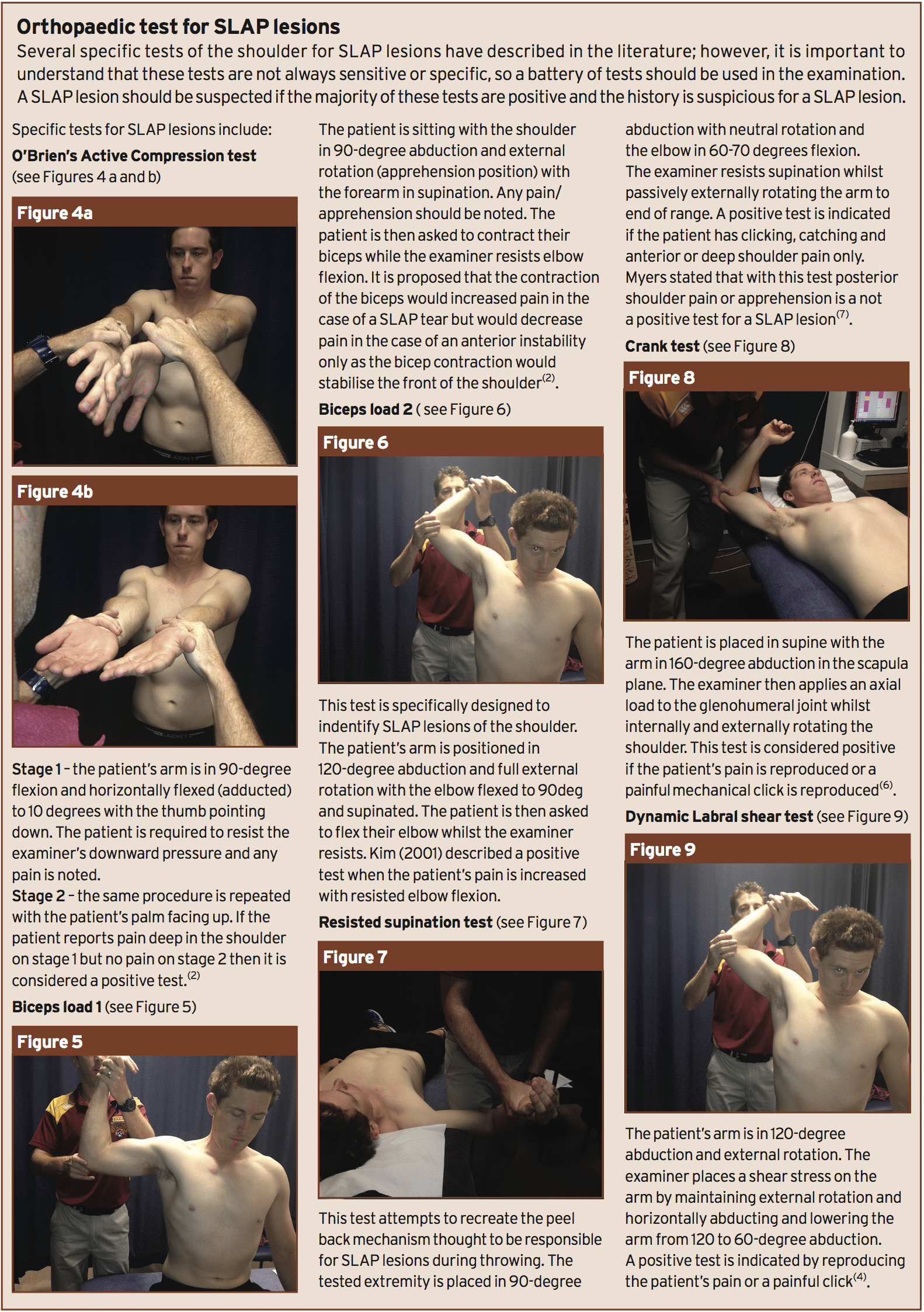
Science based therapist, Dr. Alexander Jimenez looks at the several types of SLAP lesions, a few frequent clinical indicators, orthopedic evaluations and explores the very best rehab methods...
Overhead athletes (like baseball pitchers, tennis, swimming, water polo and throwing athletes). All put enormous strain on their shoulders when participating in their chosen sport. An elite baseball pitcher's arm was listed at over 7000deg/second which puts it arguably as the fastest human body movement in game. This all happens at a joint that's been likened to a golf ball sitting on a tee -- ie it is structurally unstable. Considering all of this, is it any wonder that shoulder pain is a common occurrence in the overhead athlete? Throwers with shoulder pain will often complain of a "dead arm" which restricts them from throwing at pre-injury velocity/or control. SLAP (Superior Labrum Anterior-Posterior) lesions are common causes of this "dead arm" and will be the focus of this article.
