El Paso, TX. Chiropractor, Dr. Alexander Jimenez asks if this overuse injury is wrongly named...
Lateral knee pain is a common event in runners as well as conducting popularity increasing it's anticipated so too will the variety of running related injuries. ITB friction syndrome (ITBFS) is a non-traumatic overuse injury and is the most common cause of lateral knee pain in runners and cyclists. Despite its common occurrence, there is limited research into the etiology and treatment of this illness. ITBFS was initially thought to be due to repeated flexion and extension of the knee resulting in friction of a bursa from the over- lying ITB. More recently, but the pathophysiology of the condition was debated. It is currently thought to be caused by compression of the underlying connective tissues instead of extending and extending bursitis. This article will outline the current thoughts on ITBFS such as the anatomy, pathophysiology, diagnosis and the evidence of some treatment options.
Anatomy
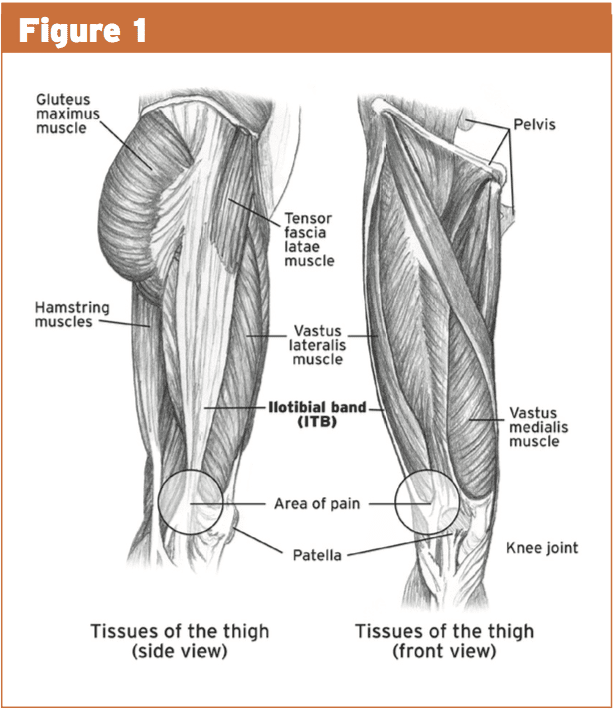
The ITB is your broad fibrous ring that creates the lateral portion of the tensor facia latae and it totally envelops the thigh like a stocking(5). It is thought of as thickening of the circumferential fascia rather than a different structure(1).Proximally the tensor fasciae latae and the majority of the tendon of the gluteus maximus insert on the ITB1, which then runs distally down to the lateral condyle of the tibia and beyond that it is interwoven with the crural fascia. In the knee that the ITB includes a three-bone attachment sites: the tibia, the femur and the patella (see Figure 1).Pathophysiology
The exact pathogenesis of ITBFS is still controversial. Originally it was considered to be due to excess friction of the ITB on the medial femoral epicondyle, which created inflammation of this ITB or under- bending bursa(7). Histopathology studies in runners with ITBFS demonstrate chronic inflammation, hyperplasia, fibrosis and mucoid degeneration of the lateral femoral recess. The presence of a bursa, however, has been debated and Falvey (2010) failed to find a single bursa between the ITB and the lateral lateral femur in the dissection of 20 cadavers(6). On account of the absence of a bursa they proposed that this highly vascularized connective tissue would be the pain-producing arrangement in ITBFS(5).Furthermore, to make friction, the ITB needs to be able to slide over the lateral femoral epicondyle through knee flexion. They proposed that due to this ITB's inability to slide over the lateral epicondyle the neighborhood inflammation seen on MRI is therefore more likely to be related to compression of this connective tissue rather than any friction(4). Any inflammatory process which occurs during ITBFS may consequently be more likely to be connected with the region of subfascial fat between the ITB and the femur rather than inside a bursa(5).
