Summary
- Neoplasms
- The vast majority of clinically suspected bone Mets are found in the axial skeleton and proximal femurs/humeri
- Radiography is the most cost-effective and readily available initial imaging tool to investigate bone Mets but often fails early metastatic detection
- Tc99 bone scintigraphy is the most sensitive and cost-effective imaging modality to demonstrate metastatic foci
- MR imaging may help regional identification of bone Mets especially if x-radiography is unrewarding
- Significant limitations of MRI: inability to perform a whole-body MRI scan
- Cost and other contraindications such as cardiac pacemakers and cochlear implants may be another limiting factor
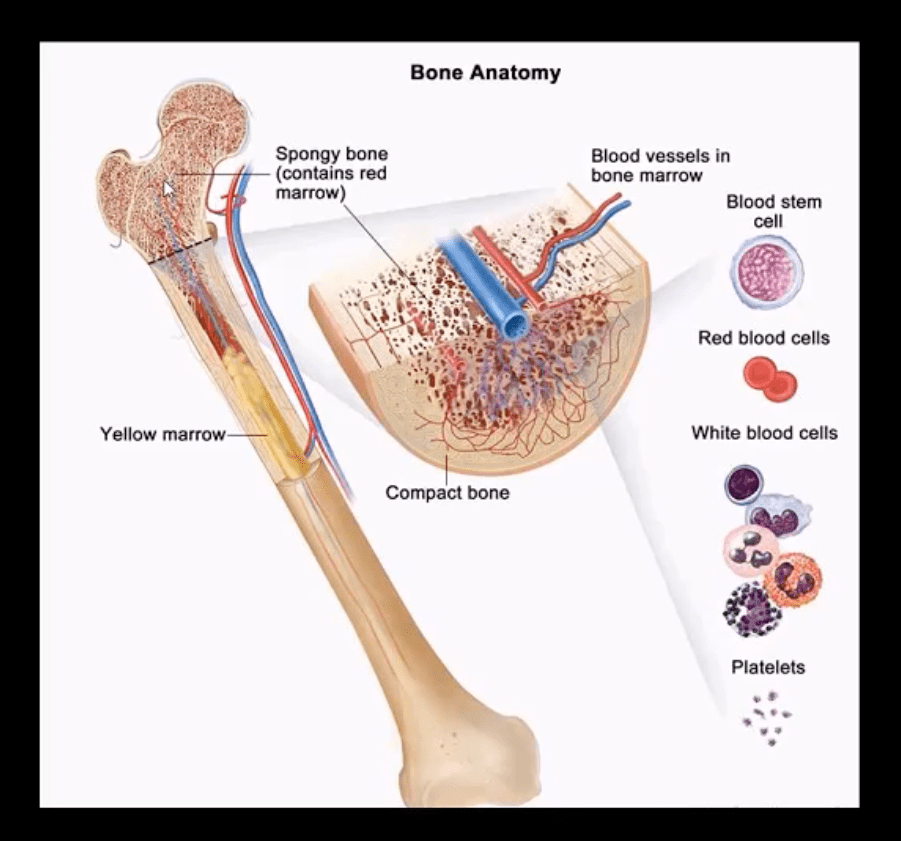
Marrow Based Neoplasms
- Malignancy originating from the marrow cells are often referred to as "round-cell tumors."