What Is A SLAP Tear?
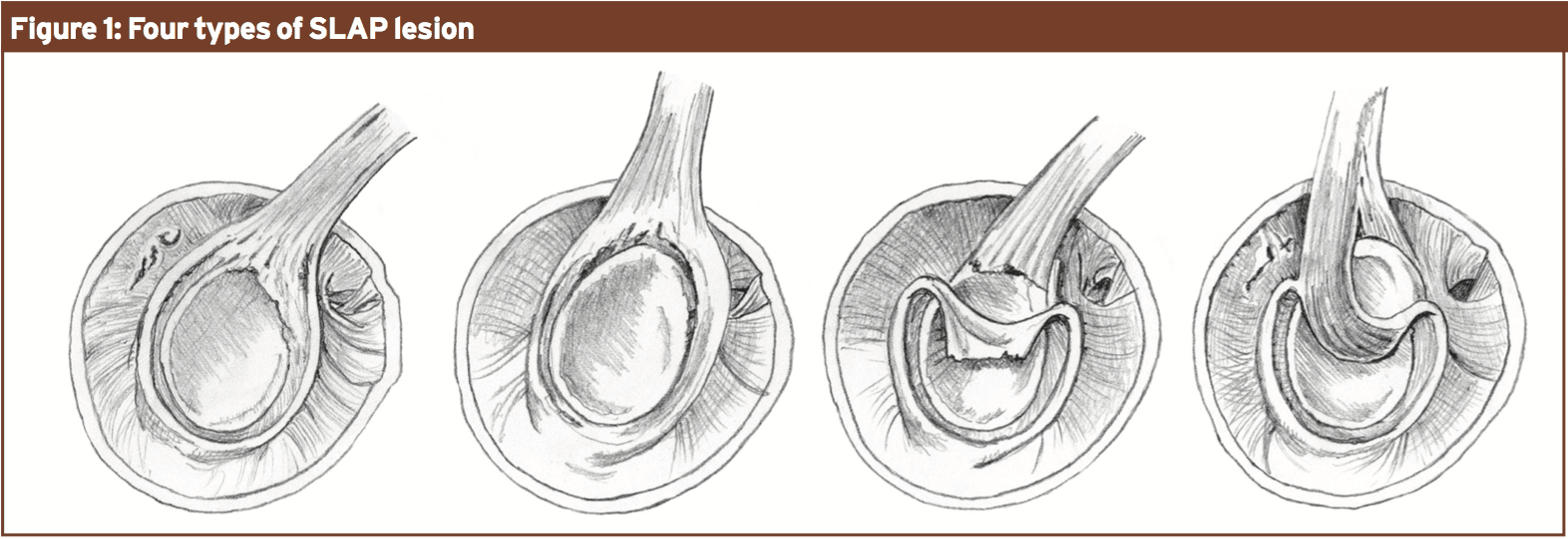
A SLAP tear is a tear of the glenoid labrum from anterior to posterior of the long head of biceps tendon. The glenoid labrum is a wedge-shaped fibrous tissue structure that's attached to the edge of the glenoid and its function is to weaken the glenoid cavity, thus improving stability, and it also has a role in muscle control and proprioception(1). The anatomy of the proximal long head bicep tendon is variable but typically it is derived from the posterior superior labrum and is wider and more densely innervated with sensory fibers compared to its distal tendon(5). Snyder has described four main subgroups of SLAP lesions(4) (see Figure 1):
Type 2 – involves detachment of the superior labrum and long head biceps tendon from the glenoid rim. This is the most common type of SLAP lesion causing symptoms and often requires surgery.
Type 3 – the meniscoid superior labrum is torn away and displaced into the joint but the tendon and labral rim attachment remains intact.
Type 4 – the tear of superior labrum extends into the tendon, part of which is displaced into the joint
along with the superior labrum.
What Is The Mechanism Of Injury?
