Pyogenic Spinal Infection
- aka Spondylodiscitis and vertebral osteomyelitis overall are relatively infrequent and may present with bimodal distribution: children and adults >50's
- Occasionally considered as two separate entities due to variations in the blood supply of pediatric vs. adult spines
- Risk factors/causes: distant site of infection in the body (25-35%), e.g., oropharynx, urogenital infections, bacterial endocarditis, indwelling catheters, florid skin infections furunculosis/abscess, etc.
- Iatrogenic: operative (e.g., discectomy) interventional or diagnostic/therapeutic procedures
- Penetrating trauma
- Immunocompromised patients
- Diabetics
- Malnourished patients or patients with low protein
- IV drug users
- Chronic disease patients, cancer patients, etc.
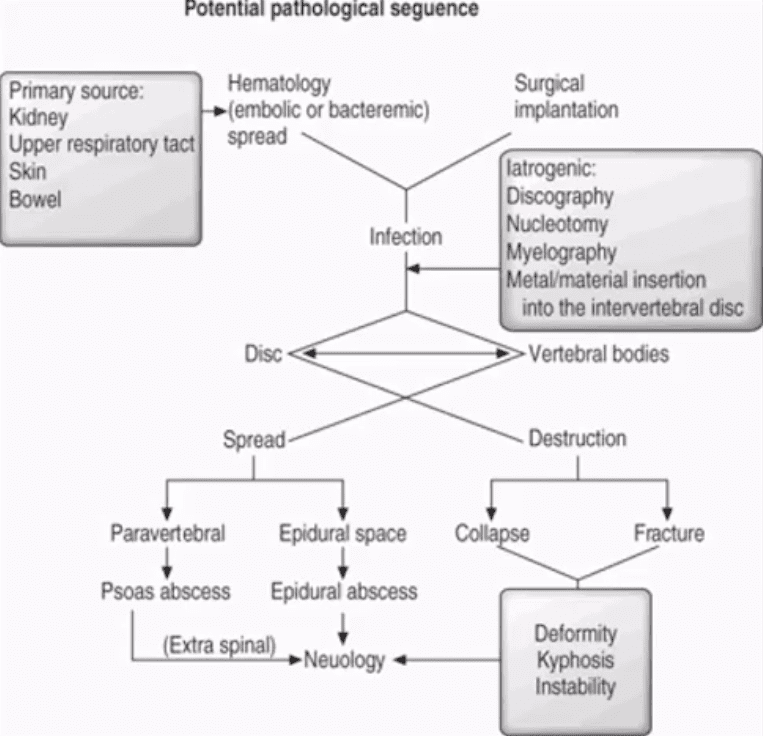
Potential Pathological Sequence
Clinical Presentation
- Back pain with or w/o high fever and other "septic" signs. High temperature may only present in 50% of children
- Exacerbation of pre-existing back pain in post-surgical cases
- Neurological complications in advanced cases of vertebral destruction and epidural abscess
- Meningitis, septicemia, etc.
