This case study has one of those treatment results that makes you believe you've made a massive difference to somebody's life. Scientific injury specialist, Dr. Alexander Jimenez investigates the case research.
This patient, Mel, loves mountain running. Much of her week revolves round instruction, getting ready for the long term in the weekend, and finally the large competition. I first analyzed her about six weeks out from a race called the Kokoda Challenge, a 96km team race. She was fighting with just two complaints. The first, and lesser, was repeated ankle sprains on both legs; the second has been chronic iliotibial band (ITB) problems, again on both sides. Though these are clearly two distinct issues, they are not entirely separate, as we will see.
Mel was always running on uneven, rocky ground and would roll her ankles several times during training and competition run. On assessment, she demonstrated laxity on both ankles from the anterior talofibular ligament (ATFL, the most commonly strained ligament of the ankle). There was no joint effusion or pain, just increased plantar flexion and inversion and increased joint movement on the ATFL anterior pull test.
Her proprioception was, to put it mildly, terrible. When balancing on one foot, then she'd eliminate balance immediately upon closing her eyes. She was not able to balance on the ball of her foot on one leg, and could not grip balance on one leg when utilizing any balance device such as a wobble board or Bosu ball.
The immediate goal was to stop her rolling her ankles, to prevent long-term joint damage and, importantly, to lower the risk of a serious acute ankle injury -- a risk that is clearly inherent in the nature of her chosen sport. The answer was straightforward: we needed to retrain Mel's proprioception.
And now to Mel's ITB problems. She'd suffered from lateral knee pain for approximately a year. She had fought through the pain in training; it'd come on after distinct distances, but would usually start when she had been going downhill.
Since she had had this problem for quite a very long time and past remedy hadn't been successful, an MRI was indicated; this revealed irritation of this under-surface of the ITB and some quite mild bony inflammation at the lateral femoral condyle. In consultation with all the sports physician, we determined that a cortisone shot would be appropriate. This would permit Mel to carry on doing some running and create a window for a few rehab work. Mel, however, wasn't keen on the concept of an injection and preferred to attempt rehab alone first.
Upon evaluation, she'd just moderate tensor fascia latae, hip flexor and ITB tightness, which we handled with soft tissue massage, trigger points and extending. But these measures didn't actually target the underlying difficulty. Mel managed to continue doing and running her rehab but with the continuing deficit within her range of motion. Back in 1994 Bullock-Saxton, Janda et al (1) revealed that the substantial difference in patterns of muscular activation around the hip in normal subjects in comparison to people who had previously suffered a serious ankle sprain. They revealed that activation of gluteus maximus was postponed on the previously injured side which changes happened in the neighborhood perception of vibration on both the injured and non-insured sides.
On testing, Mel's gluteus maximus activation was very poor. In more than hip extension, it had been nearly non-existent and she fought with another hip expansion- dominant exercise.
And she was finding single-leg stance exercises hard not only because of her lack of proprioception but also because of poor gluteus medius function, evident in isolated hip abduction in side lying, and single-leg posture exercises.
To sum up, Mel, who had been attempting to compete in endurance mountain races, had:
• chronic ATFL laxity
• ITB friction syndrome confirmed by MRI
• poor proprioception
• poor gluteus maximus and medius function anterior and lateral tightness.
• ITB friction syndrome confirmed by MRI
• poor proprioception
• poor gluteus maximus and medius function anterior and lateral tightness.
Her running gait represented this great deal perfectly. She conducted with a lengthy stride length. Her heels strike occurred way out before her hip (rather than beneath it), constantly putting gluteus maximus into a lengthened position. This was making it more challenging for the muscle to contract and extend the hip. So Mel was pulling herself along with her hip flexors and rotating her pelvis with a rather forceful hip extension so that she could propel her body forwards at heel strike.
Due to her long stride length, she crossed her midline by a massive level, ramping up the demand on her already weak gluteus medius. It wasn't surprising that in stance stage her pelvis exhibited considerable lateral tilt.
