Meniscal Tears
- Acute or chronic. Imaged with MRI (95% sensitivity & 81% specificity)
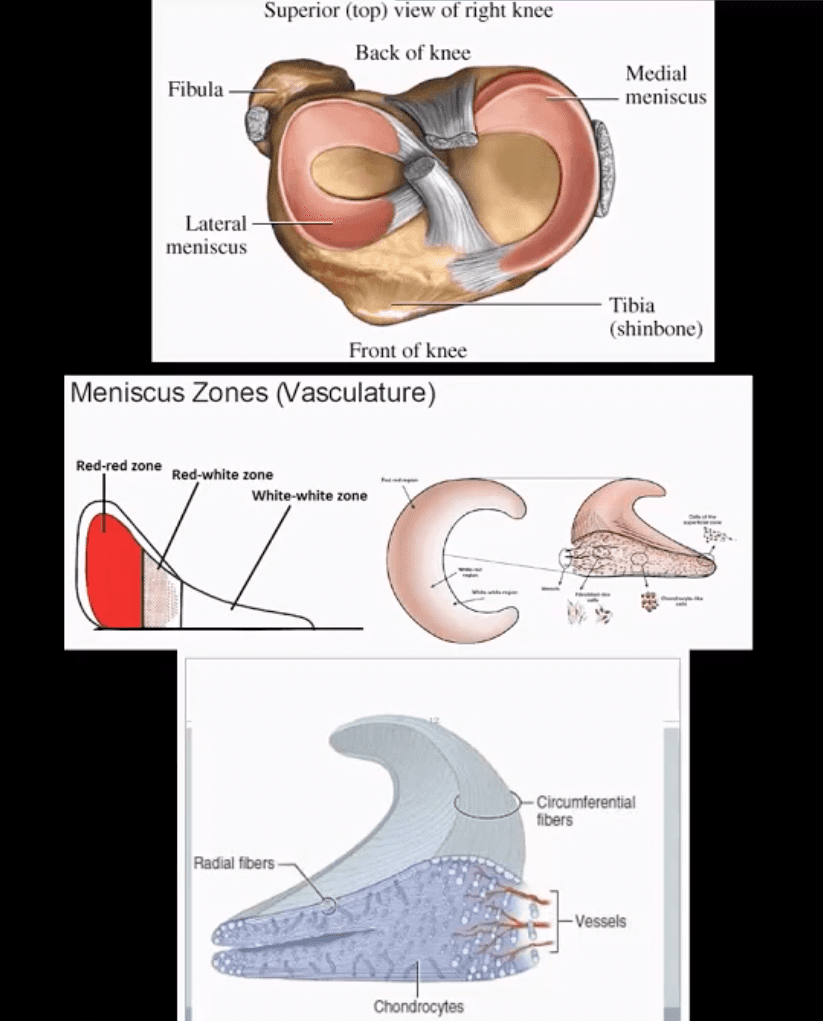
- Menisci are formed by a composition of radial and circumferential collagen fibers (97% type 1) mixed with cartilage, proteoglycans, etc. 65-75% H2O
- Aging can lead to meniscal attrition
- Acute tears are d/t rotational and compressive forces, ACL deficient knees show greater chances of meniscal tears
- Posterior horn of medial meniscus is m/c torn except in acute ACL tears when the lateral meniscus is m/c torn
- The meniscus is well vascularized in children. In adults, 3-zones exist: inner, middle and outer (above bottom image)
- Injury of the inner zone has no chance of healing
- Injury of the outer zone (25% in total) has some healing/repair
Clinical Presentation
- Pain, locking, swelling
- Most sensitive physical sign: pain on palpation at the joint line
- Tests: McMurry, Thessaly, Apply compression in prone
- Management: conservative vs. operative depends on location, stability, patient's age, and DJD and the type of tear
- Partial meniscectomy is performed. 80% proper functions on follow up. Less favorable if >40-y.o and DJD
- Total meniscectomy is not performed and only viewed historically. 70% OA 3-years after surgery 100% OA after 20 years post surgery.