- Labs: Blood tests are unspecific, may or may not indicate elevated ESR/CRP, WBC
- Diagnostic imaging is important but
- If clinical suspicion is strong, prompt I.V. antibiotics are needed to prevent serious complications
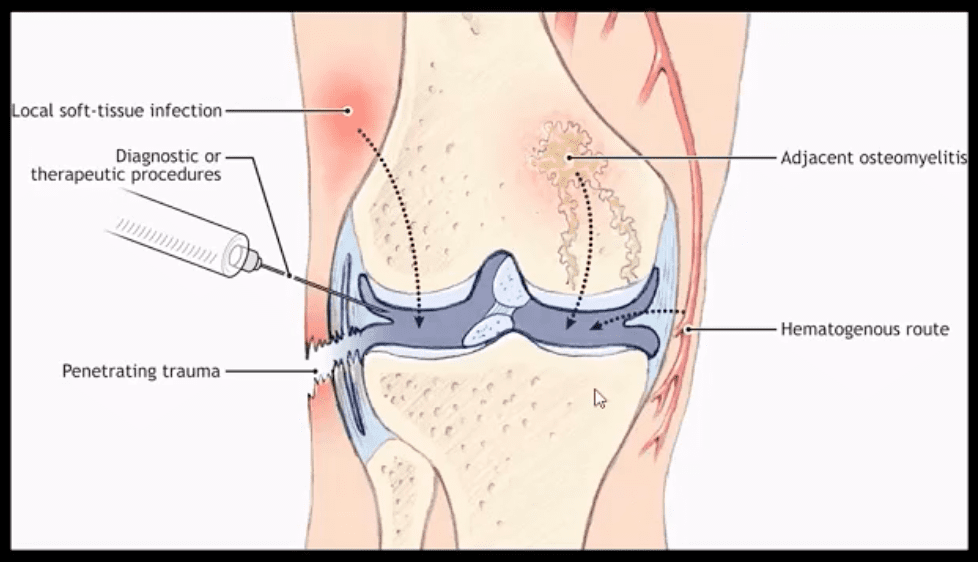
Routes of Infection
- Infection routes to the spine are similar to bone in general
- 3-distinct routes:
- 1) Hematogenous spread as bacteremia (most common)
- 2) Adjacent site of infection (e.g., soft tissue abscess)
- 3)Direct inoculation (e.g., iatrogenic or traumatic)
- M/C organism Staph. Aureus
- Mycobacterium TB (tuberculous spinal osteomyelitis) aka Pott's disease can be presented in cases of re-activated or disseminated pulmonary TB
Mechanisms of Spinal Infection
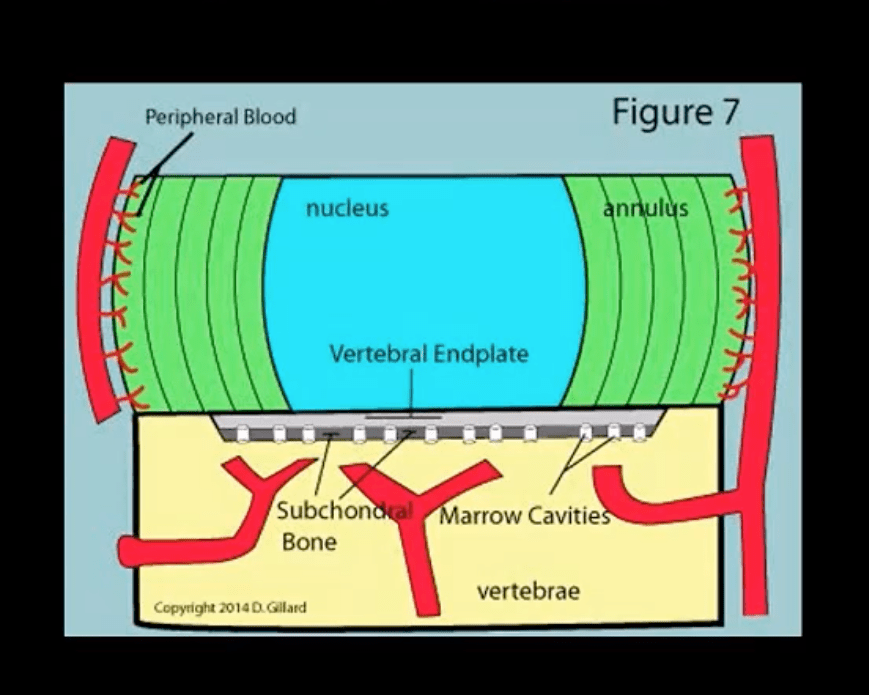
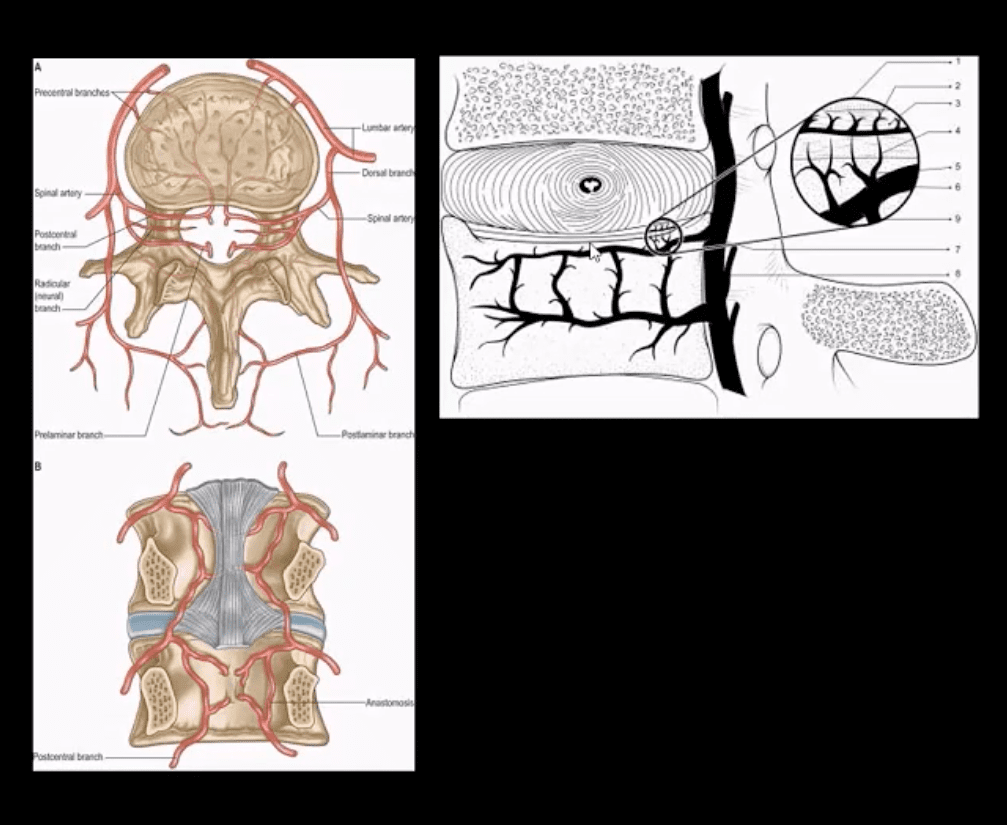
- May vary depending on the patients' age
- In children, the IVD receives direct blood supply and can be infected directly spreading to adjacent bone and causing spondylodiscitis
In Adults
- The disc is avascular
- Pathogens invade adjacent vertebral end-plates via end-arterial supply of the vertebral body that may facilitate infection due to slow, turbulent flow
- Organisms may then quickly gain access to disc substance rich in nutrients (discitis) often w/o significant initially visible destruction to the bone
- Thus, one of the earliest rad. findings of spinal infection or sudden reduction of disc height
- Later end-plate irregularity/sclerosis may develop, subsequently affecting the entire adjacent vertebral bodies
Diagnostic Imaging
- Initially, in most cases of MSK complaints, radiography is the 1st imaging step
- Initially, X-radiography is often unrewarding and may appear unremarkable for 7-10 days or presents with some subtle soft tissue changes (e.g., obscuration of Psoas shadows, etc.)