It's worth mentioning that elite runners also often drift across the midline, since they, also, run with a long stride length. The difference is that their greater stride length comes from their strong propulsion through each stride; heel-strike remains firmly beneath the hip.
Not only does a running gait such as Mel's lead to harm, but it is also very inefficient. Because her posture stage was very lengthy, any elastic energy saved from the initial ground contact was lost, causing her to have to work harder to transfer energy with every stride.
That is the reason elite runners tend not to have a heel-toe working routine: they are moving so efficiently that a heel-toe pattern could cause them to spend too long on the floor and therefore lose too much energy. A key aim of all runners -- out of track to marathon -- ought to be to reduce ground contact time, so as to boost efficiency and hence speed.
Rehab
Mel did not want to quit running, despite pleas, because running was more than just exercise for her. Much like many people, it was her solitude and anxiety relief. We had to prioritize proprioception, to attempt to improve this until she suffered a severe ankle injury.We began with low-level workouts, for example:
• balancing on one foot with eyes closed for 2 sec at a time
• single-leg balancing with small heel raises, using support as needed.
We progressed this to:
• increasing the time and height of the heel raises
• single-leg balancing while throwing a ball.
We further progressed to:
• single-leg knee bends with eyes closed
• hopping drills, eg on-the-spot, around cones, in patterns, hopping then holding balance on the ball of the foot. As Mel improved, we were able to introduce external devices to overload the proprioceptive system: a soft mat, wobble board and Bosu ball.
Other high-level exercises included:
• balancing on a wobble board while throwing and catching a ball
• single-leg knee bends on the Bosu ball.
• single-leg balancing with small heel raises, using support as needed.
We progressed this to:
• increasing the time and height of the heel raises
• single-leg balancing while throwing a ball.
We further progressed to:
• single-leg knee bends with eyes closed
• hopping drills, eg on-the-spot, around cones, in patterns, hopping then holding balance on the ball of the foot. As Mel improved, we were able to introduce external devices to overload the proprioceptive system: a soft mat, wobble board and Bosu ball.
Other high-level exercises included:
• balancing on a wobble board while throwing and catching a ball
• single-leg knee bends on the Bosu ball.
• balancing on a wobble board while catching and throwing a ball
• single-leg knee bends on the Bosu ball.
There are just two major goals with proprioceptive training. Firstly, to improve the role of the proprioceptive system with increasingly more difficult activities and secondly (especially essential in Mel's situation, as she had been running long distances on uneven ground), to increase the endurance of their neuromuscular system.
We started her on non invasive activation drills because of her gluteus maximus and gluteus medius. For the glute maximum, she needed to lie prone and practice squeezing left and right glutes together and then isolating each side.
This progressed to prone hip extension, focusing on isolating glute max contraction while maintaining neutral pelvis and spine. Mel also did single-leg bridge exercises, again concentrating initially on squeezing the glute maximum and then extending the hip, but not arching the lumbar spine. We encouraged her to concentrate on feeling like she had been tripping her gluteus maximus in walking and specifically on staircase.