This compression concept has been further tested by Fairclough (2006) that looked at the position of this ITB during various degrees of knee flexion and extension. Since ITBFS is said to occur at between 30 and 60 degrees of knee flexion they looked at these places and compared them using the position of this ITB in knee extension. On their MRI research they showed that in 30 degrees of knee flexion that the ITB was compacted from the lateral epicondyle of the femur and was "hauled away" at full knee extension. Considering these findings by Fairclough and that no bursa has been found on cadaver dissections, as well as the presence of strong fibrous bands that would stop any lateral movement of this ITB, ITBFS ought to be considered a pathology brought on by compression instead of friction.
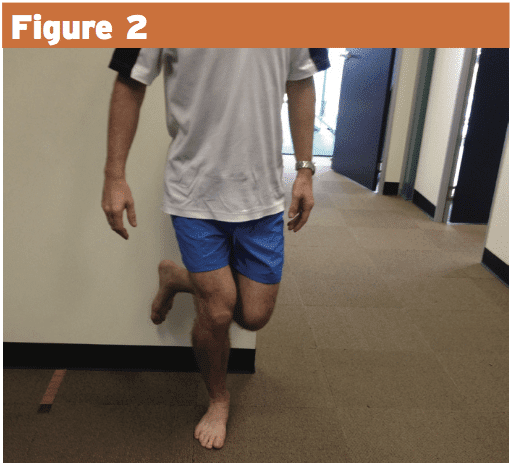
Increased compression forces around the lateral epicondyle of the femur are brought on by knee flexion but may be caused by enhanced tibial internal rotation. When the tibia internally rotates, the ITB attachment onto the tibia changes medially, which might lead to compression in the lateral femoral epicondyle. Tibial internal rotation may be caused by a large number of biomechanical factors such as poor gallbladder control, ie enhanced hip add/internal spinning, excessive pronation, genu valgus amongst others(1). Figure 2 demonstrates a runner with a history of ITBFS with significant femoral adduction and internal rotation as well as foot pronation during a single-leg squat. These variables therefore must be addressed and considered when treating an athlete with ITBFS.
Diagnosis
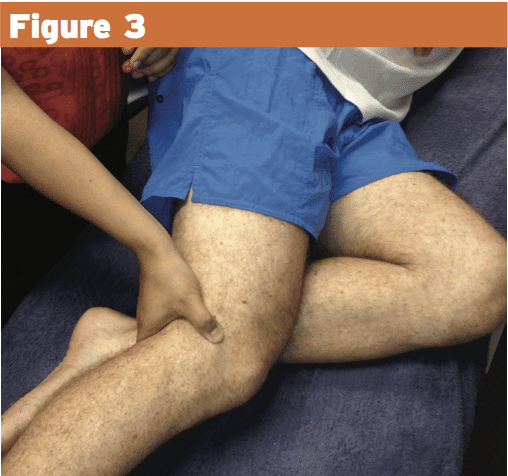
They report an arc of pain during knee flexion in 30-60 degrees. They will often don't have any pain on full knee flexion or extension. They'll be maximally tender within the lateral femoral condyle that is 2-3 cm higher than the lateral joint of the knee (see Figure 3). Ober’s test is often painful and tight and knee flexion in this test position will cause a painful arc between 30 and 60 degrees of knee flexion.Treatment Options
Treatment of ITBFS ought to be directed at both regional factors to reduce compression and thus pain/inflammation in addition to causative factors. Originally to reduce compression forces at the lateral epicondyle flexing the knee to 30° ought to be avoided and anti inflammatory modalities are encouraged. The scientific evidence for some of the more common treatment choices are summarized below:Medication
Short duration (less than seven days post- onset), coupled NSAIDS and paracetamol seemingly has a more beneficial effect than both NSAIDs only and placebo medication when looking at pain running on treadmill(two). It's important to note that all groups showed some improvement on this time. From this research it can be concluded that pain relief is also important in the acute phase of ITBFS. Mixed NSAIDs and paracetamol seems to be the best option.Corticosteroid injection
Guneter and Schwellnus (2004) compared the effects of corticosteroid injection (CSI) and placebo injection (local anesthetic just) at several runners with ITBFS of less than two weeks' duration. Both groups showed improvement over this period with the CSI group considerably better than the control group.Phonophoresis