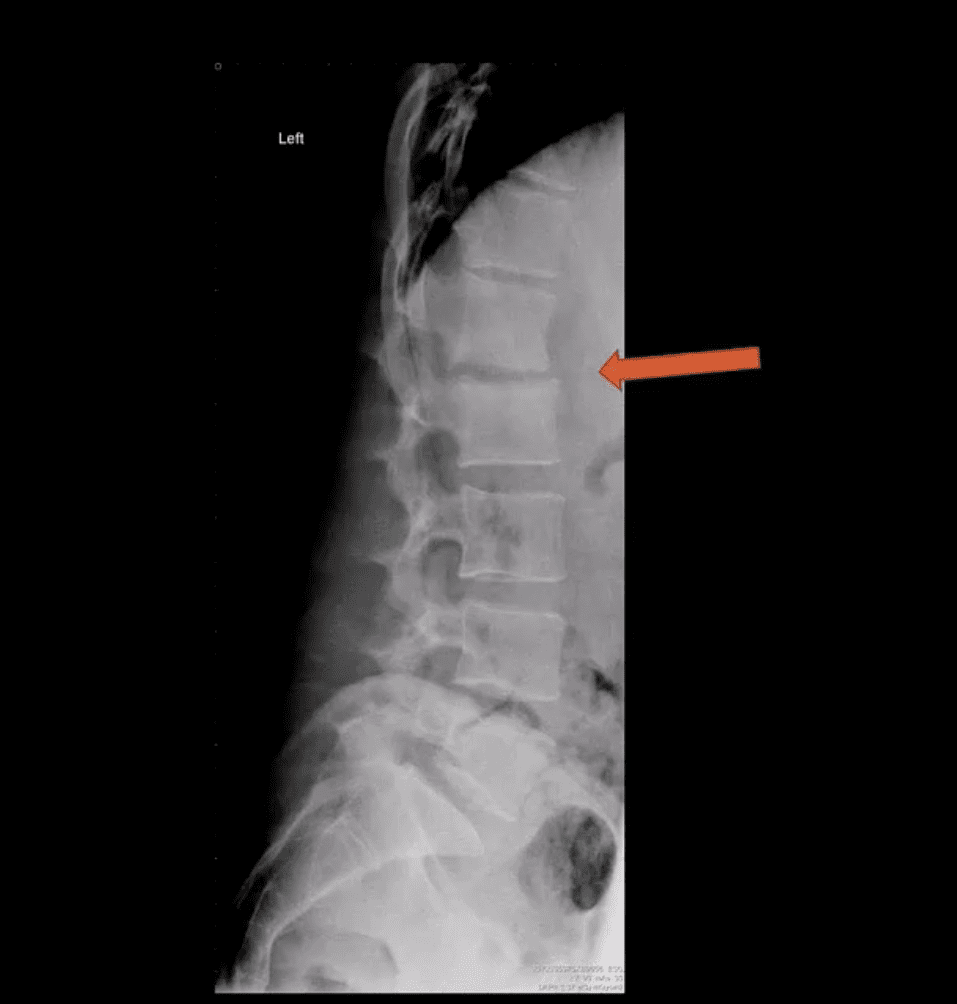
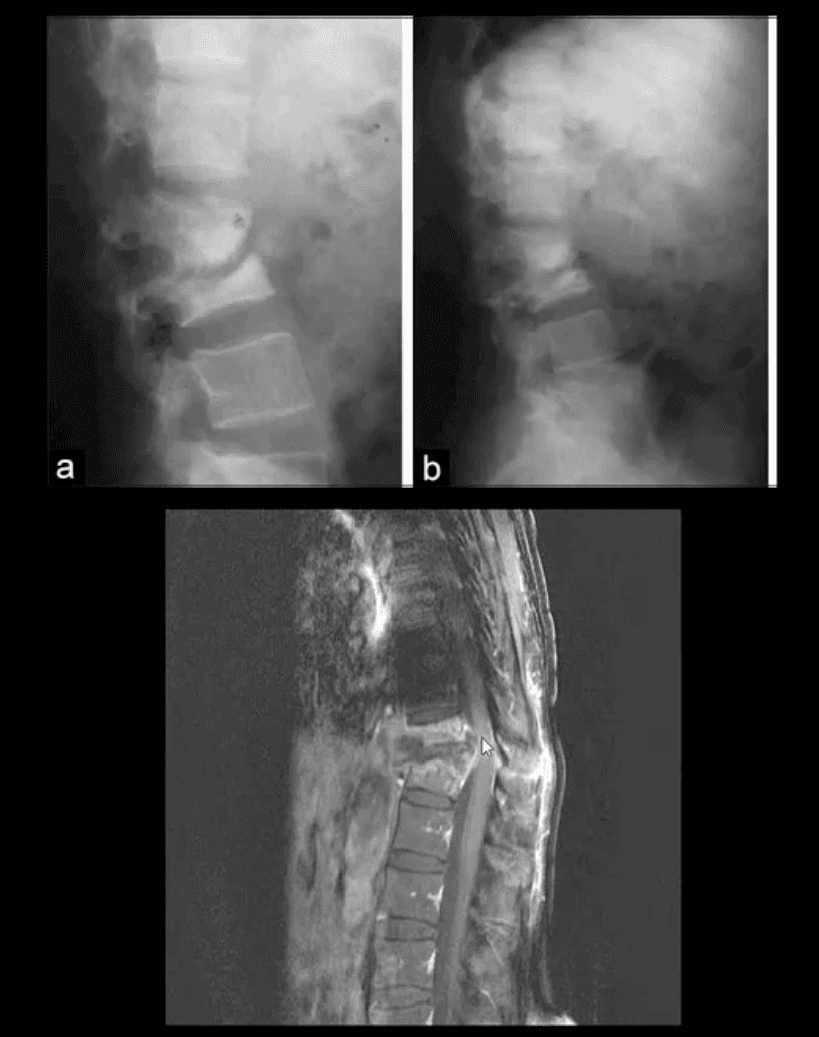
- Some of the earliest x-ray signs of pyogenic spondylodiscitis: sudden reduction of disc height (above arrow) during initial 7-10 days
- Subsequently (10-20 days) some end-plate irregularity and adjacent sclerosis may be noted
- In more advanced cases, subsequent vertebral destruction and collapse may occur
- N.B. Reliable feature to DDx between spinal infection and metastasis is the preservation of disc height in the latter
