Chiropractic back pain specialist, Dr. Alexander Jimenez looks at new study on muscle activation timing in the postural muscles and the implications for lower back pain in sportsmen and women.
Lower back pain (LBP) is a common illness among athletes (see Box 1). However, since our understanding of the etiology of back pain has improved, so have the prevention and treatment approaches. A good instance of this has been the growing emphasis throughout the last 15 years on functional training to the postural muscles of the back -- an approach to LBP treatment/prevention that's now quite widely recognized among clinicians and coaches. But though some research has emphasized advantages of the mode of training for those who have back pain and for carrying out regular activities, less research has been done on the benefits of core training for elite athletes and how this training ought to be carried out to maximize athletic operation. Really, there are many articles in the literature which promote core training programs and exercises for performance enhancement with no solid scientific rationale of their effectiveness, particularly in the sporting context.
Core Training & Muscle Activation
Many elite athletes undertake core stability and core strength training as part of their training program, despite contradictory findings and conclusions regarding their efficacy. This is principally due to the absence of a gold standard way of measuring core stability and strength if performing everyday tasks and sporting movements. A further confounding factor is that due to the diverse demands on the core musculature during regular tasks (low load, slow movements) and sporting activities (large load, resisted, dynamic movements), study conducted in the rehabilitation sector can't be put on the sporting environment and, subsequently, data regarding core training programs and their effectiveness on athletic performance are lacking.1 aspect of postural muscle function that has received special attention in recent years is muscle activation patterns. Understanding how a particular sort of movement triggers (or fails to trigger) postural muscles in the trunk is vital to unravelling the part of the postural muscles in trunk stabilization. Much of the initial work in this field has tended to focus mostly on the magnitude and patterns of electromyographic (EMG) activation in postural muscles, and this knowledge has proved invaluable to physiotherapists and sports physiologists looking for a better knowledge of LBP. More recently, there has been a developing interest in the timing of these action, and its connection to LBP.