- Multiple Myeloma (MM)
- Lymphoma
- Ewing's sarcoma
- The last two are less frequent than MM
- Red marrow in adults is in the axial skeleton and proximal femurs/humeri d/t gradual marrow "retraction" following the childhood
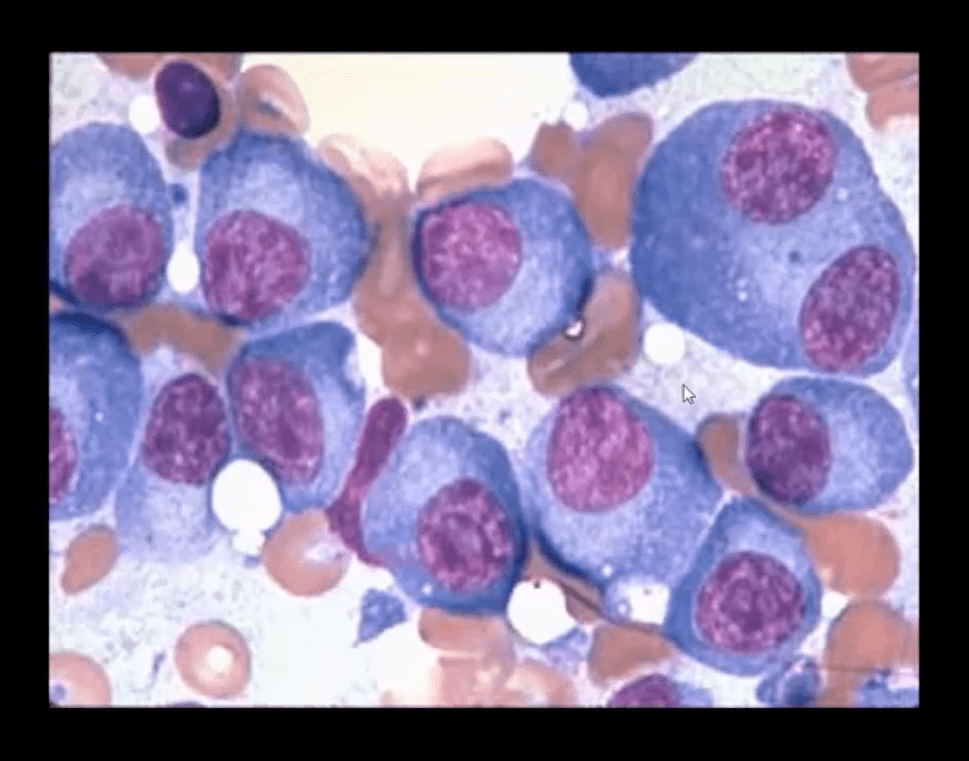
- Note bone marrow biopsy histopathology specimen of MM with abnormal plasma cells replacing regular marrow residents (above image)
- Multiple Myeloma (MM) is the most common primary bone neoplasm in adults>40s. Etiology is unknown, but many theories exist (e.g., genetic, environmental, radiation, chronic inflammation, MGUS)
- MM: malignant proliferation of plasma cells >10% of red marrow, with subsequent replacement of normal marrow cells by myeloma cells and overproduction of monoclonal antibodies paraproteins (M protein) with heavy chains IgG (52%), IgA (21%), IgM (12%) and light chains kappa or lambda aka Bence-Jones proteins
Clinical Presentation of MM
- MM is occasionally detected as unexplained anemia on routine blood studies for unrelated complaints
- Common MSK symptoms: Bone pain/Pathologic fractures
- Constitutional: Weakness/malaise