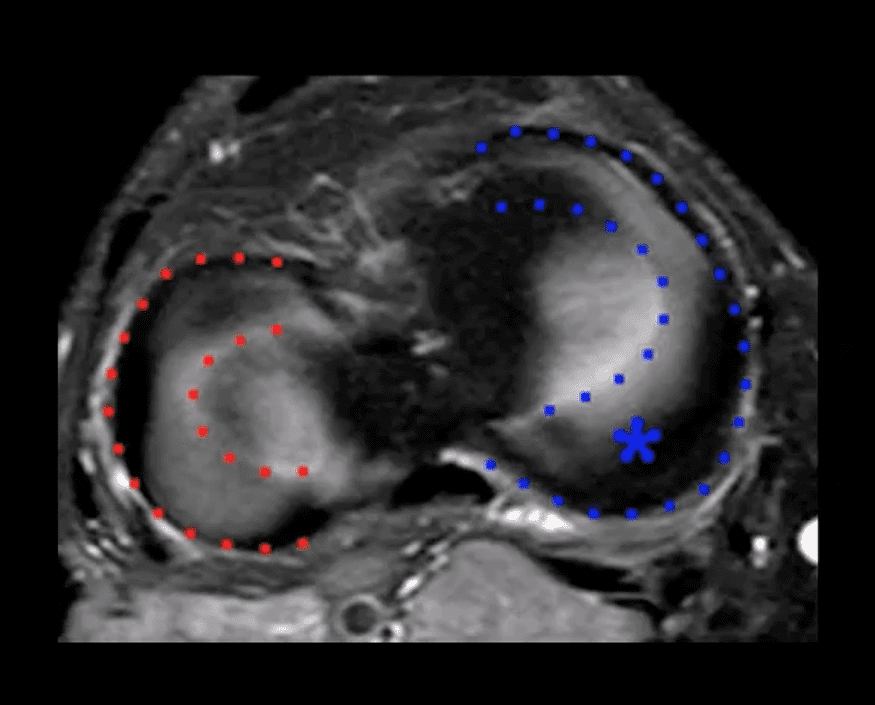
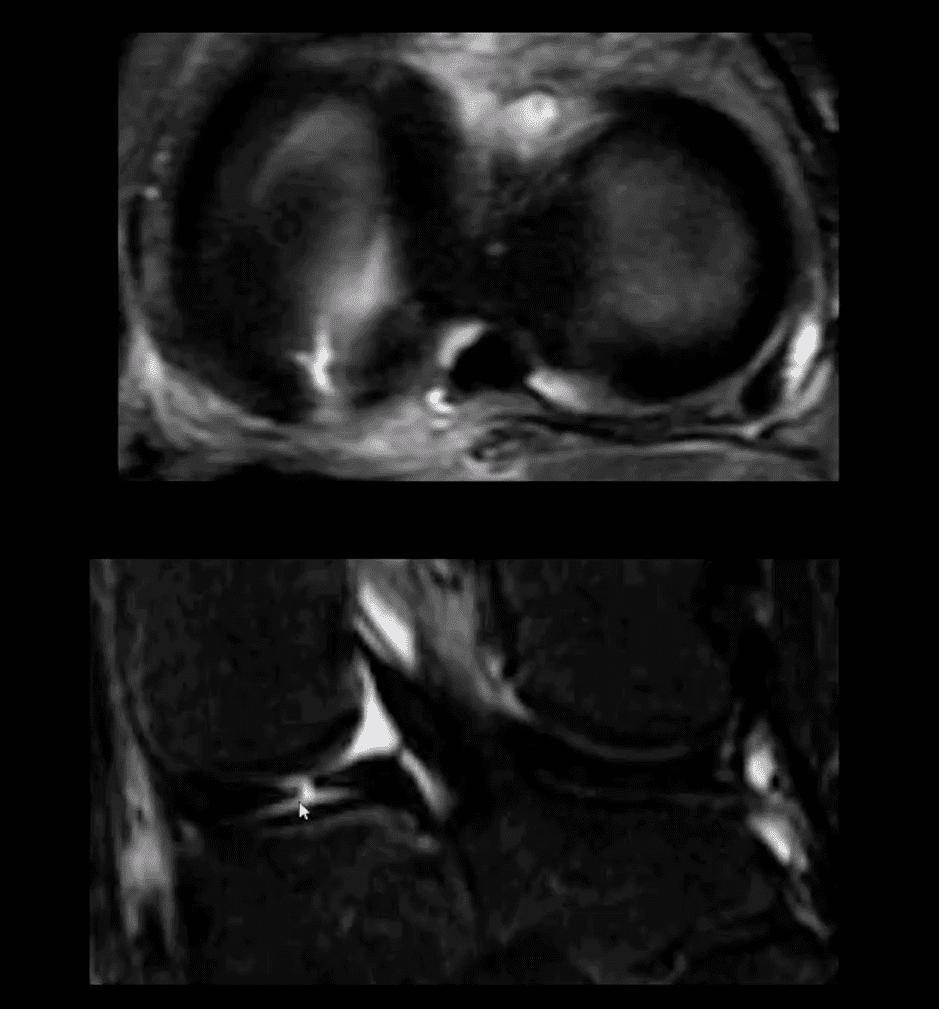
Axial MR
- Appearance the medial (blue) and the lateral meniscus (red)
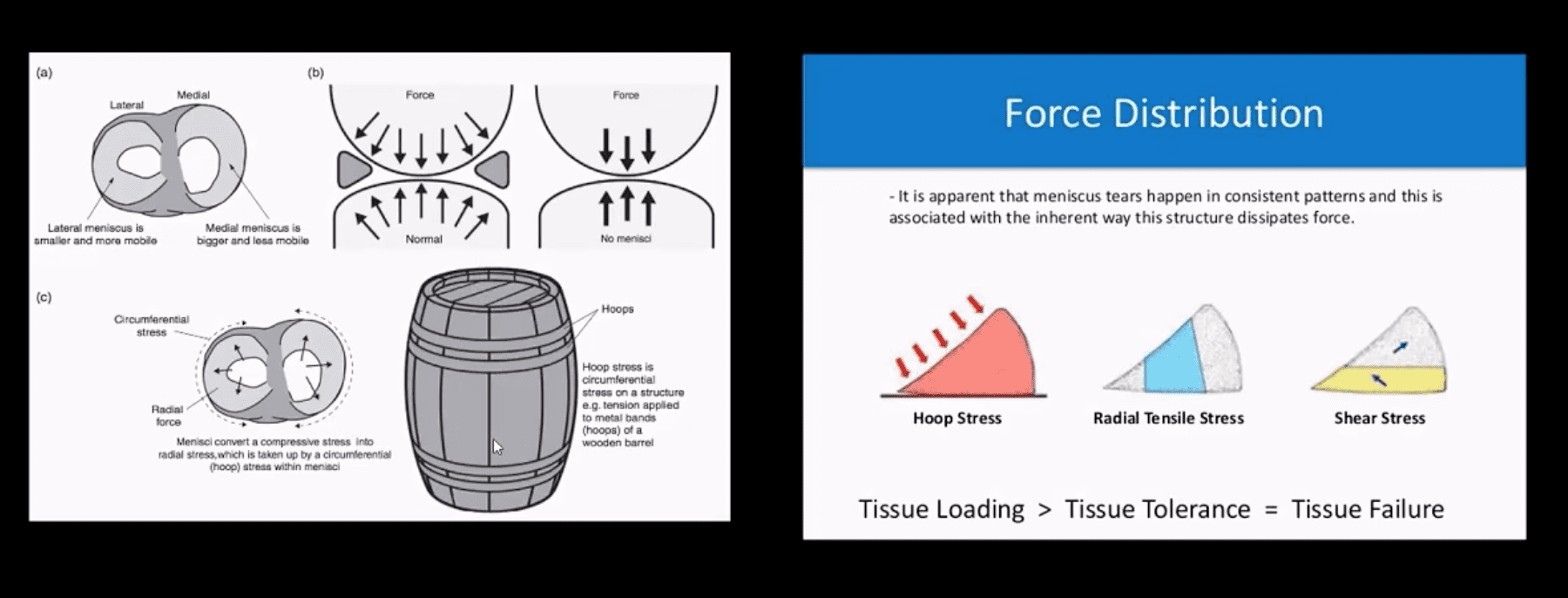
Menisci Play Significant Role
- One of the essential roles is "hoop-stress" mechanism.
- Particularly radial tears may significantly interfere with this mechanism.
- Further reading: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435920/
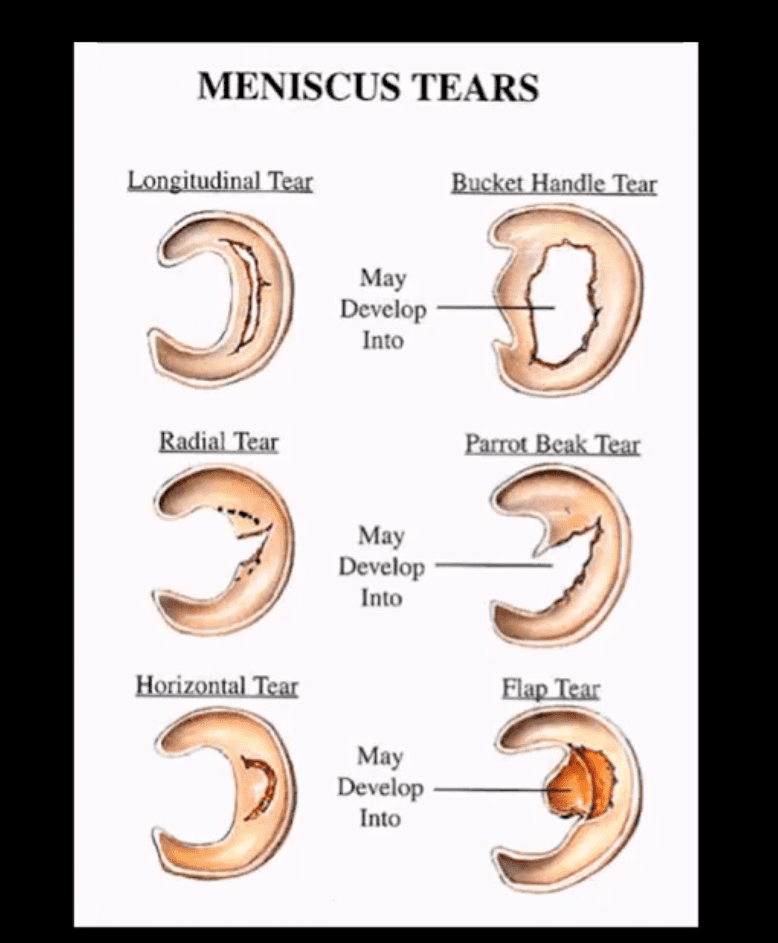
Types Location & Stability
- Types, location, and stability of tears are v. important during MRI Dx
- Vertical/longitudinal tears especially occur in acute ACL tears. Some longitudinal tears found at the periphery or "red zone" may heal
- Bucket handle tear: longitudinal tear in the inner edge that is deep and vertical extending through the long axis and may displace into a notch
- Oblique/flap/parrot-beak are complex tears
- Radial tear at 90-degree to plateau
Axial T2
- Axial T2 WI fat-sat and coronal STIR slices of the posterior horn of the medial meniscus.
- Note a radial tear of the posterior horn of the medial meniscus near the meniscal root. This is potentially an unstable lesion requiring operative care
- The meniscus, in this case, is unable to provide a "hoop-stress mechanism."
