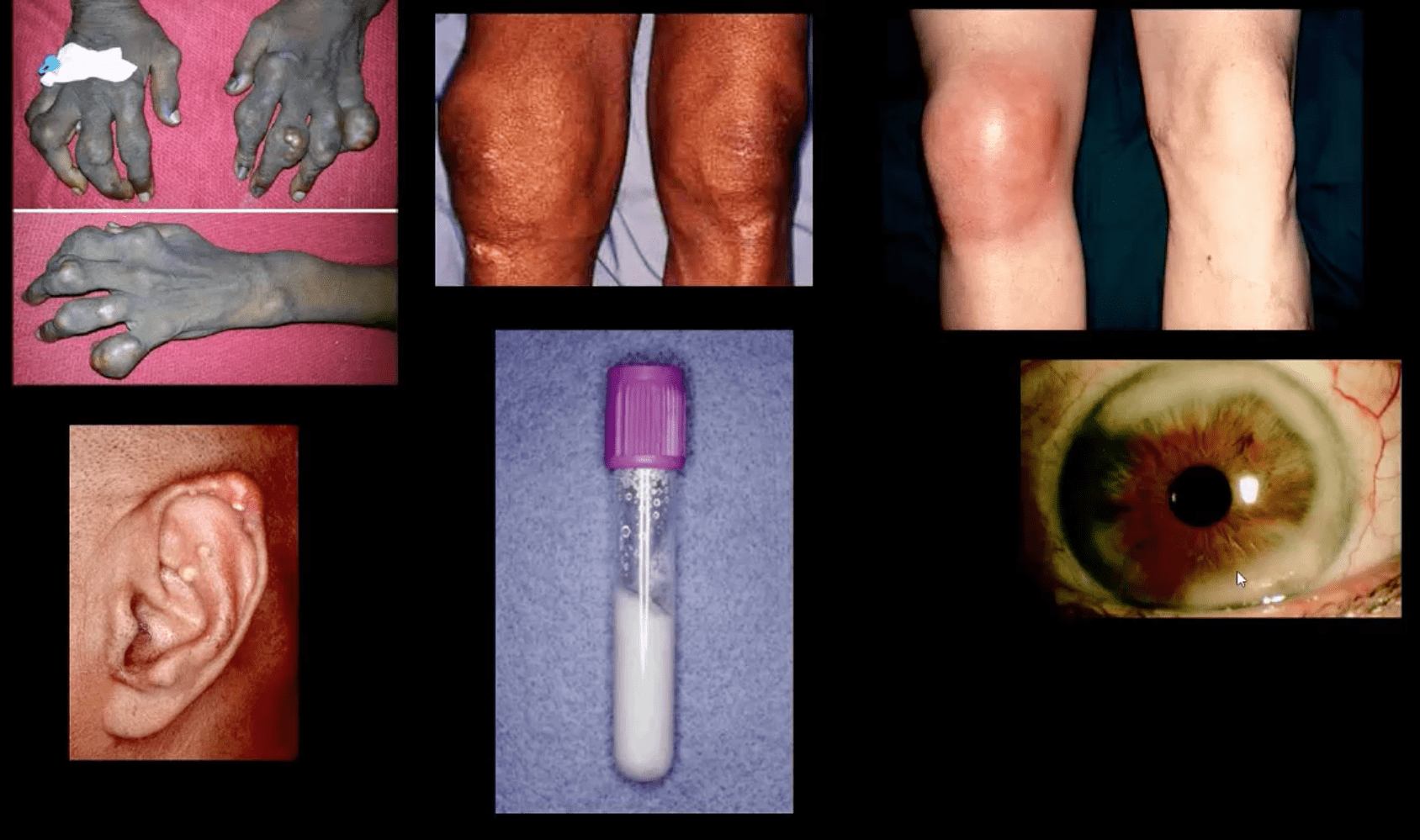
Clinical Presentation
- Depends on stages
- Acute attacks: acute joint pain "first and the worst" even painful to light touch
- DDx: septic joint (both may co-exist) bursitis etc.