- Systemic: bleeding, anemia, Infection (especially pneumococcal) d/t marrow replacement and pancytopenia
- Hypercalcemia d/t bone resorption
- Renal failure aka myeloma kidney
- Neuropathies
- Amyloidosis
- Gout
- Diagnostic imaging plays an essential role during the Dx of MM
- Bone marrow aspiration biopsy, blood tests, and serum protein electrophoresis may be used
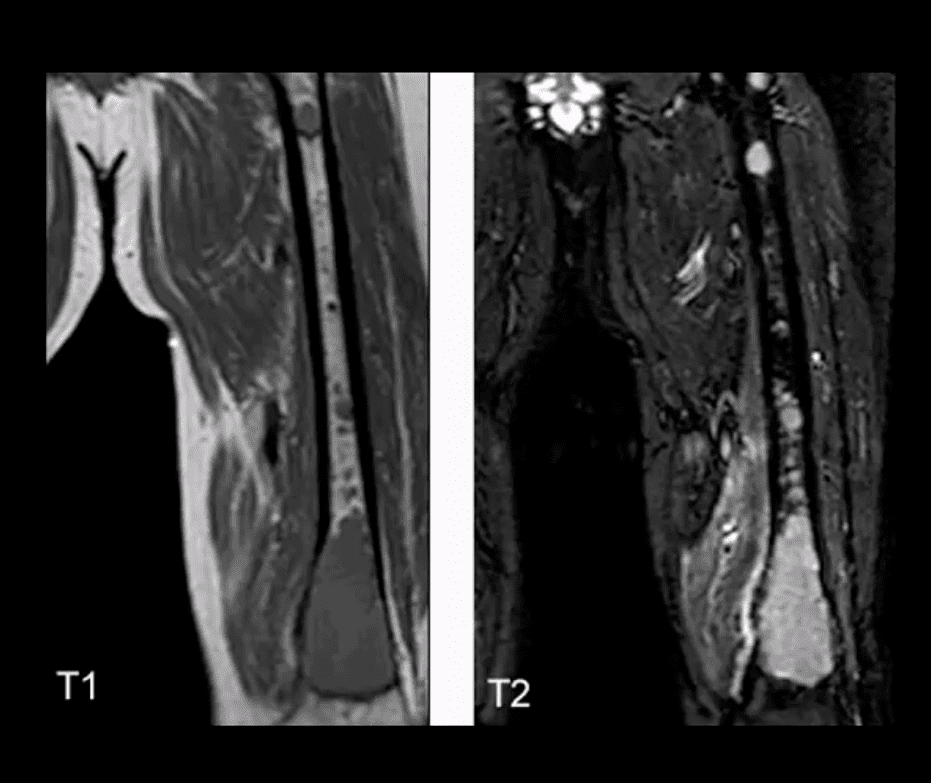
- Imaging approach: bone pain is investigated with initial x-radiographs if radiographs are unrewarding MR imaging may help to reveal bone marrow abnormality. MRI is recommended as myeloma survey
- Currently, MRI protocol known as "whole body myeloma scan" consisting of T1, T2-fat suppressed, and T1+C coronal sequences can detect MM in the skull, spine, pelvis, ribs and femurs/humeri. This technique is much more superior to radiographic "skeletal myeloma survey."
- Tc99 bone scintigraphy is not typically used for MM because over 30% of MM lesions are "cold" or photopenic on radionuclide bone scan d/t highly lytic nature of MM with osteoclasts outpacing osteoblasts.