The ability to rapidly modulate the timing of muscles in response to sudden postural perturbations is deemed paramount for maintaining posture and equilibrium, and thus in boosting good lower back health. The literature indicates that, in comparison with healthy controls, besides demonstrating reduced EMG activity, people with chronic LBP also demonstrate delayed activity reaction to both expected and unanticipated postural perturbations(4,5). Moreover, acute experimentally-induced LBP in healthy people has been proven to change trunk muscle activity during trunk flexion--extension, in addition to attaining and quick arm-movement tasks. Simply speaking, sufferers with acute or chronic LBP seem to be at increased risk of further injury in response to unexpected external perturbations(6,7).
Timing & Pain
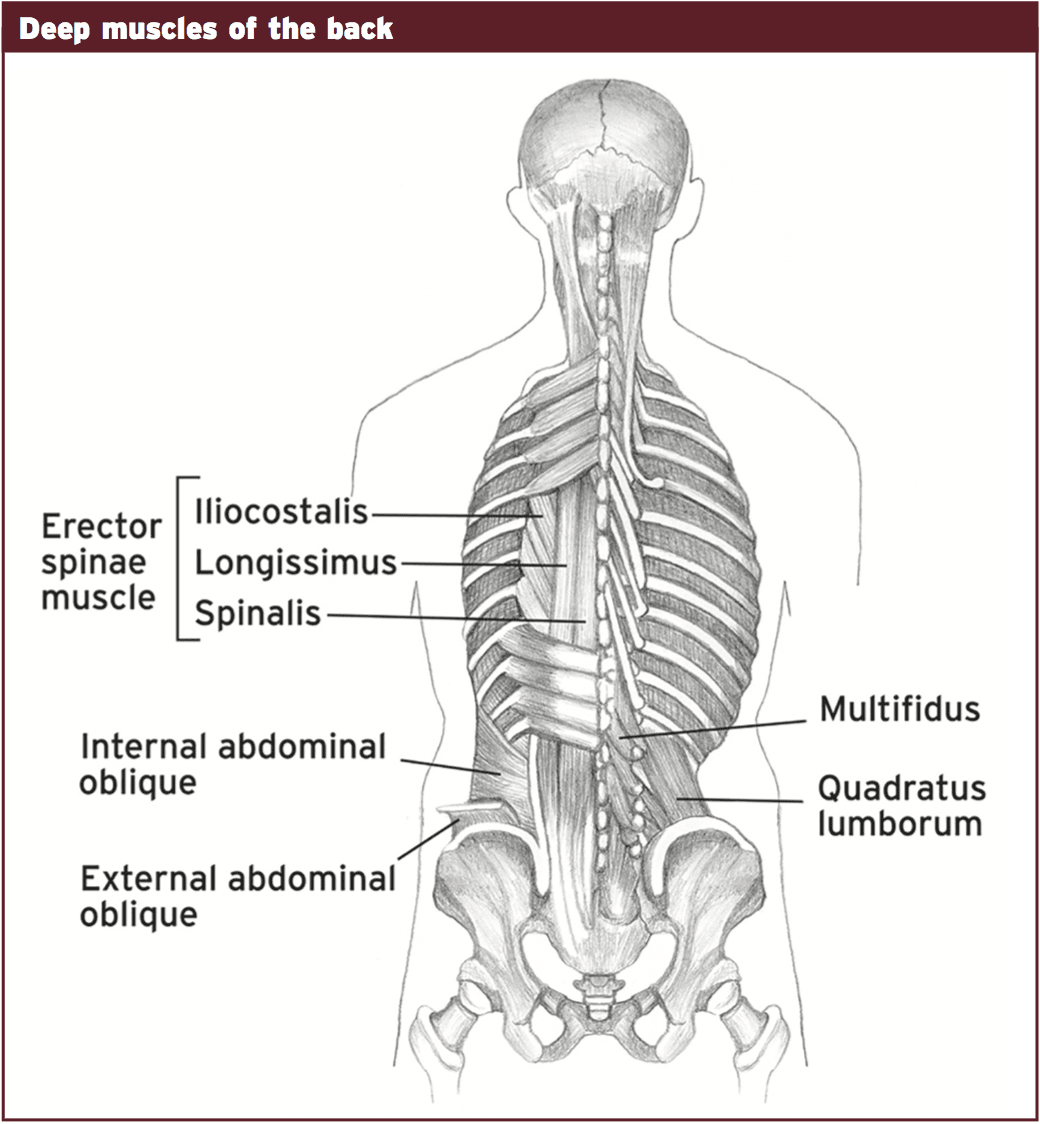
One criticism of these kinds of studies was that they employed protocols aimed at approximating 'real-life' perturbations but, in reality, these protocols were not sufficiently realistic to enable meaningful conclusions to be drawn. Nonetheless, these criticisms were answered by a 2011 study by Danish scientists, which examined automatic postural reactions in the presence of experimentally induced LBP to quickly, functionally applicable, complete body perturbations(8). These perturbations were created by a computer-controlled platform which enabled movement in 3- dimensions to generate tilting or sliding perturbations closely mimicking 'tripping over an obstacle' or 'slipping on a wet surface'.In the study, the researchers analyzed the activation of the erector spinae and external oblique muscles in response to unanticipated, bi-directional postural perturbations prior to and after the induction of acute LBP in healthy individuals. Each experimental session consisted of a baseline, control, and also an acute LBP condition. For the management and acute LBP condition, isotonic or hypertonic saline, respectively, was inserted to the ideal erector spinae muscle. In each condition, participants stumbled on a moveable platform during which 32 randomized postural perturbations were conducted. These consisted of eight repetitions of four perturbation types achieved within a period of 4-5 minutes -- 8cm anterior slides, 8cm posterior slides, 10 anterior tilts, and 10 posterior tilts. Throughout those perturbations, bilateral EMG was recorded by the erector spinae and external oblique muscles as well as the subjective pain experienced by these subjects.
The results demonstrated that compared to the 'no back pain' condition (control), back pain delayed the beginning time of both erector spinae and external obliques to the forward and backward slipping perturbations (although only the onset time of the erector spinae systematically varied with all the differing perturbation types and directions). It was also evident that in the back pain illness, the EMG amplitude was reduced bilaterally for all perturbations (see fig 1a 1d).