- Gouty arthritis typically presents as monoarthropathy
- Chronic tophaceous stage: deposits in joints, ear pinna, ocular structures, and other regions. Nephrolithiasis etc. Men>women. Obesity, diet, and age >50-60.
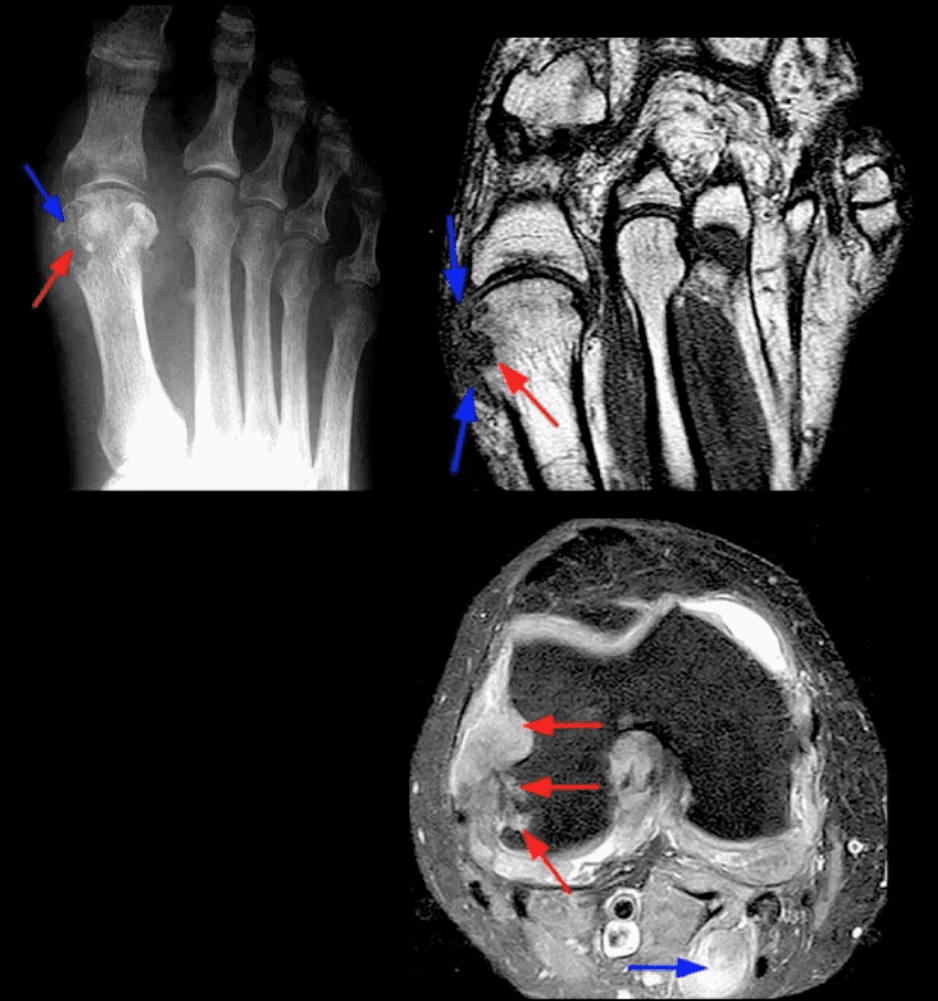
- Radiography: early attacks are unremarkable and may present as non-specific joint effusion
- Chronic tophaceous gout radiography: punched out peri-articular, para-articular and/or intraosseous erosions with overhanging edges. A characteristic rim of sclerosis and internal calcification, soft tissue tophi. Target sites: lower extremity m/c
- Rx: allopurinol, colchicine (esp. preventing acute episodes and maintenance)
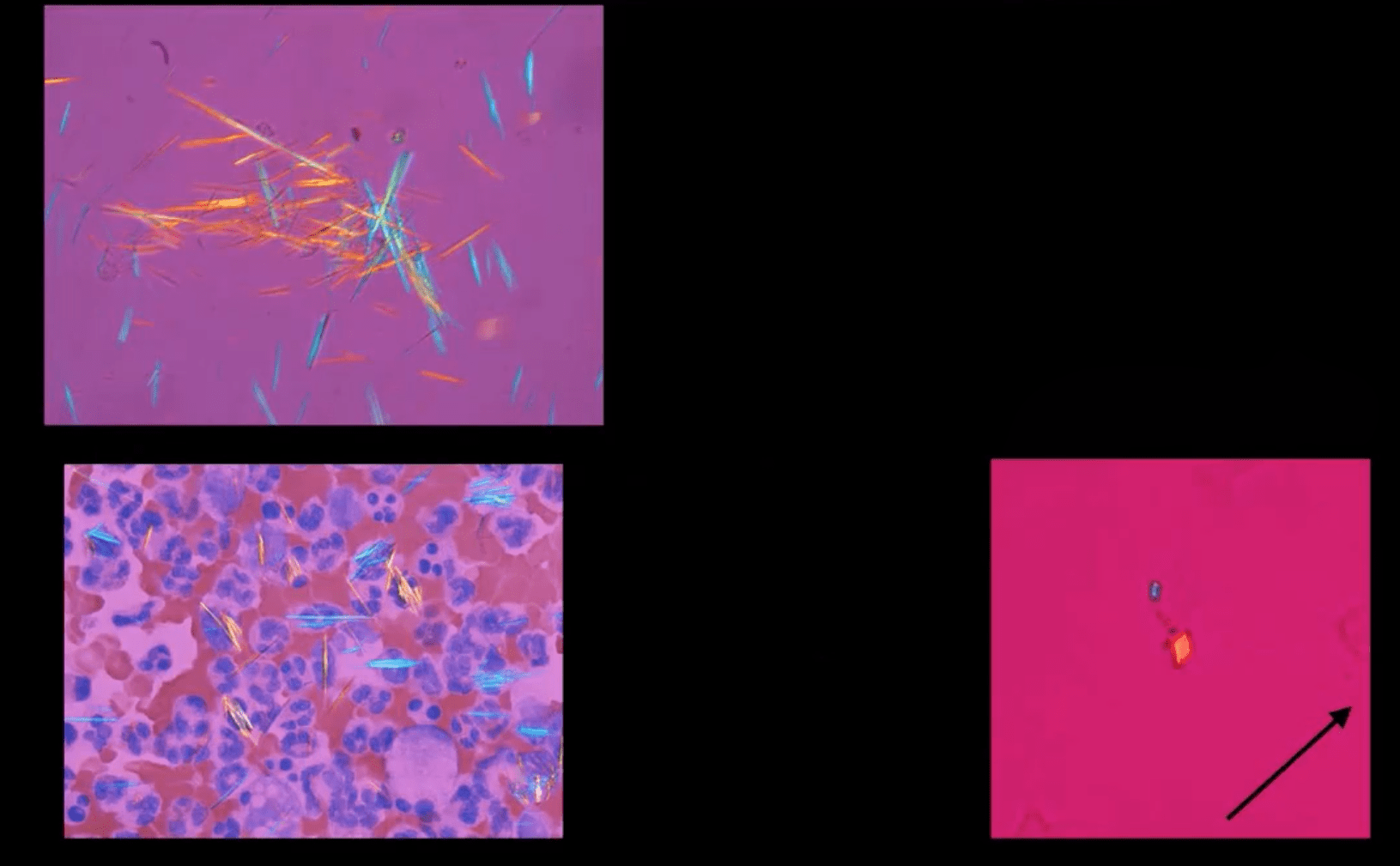
Synovial Aspiration
- Synovial aspiration with polarized microscopy reveal negatively birefringent needle-shaped MSU crystals with large inflammatory PMN presence. DDx: positively birefringent rhomboid-shaped CPPD crystals (above bottom right) seen in Pseudogout and CPPD
Large S.T.
- Density and joint effusion punched out osseous erosion with overhanging margins, overall preservation of bone density, internal calcifications Dx: chronic tophaceous gout
MRI Gout Features
- Erosions with overhanging margins, a low signal on T1 and high on T2 and fat-suppressed images. Peripheral contrast enhancement of tophaceous deposits d/t granulation tissue
- Dx: final Dx; synovial aspiration and polarized microscopy