The exact mechanism still remains controversial with three major theories present. The deceleration theory initially proposed that in a throwing athlete a SLAP lesion happened during the deceleration phase of projecting as a result of eccentric contraction of the biceps tendon(7). They suggested that this overloaded the biceps anchor that detached it from its intra- articular attachment. A direct blow to the shoulder has also been believed to be a cause for a SLAP lesion -- for instance, an athlete landing in an outstretched arm might compress/pinch the labrum between the glenoid and the humerus(1). More lately, Burkhart described the acceleration or "peel back mechanism" which occurs when the arm is at the cocked position of abduction and external rotation. They explained that during arthroscopy in shoulder abduction and external turning the thoracic fascia presumes a more vertical and posterior angle which generates a twist at the bottom of their biceps and a torsional force on the anterior superior labrum(1).Kuhn experimentally compared the deceleration and acceleration theories in cadavers models(1). They applied a brute force to the biceps tendon from the follow through place and were able to generate a superior labral avulsion in 20% of his specimens with a massive push. To simulate the peel back mechanism they placed the arm at an abducted and externally rotated position. In 90% of the shoulders analyzed, they could create a type 2 SLAP lesion with 20 percent less force than at the deceleration version. From this it can be proposed that the peel back mechanism is more likely to cause a SLAP lesion than the deceleration model and that the bicep tendon is not pulled but peeled from the bone.
What Is The Clinical Presentation?
Subjective
Athletes who have a SLAP tear will often describe pain deep in the shoulder and it can be anterior or posterior. A throwing athlete may describe weakness when they throw and may state that they have lost their “zip”. Often the athletes may still throw, but maybe not at their normal velocity. They may describe a history of tightness on the back of their shoulder and pain/ weakness at the front especially within the coracoid process area(8). They may also clarify a click or pop when they toss and it is important to ascertain whether these symptoms are fresh and/or are painful. From the throwing athlete, it's important to inquire when exactly from the casting action they obtain their pain. As outlined earlier, an athlete that has pain/weakness at the late night phase may have a SLAP tear whereas an athlete who merely explains pain on follow-through may be more inclined to have impingement-type pain.
Objective
Standing Posture
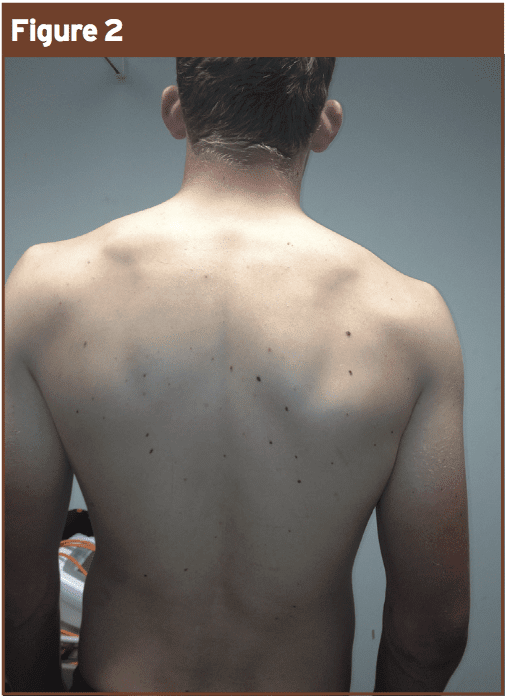
Ordinarily, overhead athletes with SLAP tears will have poor scapula position at rest on their dominant side: Figure 2 shows inferior scapula position in a right-arm thrower. Burkhart explained this asymmetrical scapula position as with a SICK (Scapular malposition, Inferior border prominence, Coracoid pain and dysKinesis of scapula motion) scapula(3). It is also important to note thoracic posture, as increased kyphosis and lack of trunk rotation can also increase load on the shoulder when throwing.Shoulder ROM
Active ROM of the shoulder must then be assessed to ascertain any motion restriction or pain. Glenohumeral rotation range ought to be assessed in all overhead athletes. A thrower's shoulder needs to have enough laxity to allow for excessive external rotation (demand of good throwing) with adequate dynamic stability to avoid subluxation. Glenohumeral rotation array is conventionally done in supine with the arm in 90-degree abduction. Commonly these athletes will get an increase in external rotation range (possibly due to repetitive stretching of their anterior capsule at the cocking phase and/ or humeral retroversion when they threw a lot if they were young) and a drop in internal rotation range. This absence of internal rotation range is frequently due to contracture of the posteroinferior capsule contracture and is popularly known as GIRD (Glenohumeral Internal Rotation Deficit). Sleeper stretches (see Figure 3) have been demonstrated to not only reduce GIRD but also to reduce shoulder injuries by around 40% in major league baseball players(1).Treatment