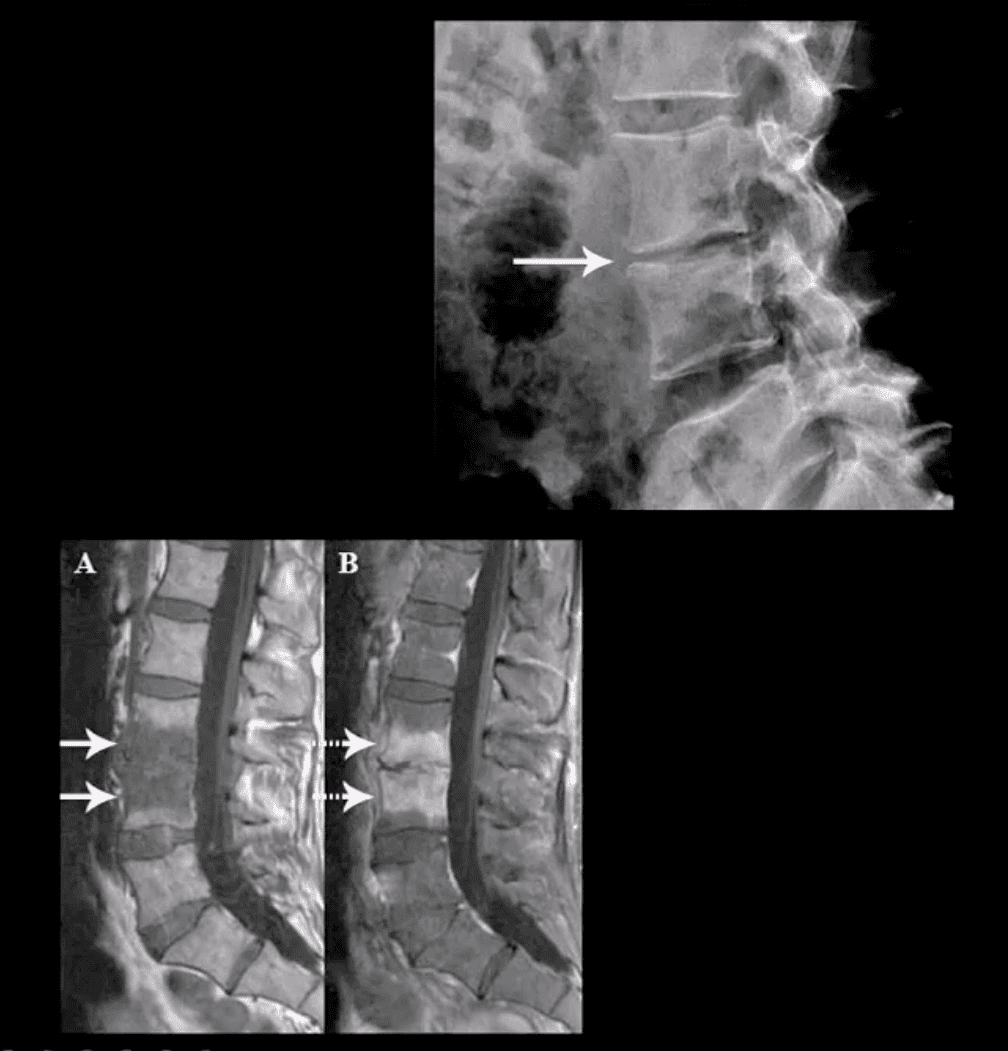
Discitis
- Discitis needs to be DDx from DDD (spondylosis)
- An important DDx between discitis and DDD is lack of osteophytes (spondylophytes) and intradiscal gas (vacuum phenomenon) in DDD.
- Presence the of intradiscal gas (vacuum phenomenon) virtually excludes discitis (except if gas-forming pathogens are involved)
- Note: sudden disc narrowing with no appreciable spondylosis (above the first image) is suspicious for infection (discitis)