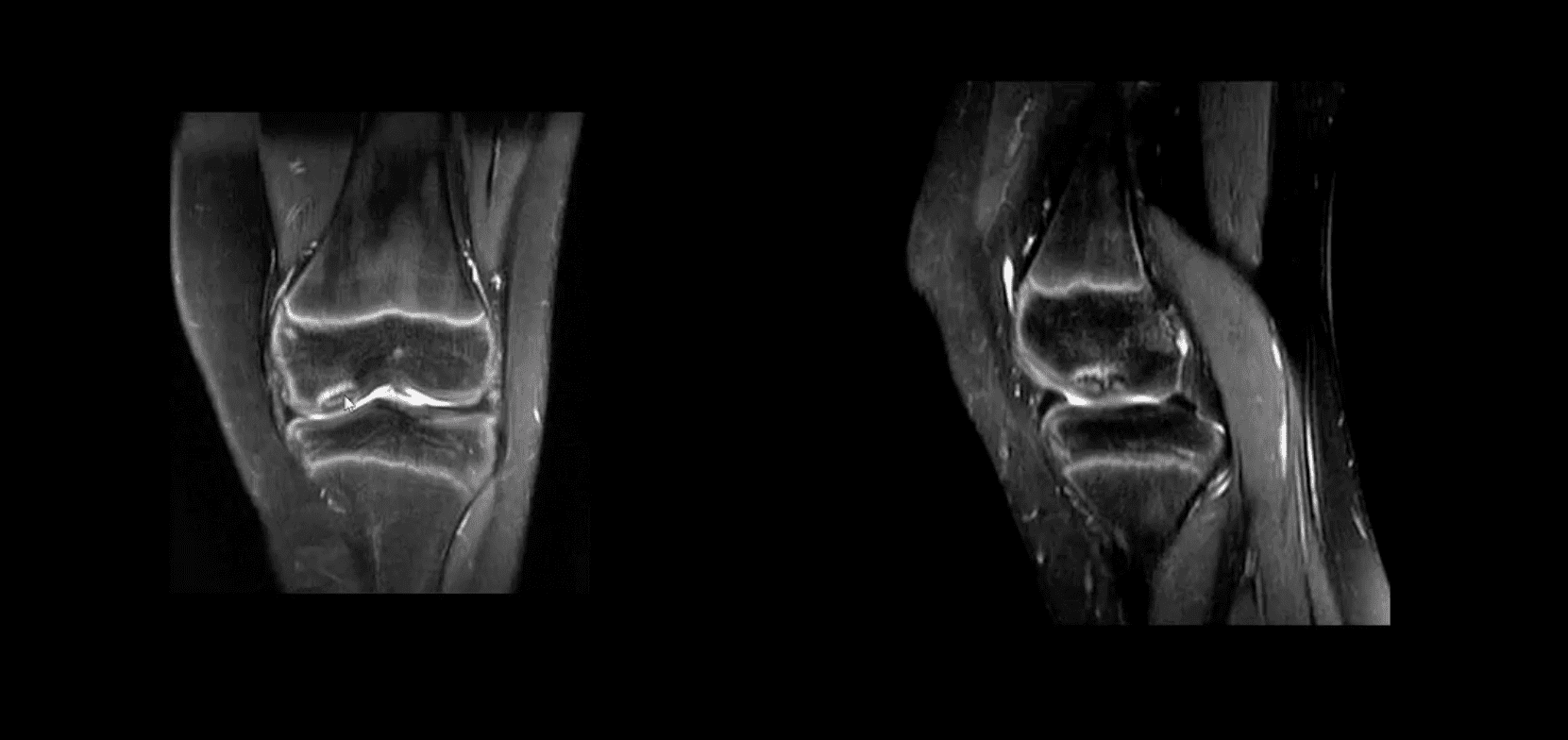
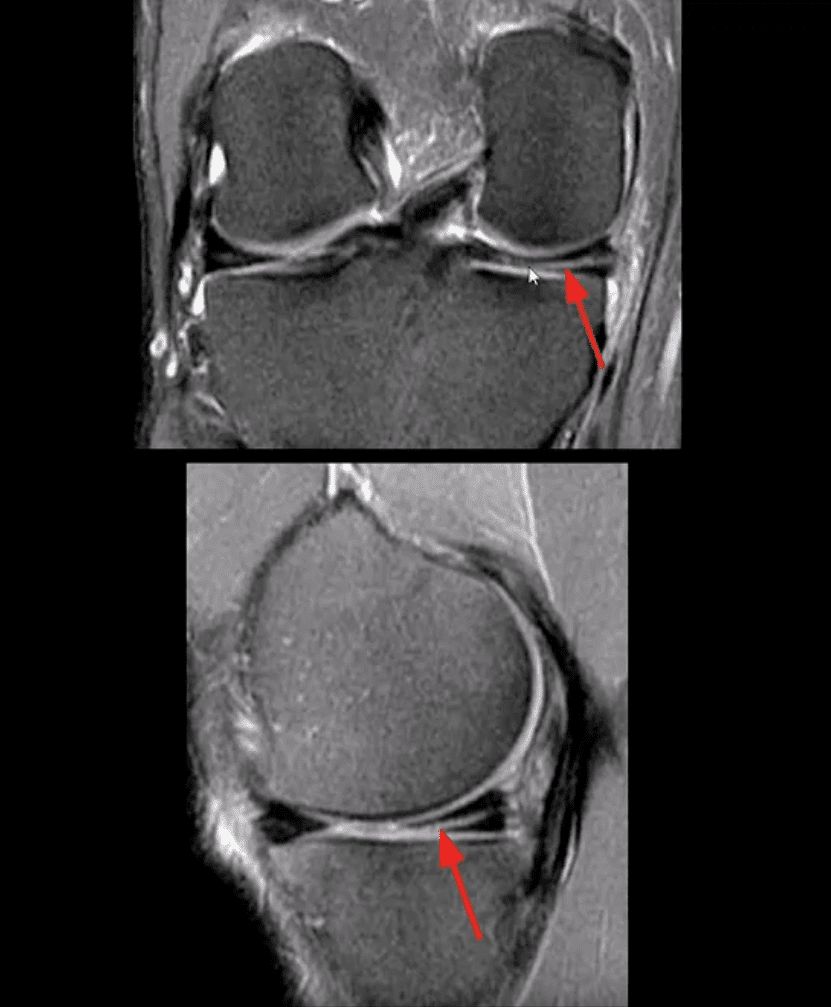
MRI Slices Coronal & Sagittal
- Fat-sat coronal and sagittal proton density MRI slices revealing horizontal (cleavage) tear that is more typical in the aged meniscus
- In some cases, when this tear does not contain a radial component, it may partially heal obviating the need for operative care
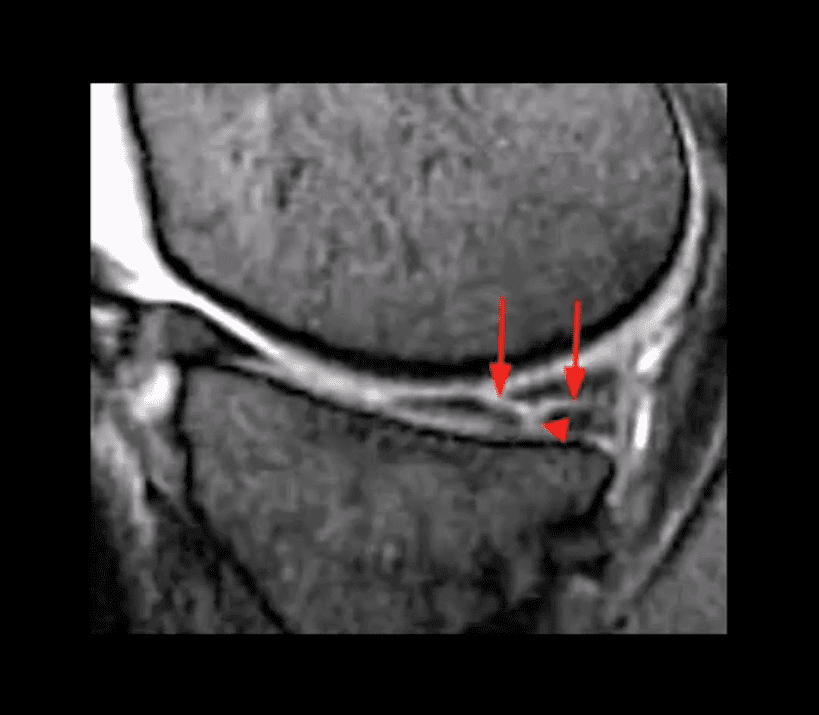
T2 w GRE Sagittal MRI Slice
- Complex tear with a horizontal oblique and radial component.
- This type of tear is very unstable and in most cases may need operative care
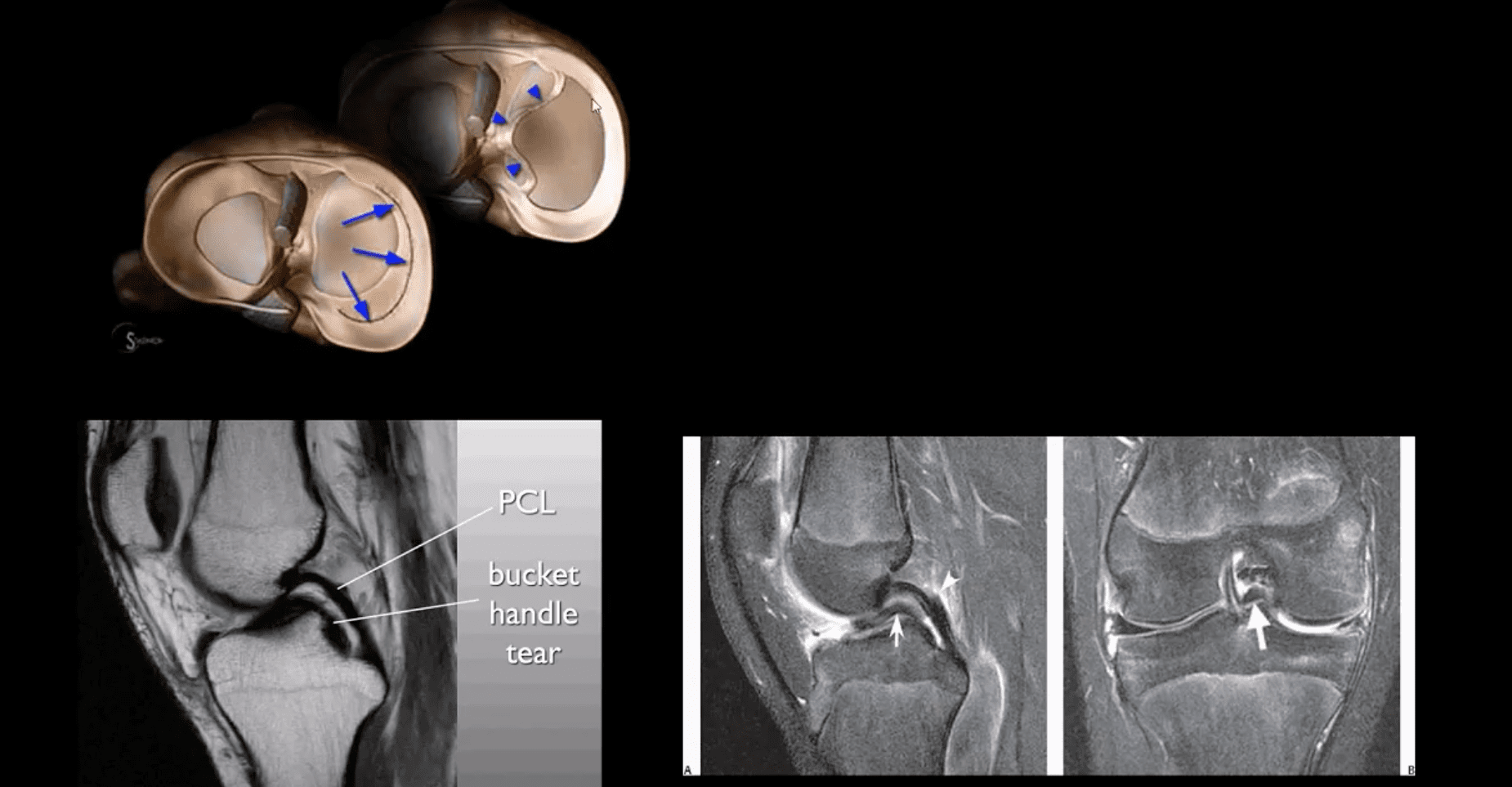
Bucket Handle Tear
- Bucket handle tear are m/c in the medial meniscus esp. with acute ACL and MCL tear
- MRI signs; double PCL sign on sagittal slices
- Absent "bow-tie" sign and others
- Most cases require operative care
DDx From Meniscal Degeneration

- Occasionally meniscal tears need to be DDx from meniscal degeneration which may also appear bright (high signal) on fluid-sensitive MRI