- A radiographic skeletal survey is considered more sensitive than bone scintigraphy in MM
- PET-CT scanning of MM is gaining popularity due to the high level of detection of multiple sites of MM
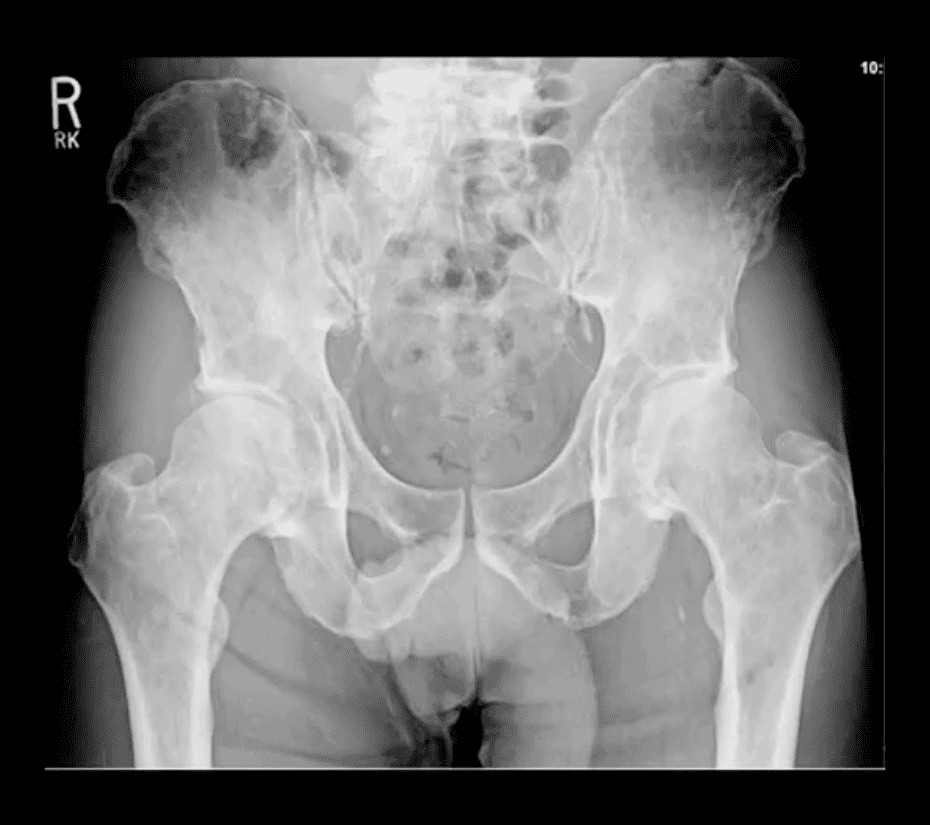
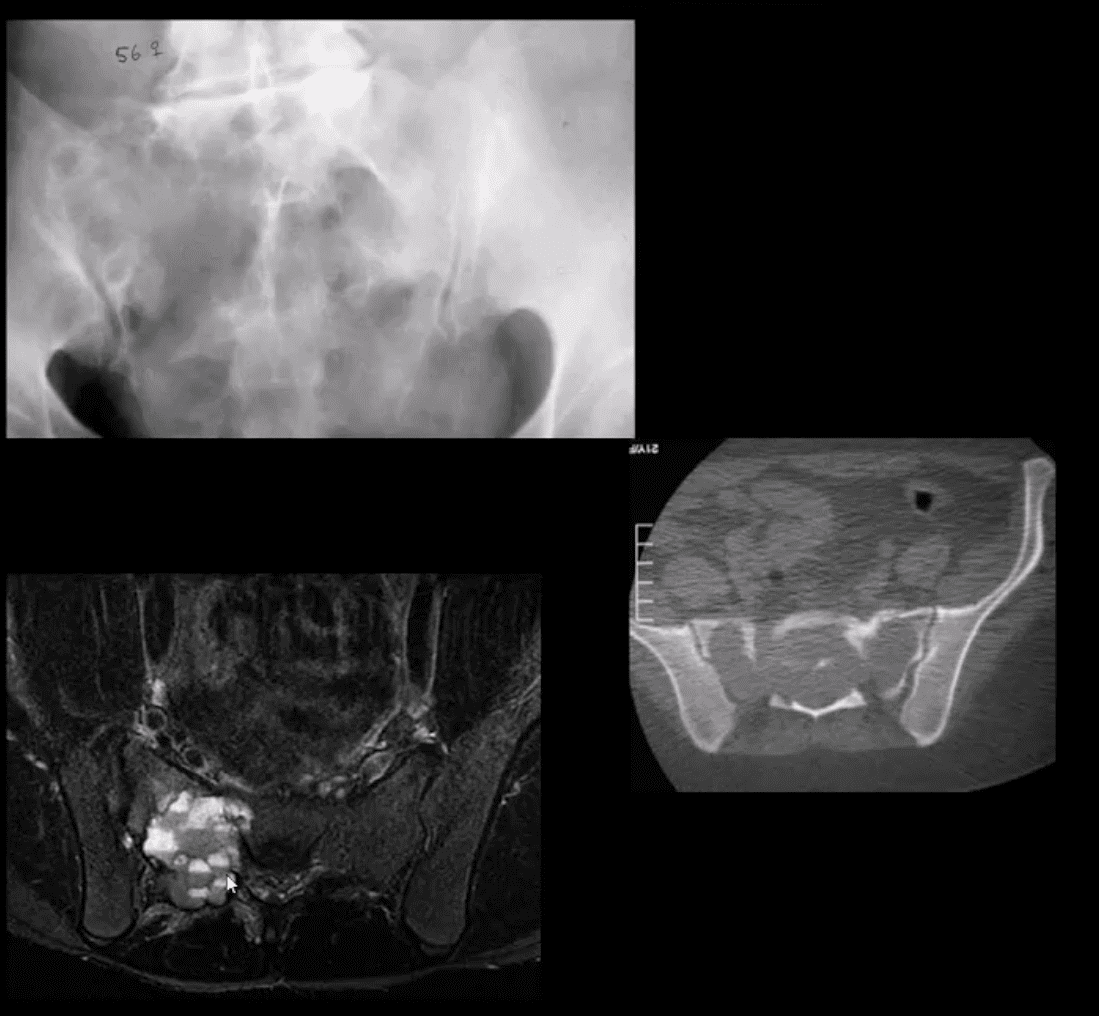
- Radiographic Dx of MM: consists of identification of characteristically localized focal osteolytic "punched out" or "moth-eaten" lesions of variable sizes following the distribution of adults red marrow
- Note rad abnormality is known as "raindrop skull" is characteristic of MM
- Radiographic appearance of MM may vary from "punched out" round radiolucencies to "moth-eaten" or permeating osteolytic lesion producing endosteal scalloping (yellow arrow)
- Pelvis and femurs are commonly affected by MM and present radiographically as round lytic punched out or moth-eaten lesions
- N.B. Occasionally MM may pose radiographic dilemma by presenting as generalized osteopenia in the spine that can be difficult to differentiate from age-related osteoporosis