The results of this experiment indicated that the subjects with LBP exhibited:
● higher baseline EMG amplitudes of the erector spinae muscles before perturbation onset;
● fewer early-phase activations at the internal oblique and gastrocnemius muscles;
● fewer late-phase activations at the erector spinae, internal and external oblique, rectus abdominae, and tibialis anterior muscles;
● higher EMG amplitudes of the gastrocnemius muscle following the perturbation.
● higher baseline EMG amplitudes of the erector spinae muscles before perturbation onset;
● fewer early-phase activations at the internal oblique and gastrocnemius muscles;
● fewer late-phase activations at the erector spinae, internal and external oblique, rectus abdominae, and tibialis anterior muscles;
● higher EMG amplitudes of the gastrocnemius muscle following the perturbation.
Late Onset Muscle Activation In Athletes
The research above looked at start activation instances in (differently) healthy but sedentary individuals. But what are the consequences for athletes? Unfortunately, the literature in this regard is very thin on the ground. However, a brand new study published in 2013 has looked in the reflex reaction of shallow trunk musculature in athletes with chronic low back pain(10) to check whether similar patterns of delayed muscle activation onset exist within the athletic body. In particular, the investigators sought to compare long latency reflex response (happening between approximately within 40ms to 100ms) in athletes with chronic LBP against asymptomatic athletes.To do this, 24 athletes with chronic LBP were compared with 25 hepatitis athletes. At the position rankings, perturbations were introduced equally expectedly and unexpectedly while the surface EMG of the rectus abdominis and erector spinae muscles were listed. The latency of the onset of muscle activation and the root mean square (RMS) amplitudes within the response length were compared between the two groups.
In comparison with the asymptomatic athletes, the latency of onset has been postponed from the LBP athletes when the athlete underwent unexpected perturbations. However, during the anticipated perturbations, no modification was observed. The investigators went on to conclude that 'chronic LBP athletes exhibit a delay in onset latency to unexpected perturbations and decreased long latency response amplitudes to perturbation tasks compared to asymptomatic athletes. These modifications can induce athletes to recurrent low back pain and further injury.'
Questions
If muscle activation time is a significant element in LBP, an obvious question to ask at this stage is if a core training program (which often creates the staple of many a lower back injury rehabilitation program) can help normalize muscle activation patterns. There is a paucity of research in this area but a study published in 2012 is revealing(11). In this study, researchers sought to investigate feed- forward activation or timing of abdominal muscle activation in response to rapid spinal flexion following an eight-week plan of core stability exercises, sling exercises, or overall exercises.Of specific interest was the effect on muscle activation onset (listed bilaterally from m-mode ultrasound imaging) at the deep abdominal muscles in response to quick shoulder flexion in the chronic nonspecific LBP patients.
In the conclusion of the eight-week instruction period, there were only insignificant or very modest improvements in the LBP subjects. The baseline-adjusted 'between group' differences showed a 15 millisecond advancement with sling training relative to core stability training, and a 19 millisecond advancement relative to general exercise training. To put it differently, eight months of core stability training produced hardly any advancement in the start of abdominal muscle contractions.
Conclusion & Conclusion
Despite our growth in understanding along with the widespread take-up of core training work, low back pain is still a significant issue among athletes. Recent study on muscle activation patterns suggests that the late onset of stimulation in postural muscles is likely to be a contributing factor in the etiology of chronic low back pain and rehabilitation/ prevention programs relying only on core activation could be insufficient to help normalize postural muscle activity.References
1. Spine (Phila Pa 1976). 2004 Feb 15;29(4): 449-54
2. Neurosurg Focus. 2006 Oct 15;21(4):E7
3. Br J Sports Med. 2003 Jun;37(3):263-6
4. Brain Res 2001; 141:261–266
5. Spine 2000; (Phila Pa 1976) 25:947–954
6. Exp Brain Res 2003; 151:262–271
7. Spine 2007; (Phila Pa 1976) 32:E801–E808
8. Exp Brain Res 2011; 210:259–267
9. J Neurophysiol. 2011 Nov;106(5):2506-14
10. J Back Musculoskelet Rehabil. 2013 Apr 29. [Epub ahead of print]
11. Spine (Phila Pa 1976). 2012 Jun 1;37(13): 1101-8