- MRI +C is required to evaluate suspected infection
- N.B. 50-60% of pyogenic spondylodiscitis occur in the lumbar region
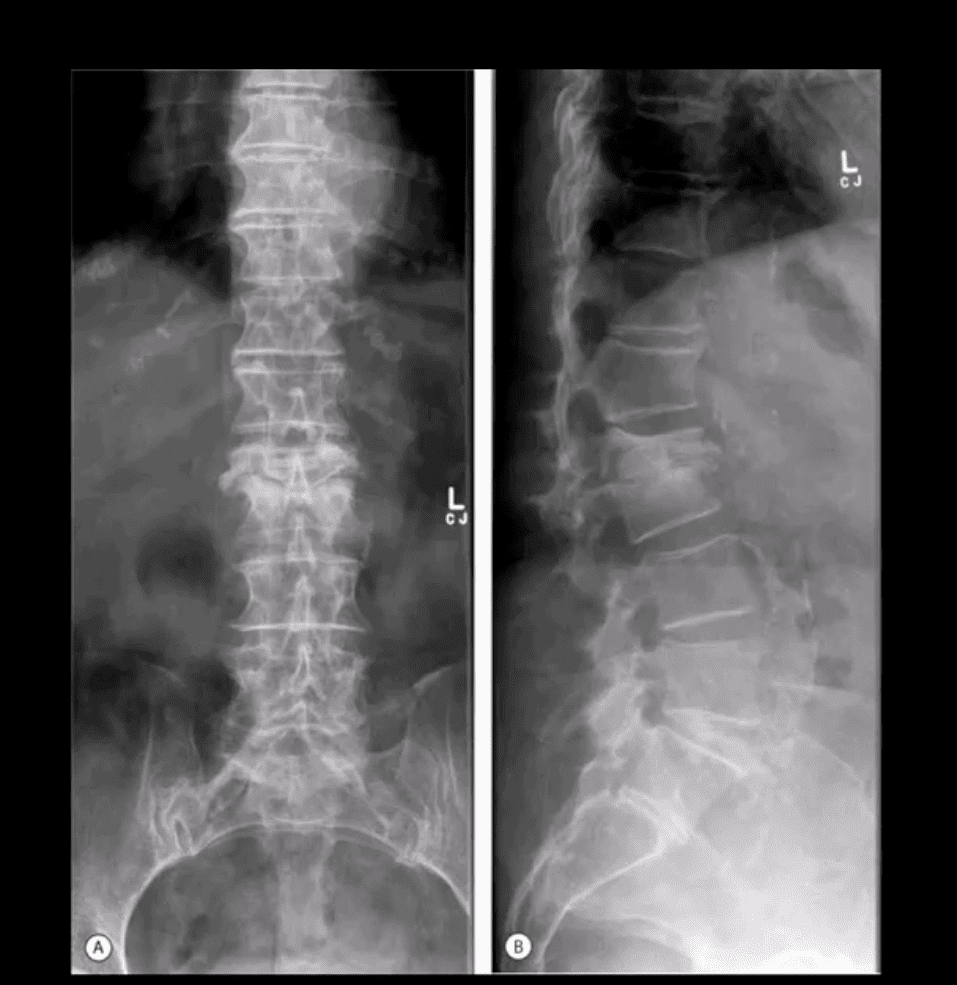
AP & Lateral Lumbar Radiographs
- Note severe disc narrowing and adjacent vertebral body destruction at L1-L2 in a 68 -y.o.-female with a known Hx of type 2 DM
- Additional imaging modalities should be used to support the Dx
- Final Dx: Pyogenic Spondylodiscitis
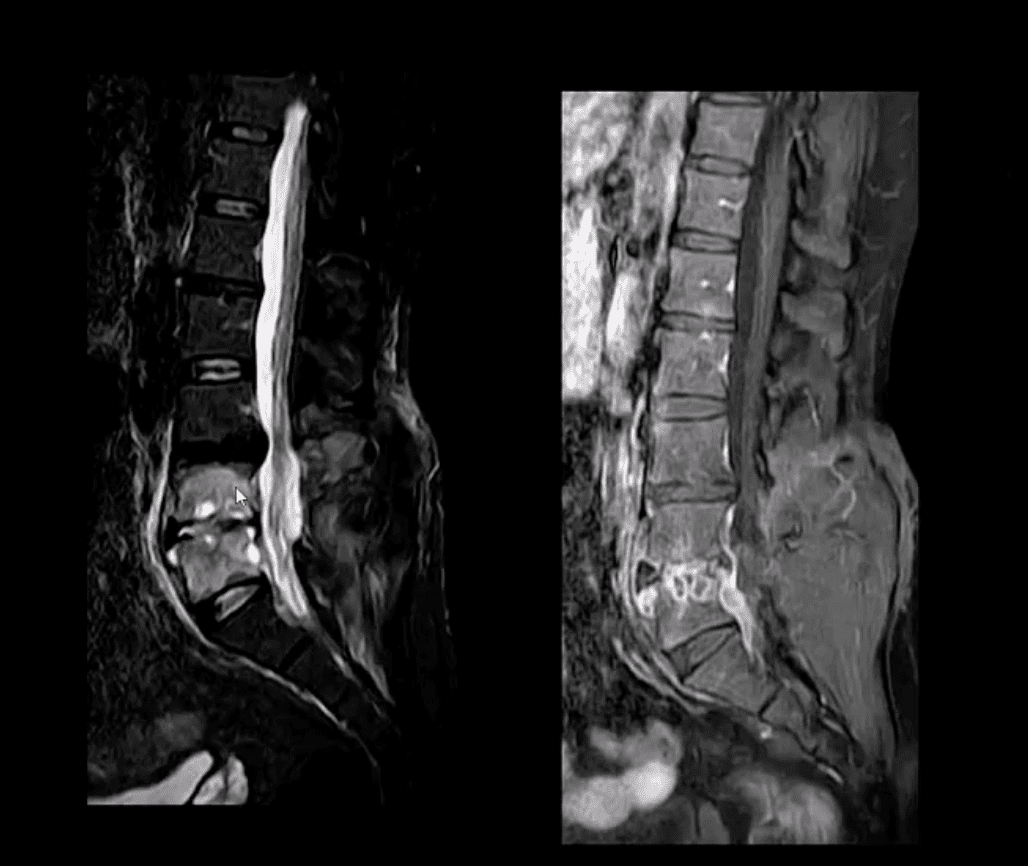
Sagittal T1 & T2 MRI
- Weighted MRI slices of a patient who had laminectomy at L4
- MR imaging with gad contrast is the modality of choice for Dx of spinal infection
- Early septic changes affecting the disc and adjacent vertebral end-plates are readily demonstrated as a low signal on T1 and high T2/STIR d/t edema and inflammation
- T1 FS +C gad images show avid enhancement of the lesion due to granulation tissue around the phlegmon. Peripheral enhancement is also characteristic of an abscess.