- MR imaging of MM reveals marrow changes with low signal on T1, a high signal on fluid-sensitive sequences and bright contrast enhancement on T1+C gad d/t increased vasculature and high activity of MM cells
- Example of full-body MRI of "whole body myeloma scan" with T2-fat suppressed (A), T1 (B) and T1+C (C) pulse sequences produced in coronal slices
- Note multiple foci of bone marrow changes in the spine pelvis and femurs
Miscellaneous Neoplasms of the Spinal Column
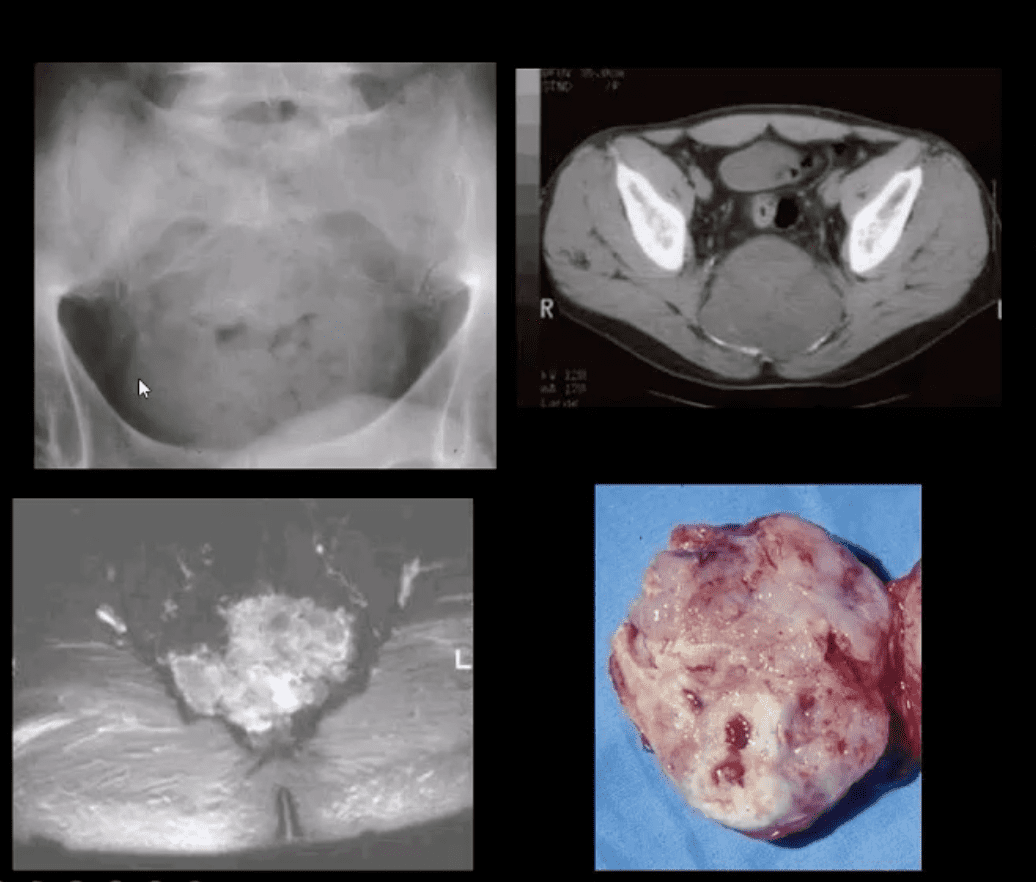
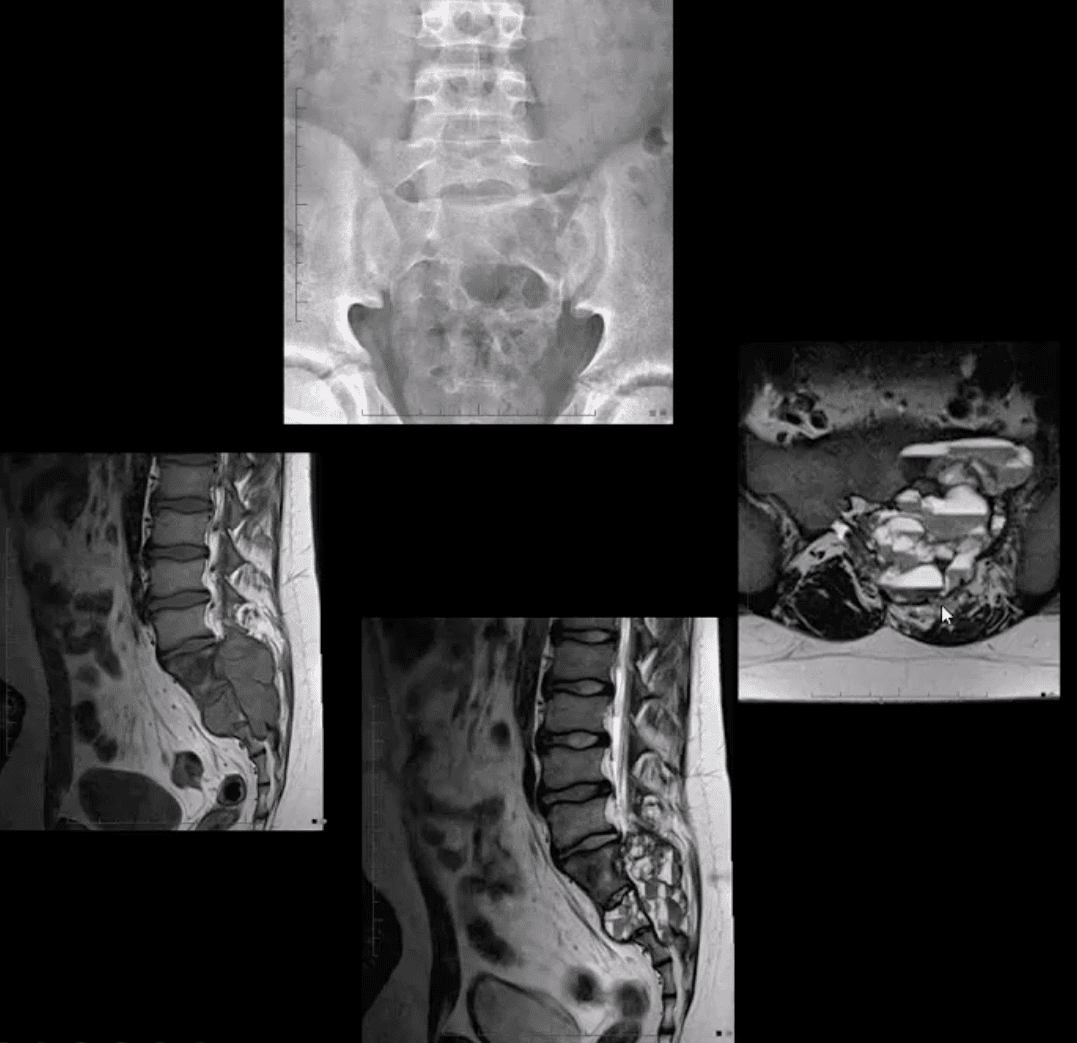
- Chordoma: is relatively uncommon but considered the m/c primary malignant neoplasm that only affects the spine. D/t slow growth is often misdiagnosed for a considerable length of time as LBP
- Pathology: derives from malignant transformation of notochordal cells presented as mucoid, gelatinous mass containing physaliphorous cells
- Demo: M: F 3:1 (30-70S). 50%-sacrococcygeal, 35% spheno-occipital 15%-spine
- Clinically: asymptomatic for a long time until non-specific LBP, changes in bladder & bowel, neurological signs are less common d/t midline "outward" growth & inferior to S1. Local invasion worsens prognosis. 60%-survive 5-years, 40%-10-years, Mets are delayed, poor prognosis d/t local invasion. >50% can be id. on DRE.