- The simplest rule is that if there is a true meniscal tear aka Grade 3 lesion, it always reaches/extends to the tibial plateau surface
The Role of MSK Ultrasound (US) in Knee Examination
- MSK US of the knee permits high resolution and dynamic imaging of primarily superficial anatomy (tendons, bursae, capsular ligaments)
- MSK US cannot adequately evaluate cruciate ligaments and the menisci in their entirety
- Thus MR imaging remains modality of choice
Potential Pathologies Successfully Evaluated by MSK US
- Patellar tendionosis/patellar tendon rupture
- Quadriceps tendon tear
- Prepatellar bursitis
- Infrapatellar bursitis
- Pes Anserine bursitis
- Popliteal cyst (Baker cyst)
- Inflammation/joint effusion with synovial thickening and hyperemia can be imaged with US (e.g., RA) especially with the addition of color power Doppler
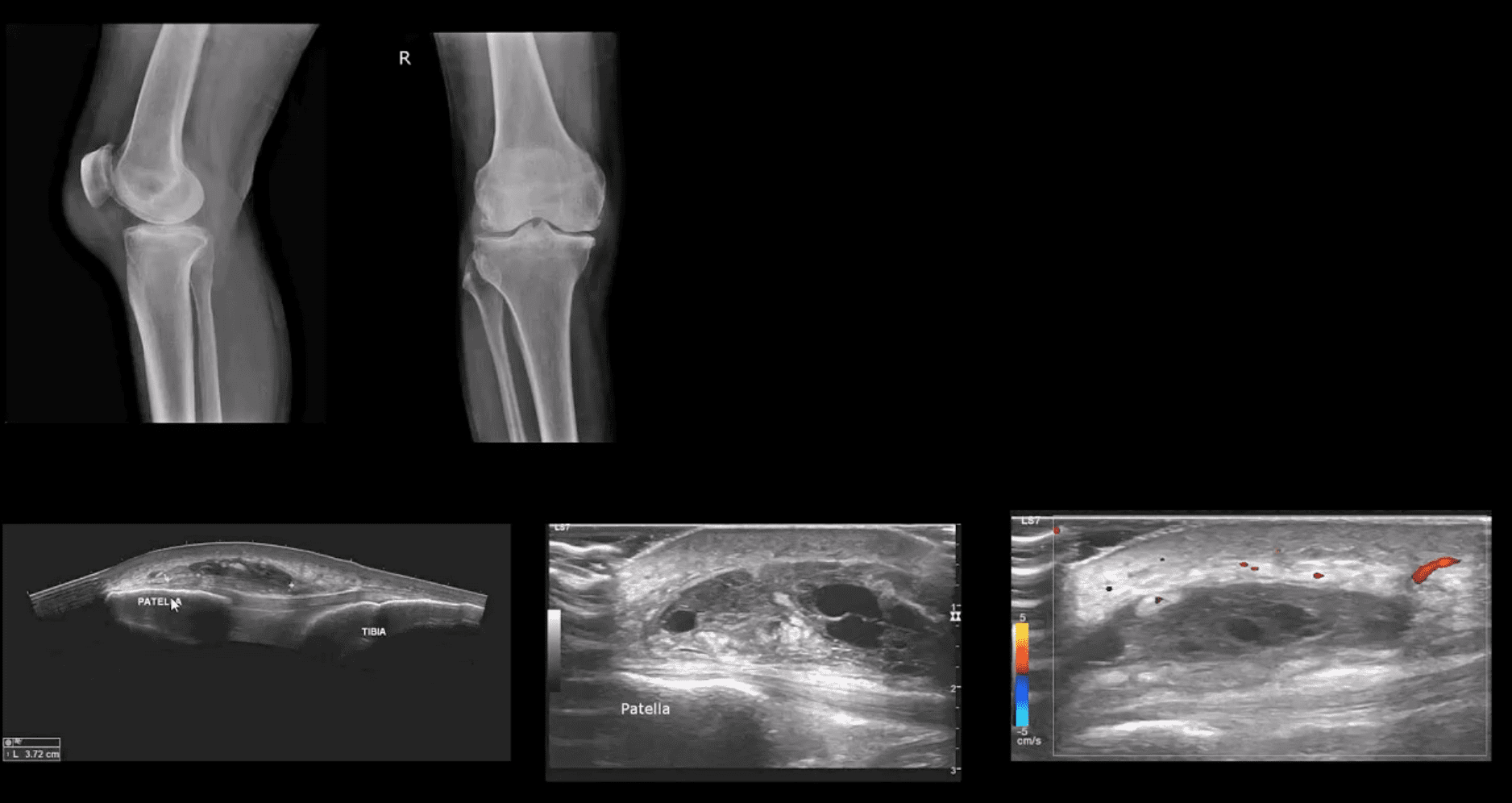