A Case Study
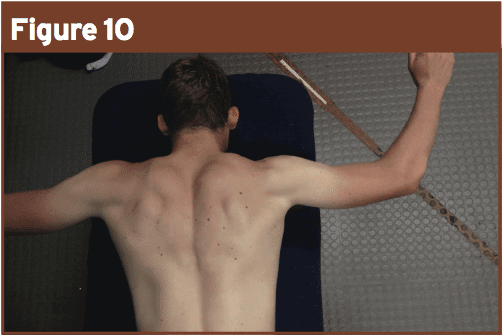
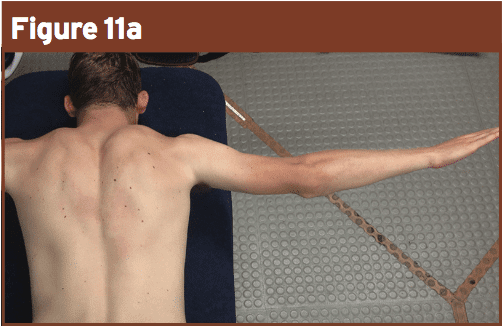
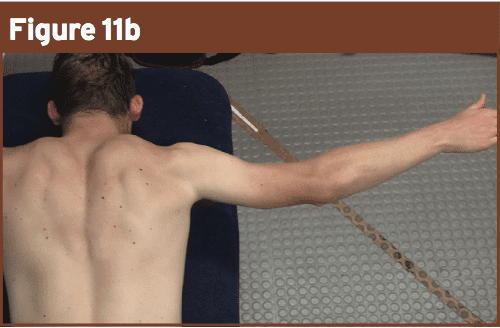
Shoulder injuries in the throwing athlete would be initially managed with conservative therapy with therapy focused on improving GIRD and/ or scapula control. In most cases the whole kinetic chain should be assessed and proper exercises should be implemented based upon the requirements of their game.Figure 2 reveals a cricketer who bowls and throws with his right arm. When I first saw him, he complained of pain and "fatigue" in his shoulder when he bowled and threw from the boundary. He also had pain through range on abduction, which resolved if his scapula position was fixed (posterior tilted). He had no reduction of glenohumeral range on his right side. In this case (because of the success of posteriorly tilting his scapula on his pain through the evaluation) treatment focused on lengthening techniques of the muscles that anteriorly tilt his scapula, ie pec minor, and strengthening for his lower and middle trapezius that help to posteriorly tilt his scapula. This player was given a range of exercises in prone to improve his scapula position (see Figures 10 - 11).
Conservative treatment isn't always effective especially if a type 2 SLAP lesion is current. In such cases operative therapy is required and the athlete can take 9-12 months to return to sport and they'll report that it requires up to two years to go back to their pre-injury level.
Conclusion
In summary, SLAP lesions are typical in the overhead athlete and a structured evaluation particularly looking at scapula control, glenohumeral rotation range in addition to orthopaedic tests can help to identify when a SLAP lesion is current and will also help direct therapy. Frequently in elite-level athletes, particularly when a type 2 lesion is present, surgery is needed(4).References
1. Burkhart S, Morgan C, Kibler B (2003) The disabled throwing shoulder: Spectrum of pathology, Part 1: Pathoanatomy and Biomechanics. Arthroscopy: the Journal of arthroscopic and related surgery, Vol 19, No4, 404-420
2. Burkhart S, Morgan C, Kibler B (2003) The disabled throwing shoulder: Spectrum of pathology, Part 2: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy: the Journal of arthroscopic and related surgery, Vol 19, No5, 531-539
3. Burkhart S, Morgan C, Kibler B (2003) The disabled throwing shoulder: Spectrum of pathology, Part 3: The SICK scapula, scapula dyskinesis, the kinetic chain and rehabilitation. Arthroscopy: the Journal of arthroscopic and related surgery, Vol 19, No6, 641-661
4. Brukner P and Khan K (2012) Clinical Sports Medicine 4th edition McGraw Hill
5. Krupp R et al (2009) Long head of bicep tendon pain: differential diagnosis and treatment. Journal of orthopaedic and sports physical therapy Vol 39, no 2 55-70
6. McFarland E, Tanaka M, Papp D (2008) Examination of the shoulder in the overhead and throwing athlete, Clinical Sports Medicine 27, 553-578
7. Myers T et al (2005) The resisted supination external rotation test; A new test for diagnosis for SLAP lesions, the American Journal of Sports Medicine, Vol 33, No9 1315-1320
8. Ryu J, Pedowitz R (2010) Rehabilitation of bicep tendon disorders in athletes. Clinical Sports medicine 29 229-246