- Imaging: x-rays often tricky d/t overlying gas/feces. CT is >sensitive to id the bone mass and internal calcifications. MRI: T2 bight signal, T1 heterogeneously low and high d/t mucus/blood decomposition, MRI best detects local invasion and essential for care planning. Rx: complete excision is often impossible d/t local vascular invasion.
- Giant cell tumor (GCT): 2nd most common primary sacral tumor. It is a histolgically benign neoplasm containing multinucleated Giant cells of Monocyte-Osteoclast origin
- Imaging Dx: x-radiography is the 1st step usually in response to complaints of LBP. Often challenging to id on x-rays d/t bowel gas/feces
- Key rad feature: osteolytic expansile lesion noted by destruction of sacral arcuate lines. CT may id the lesion better. MRI is the modality of choice folowing x-rays. MRI: T1 low to intermediate signal. Heterogeneously high d/t edema with areas of low signal on T2 d/t blood degradation and fibrosis. Characteristic fluid-fluid levels may be noted especially if ABC develops within a GCT. Rx: operative. Prognosis is less favorable than GCT in long bones d/t lung Mets (deposits) in 13.7%
- Aneurysmal Bone Cysts (ABC) are benign expansile tumor-like bone lesions (not a true neoplasm) composed and filled with numerous blood-filled channels. Thus the term "blood sponge." ABC is m/c id in children and adolescents
- Unknown etiology: trauma and pre-existing bone neoplasm (e.g., GCT) often reported. Clinically: pain that may be progressive d/t rapid nature of ABC expansion. In the spine, ABC m/c affects posterior elements and presented as expansile, soap-bubbly or lytic lesion.
- DDx: can be broad, but Osteoblastoma and GCT are the top DDxs.
- Imaging: x-rays demo expansile mass in posterior elements, CT is more sensitive than x-rays, MRI will demo characteristic fluid-fluid levels and mixed high and low signal d/t edema and blood decomposition/aging with some septations.
- N.B. MRI fluid-fluid levels are not exclusive to ABC, and DDx includes GCT, osteoblastoma, telangiectatic osteosarcoma.
- Rx: operative curettage and bone grafting, fibrosing agents. Recurrence 10-30%.