Patient Presented With Atraumatic Knee Pain & Swelling
- Radiography revealed sizeable soft tissue density within the superficial pre-patella region along with mild-to-moderate OA
- MSK US demonstrated large septated heterogeneous fluid collection with mild positive Doppler activity on the periphery indicating inflammation d/t Dx of Superficial pre-patella bursitis
Long Axis US Images
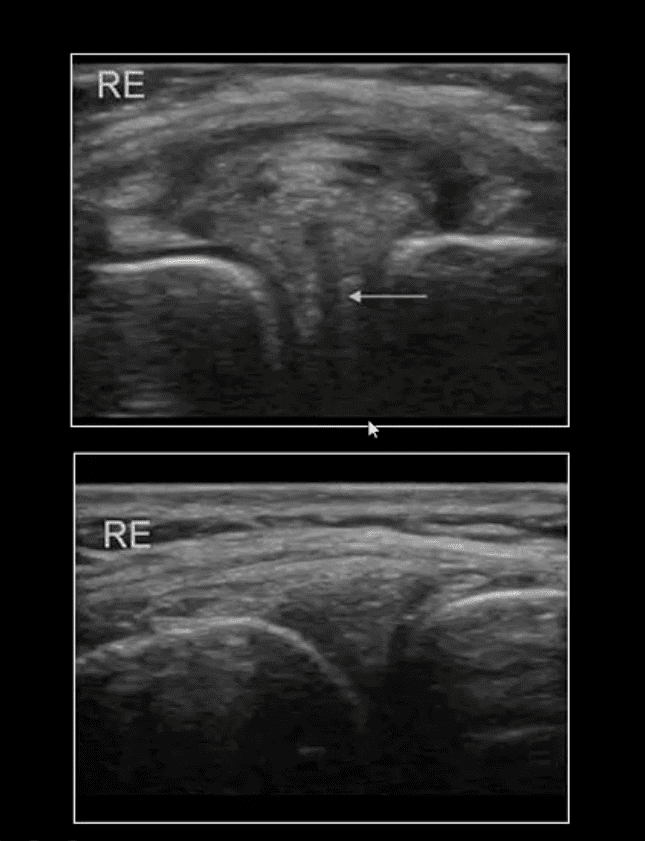
- Note normal lateral meniscus and fibers of LCL (above bottom image) compared to
- Horizontal degenerative cleavage tear along with protrusion of lateral meniscus and LCL bulging (above top image)
- Major limitation: unable to visualize the entire meniscus and the ACL/PCL
- MRI referral is suggested
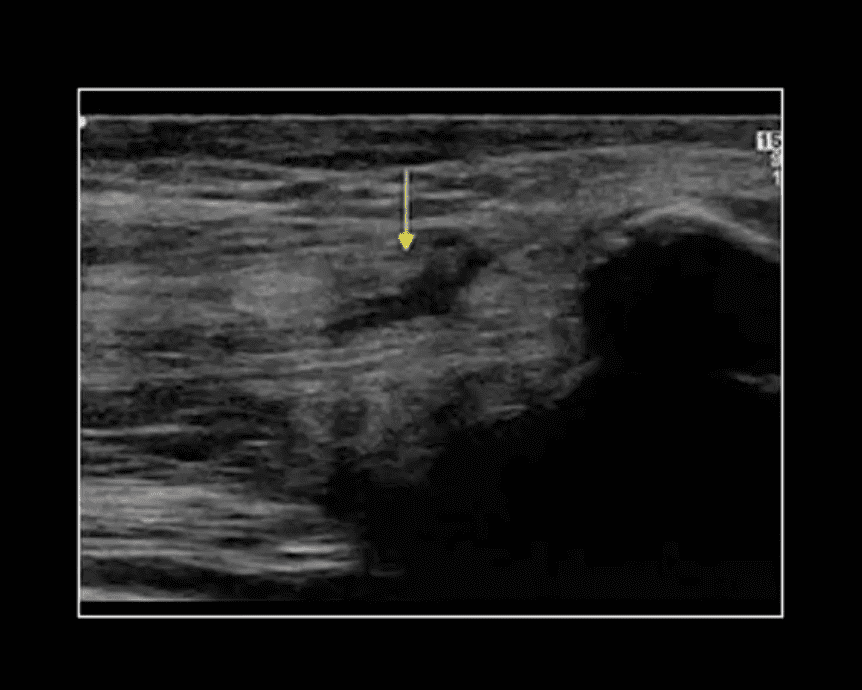
Rupture of Distal Tendon of Quadriceps
- Note rupture of distal tendon of the Quadriceps muscle presented as fiber separation and fluid (hypo to anechoic) fluid collection within the substance of the tendon