- Epidural extension/abscess can also be successfully detected my MRI
- N.B. 50% of epidural abscess cases present with neurological signs
STIR & T1 FS +C Gad Sagittal MRI
- Marked septic collection and edema affecting L4-5 disc and vertebral body with some epidural extension and paraspinal soft tissue edema. Avid contrast enhancement is noted surrounding low signal foci within the bone and disc tissue, some gad. Enhancement is observed in posterior paraspinal muscles and dural spaces
- Management: Dx of spondylodiscitis requires prompt I.V antibiotics. If instability and neurological complications develop referral to a Neurosurgeon is required
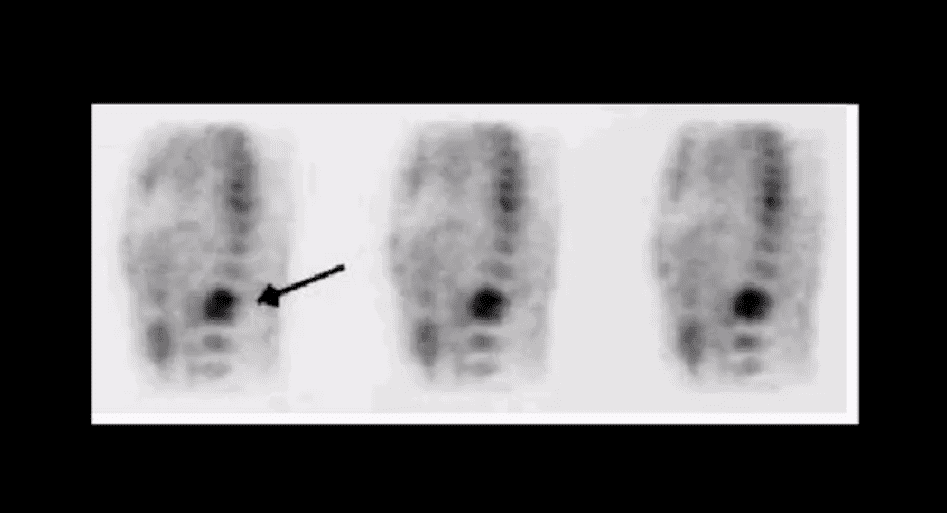
MRI Unavailable or Contraindicated
- Bone scintigraphy is very sensitive but non-specific for spinal infection but overall is of great value d/t higher sensitivity than x-rays and relatively low cost.
- An area of increased flow with radiopharmaceutical uptake is characteristic but not specific sign of spondylodiscitis
- If neurological symptoms are present and MRI is contraindicated than CT myelography may be used
TB Osteomyelitis aka Pott's Disease
- TB osteomyelitis is increasing d/t HIV and other immunocompromised states. Extrapulmonary TB m/c affects the spine and especially the thoracic spine (60%)
- Radiographic Pathology: TB bacillus infects the vertebral body and often spreads subligamentously. "Cold" paraspinal abscess collection may develop and spreads along fascial planes, e.g., Psoas abscess. Disc spaces are preserved until v. late and skip areas are noted helping to DDx TB from pyogenic infection. Severe vertebral destruction aka Gibbus deformity may develop (>60-degree sometimes) and may become permanent. Neurologic and many regional complications may develop
- Imaging approach: CXR with spinal x-rays 1st step that may be unrewarding but may potentially reveal VB destruction w/o disc narrowing. CT scanning is more superior than x-rays. MRI with gad C is a modality of choice
- Management: isoniazid, rifampin, operative.
- DDx: Fungal/Brucella infection, neoplasms, Charcot spine