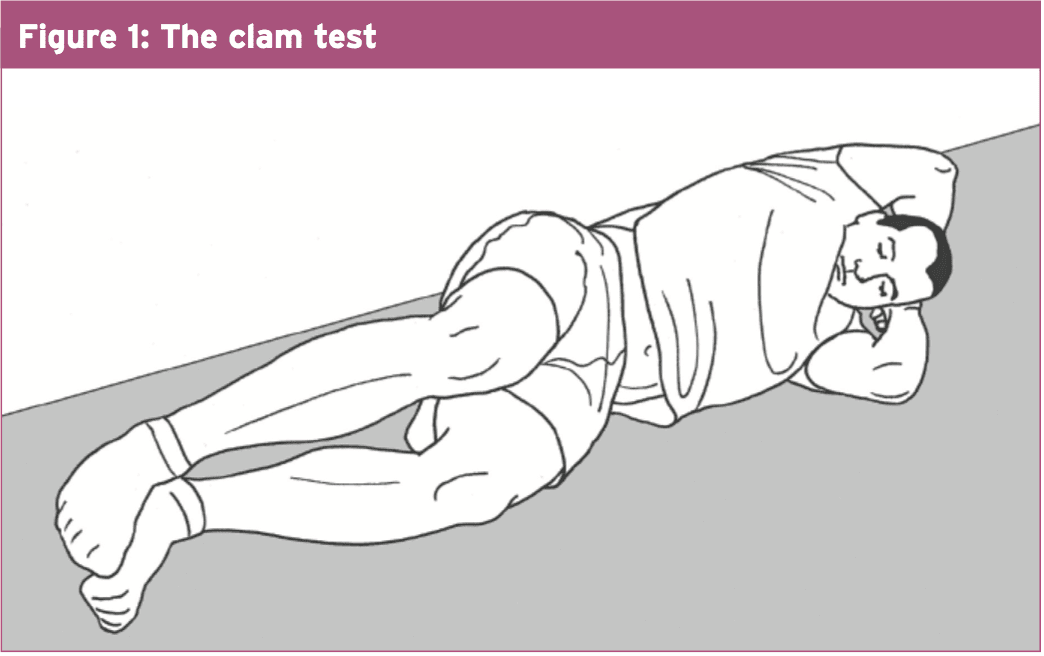
For gluteus medius activation, we utilized clams (side-lying with hips flexed to 30°, heels together and lifting top knee apart without the pelvis shifting; see Fig 1, below) and side-lying hip abduction with a straight leg.
We later introduced the technically demanding Romanian deadlifts (RDLs). These, I believe, are the ideal method for athletes to reinforce the gluteus maximus. Mel finally progressed to single-leg RDLs, an extremely ambitious exercise, which definitely must be worked up to.
Gluteus medius endurance bilaterally was worked on with "crab walk". This involves looping a flexband round the ankles in standing, assuming a semi-squat and widening the stance, then taking little sideways shuffling steps with one foot, then the other, while keeping up the strain on the ring. This impacts the gluteus medius muscles; it can be progressed by increasing the amount of steps or utilizing a more powerful group.
Not Any Old Exercises...
We tailored all of the strengthening exercises to suit Mel's specific sporting needs. She needed to possess exceptional endurance in all those critical muscles we were targeting if she had been going to keep an efficient gait through an occasion. Her program was so designed to signify this, with lower weights but higher repetitions (beginning at 15), and even more than the standard three sets. All these additional repetitions had the additional advantage of assisting her more quickly hard- wire the beneficial motor patterns.It also meant she had to work very hard indeed on her rehab. Especially during the late-stage rehab, the sessions were very arduous. But then, she wasn't trying to perform what could be considered normal for a 43-year-old girl. One bonus was that since the subsequent sessions were so tough, she had to take adequate recovery period, which restricted her into a maximum of 3 sessions weekly. Mel became technically very capable and powerful; she proceeds to perform her exercises frequently as maintenance.
Running Form
The running procedure re-education was quite simple. We focused on shortening Mel's stride and getting her to feel as though her heel strike was back beneath her body rather than straying over the midline. Next, she had to feel as though she immediately propelled her entire body over her foot, to make a decline in her ground contact time. We also cued her to feel her gluteus maximus contracting as she extended her hip. As she had good body awareness, this worked well for her. I also invited her to connect up the feeling she had been getting in the gym rehabilitation work together with how her gluteals were functioning in her running.But she wanted to try anyhow. As anticipated, she did not make it and her knees were an issue. But at least she'd ceased rolling her legs. She also began running again, with all the pain improving and still no rolling of their ankles. Mel had a favourite 18km training loop she liked to do regularly and she began running that pain-free -- that she had not been able to do for 12 weeks. Actually, she came to physio after one weekend hugely excited because she'd conquered her personal best by 10 minutes on her 18km training loop.
But the real test was yet to come: a 50km mountain run. This happened around three months after the Kokoda event. Mel ran powerful and pain-free. She was pumped.
Reference
1. Bullock-Saxton J, Janda V et al. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med 1994; 15: 330-334