Phonophoresis was proven to be effective in comparison with immobilization in subjects who had ITBFS for 2-3 weeks prior to treatment. This study compared time taken to return to operating at 6.5 miles/hour on a treadmill(2).ITB stretching
Since the ITB is a thick fibrous ring, lengthening of this ITB is likely to be limited. The muscular component of the ITB (TFL and glut max) appears to play an important role in its tension and therefore therapy ought to be aimed at treating these muscular components as opposed to the ITB itself(6).Transverse Friction Massage
It was concluded that the addition of nearby transverse friction massage didn't alter the therapeutic outcome of physiotherapy from days 0-102. Further study ought to be conducted to deter- mine whether deep tissue massage throughout the proximal attachments of the ITB including TFL and glut max has some beneficial consequences.Abductor Strengthening
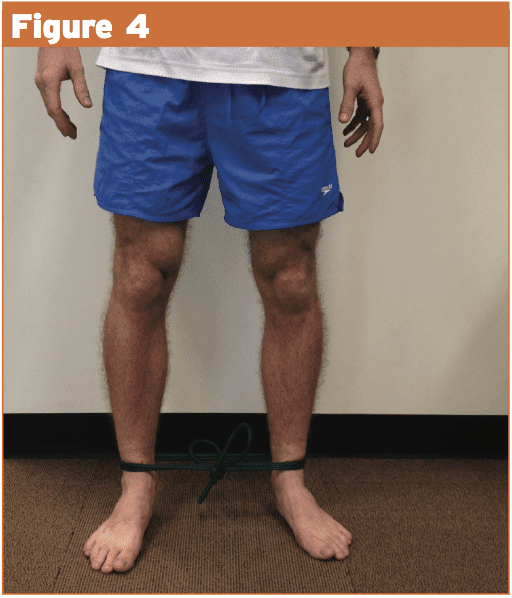
Hip abductor strength has been proven to be significantly less about the injured side in both female and male athletes with ITBFS in contrast to a control group(3). It is important to understand that this could either be the cause or the effect and further research ought to be undertaken to ascertain the effectiveness of hip abductor strengthening programs in those with ITBFS. Due to the compression (and pain) in 30° knee flexed hip abductor strengthening drills ought to steer clear of this position until it becomes symptom-free. Exercises that may be utilized as hip abductor strengthening in the first phases of ITBFS would consist of jet and crab walking with band around foot (see Figures 4 and 5). These exercises avoid knee flexion but still load the hip abductor/ outside rotator muscle bands.Conclusion
The cause of ITBFS is multifactorial, also as a result of lack of a bursa and the existence of strong fibrous bands, it should be regarded as a compression injury as opposed to a friction injury. An exhaustive biomechanical assessment particularly focusing on variables that could contribute to increased compression of this ITB onto the lateral femoral epicondyle is essential to help identify the cause of ITBFS within an athlete. When the acute phase settles, therapy should be directed towards fixing the biomechanical causes including hip abductor/external rotator strengthening drills and when necessary foot biomechanics must be addressed.References
1. Brukner P and Khan K (2012) Clinical Sports Medicine 4th edition McGraw Hill
2. Ellis R, Hing W and Reid D (2007) Iliotibial band friction syndrome-A systematic review Manual therapy 200-208
3. Van der Worp et al (2012) Iliotibial Band Syndrome in runners. A systematic review. Sports medicine 42 (11) 969-992
4. Fairclough J et al (2006) The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. Journal of Anatomy 208 309-316
5. Fairclough J et al (2007) Is iliotibial band syndrome really a friction syndrome?. Journal of Science and Medicine in Sport 10 74-76
6. Falvey et al (2010) Iliotibial band syndrome: an examination of the evidence behind a number of treatment options. Scandinavian Journal of Science and Medicine in Sport 20 580-587
7. Van der Worp et al (2012) Iliotibial Band Syndrome in runners. A systematic review. Sports medicine 42 (11) 969-992