- Advantages of MSK US over MRI to evaluate superficial structures:
- Dynamic imaging
- Availability
- Cost-effective
- Patient's preparation
- Disadvantages: limited depth of structures, inability to evaluated bone and cartilage, etc.
Osteochondral Knee Injuries (OI)
- osteochondral knee injuries can occur in children 10-15 y.o presented as Osteochondritis Dissecance (OCD) and in mature skeleton m/c following hyperextension and rotation trauma, particularly in ACL tear.
- OCD-typically develops from repeated forces in immature bone and affects m/c postero-lateral portion of the medial femoral condyle.
- OI in mature bone occurs m/c during ACL tears mainly affecting so-called terminal sulcus of the lateral femoral condyle at the junction of the weight-bearing portion opposed to the tibial plateau and the part articulating with the patella
- Osteochondral injuries may potentially damage the articular cartilage causing secondary OA. Thus need to be evaluated surgically
- Imaging plays an important role and should begin with radiography often followed by MR imaging and orthopedic referral.
OCD Knee
- 95% associated with some trauma. Other etiology: ischemic bone necrosis especially in adults
- Other common location for osteochondral injuries: elbow (capitellum), talus
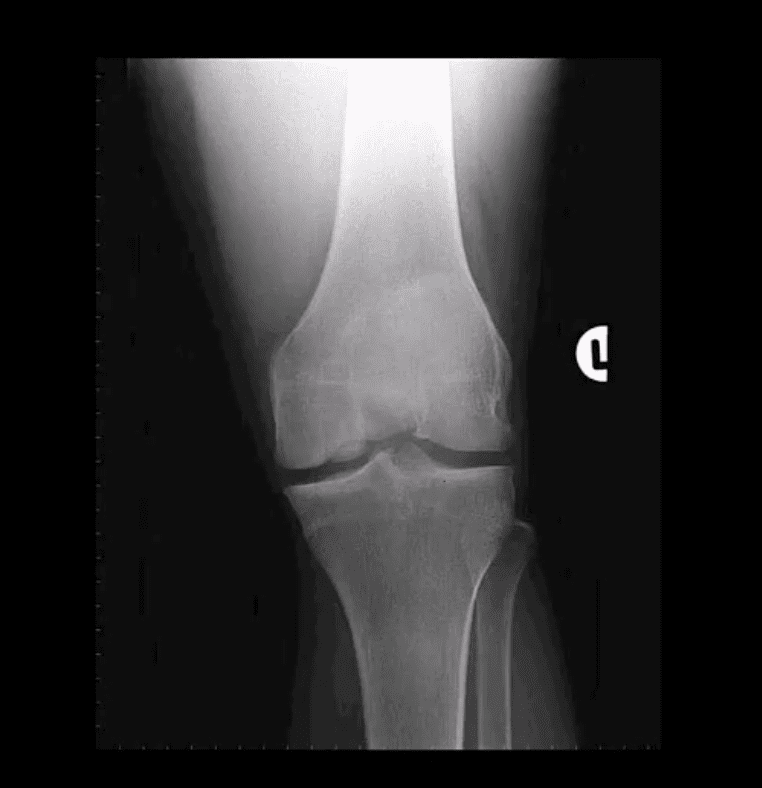
- 1st step: radiography may detect osteochondral fragment potentially attached or detached
- Location: the posterior-lateral aspect of the medial femoral condyle. Tunnel (intercondylar notch) view is crucial
- MRI: modality of choice >90% specificity and sensitivity. Crucial for further management. T1-low signal demarcating line with T2 high signal demarcating line that signifies detachment and unlikely healing. Refer to orthopedic surgeon
- Management: stable lesion esp. in younger children>off weight-bearing-heals in 50-75%
- Unstable lesion and older child or impending physeal closure>operative fixation.