Hip chiropractor and trauma specialist, Dr. Alexander Jimenez looks at among the most frequent causes of hip pain -- femoroacetabular impingement (FAI)...
Over the previous 10 years, with the advent of MRI and hip arthroscopy, the reported prevalence of hip labral and acetabular rim pathology has considerably increased(1). Hip pain is a common cause of reduction of training/game time with as much as 15 percent of all AFL injuries reported as hip pain(1).
What's FAI?
FAI happens when the femur impinges on the acetabulum. This happens due to an anatomical variation in either the femur or acetabulum and is present in up to 20% of the population.FAI is categorized into three main types (see Figure 1):
1) Cam impingement -- this is the most common type of FAI and is most often found in young males(3). It refers to a "bump" most often on the anterior and also superior part of the femoral neck. In a camera lesion, the normally concave head/neck junction of the femur appears flattened or even convex(two) because the hip flexes, adducts and internally rotates this part of the femur then abuts against the acetabulum. Repetitive abutment applies shear stress into the articular cartilage resulting in delamination and labral tears can eventually occur(2). The cause of the anatomical variations on the femoral neck is unknown but a couple of theories have been suggested. Cam lesions could have a genetic inclination and/or they may occur due to over-activity of the epiphyseal plate (because of increased load) during adolescence(2,3). Most probably it is a combination of both of these factors. Ganz (2003) proposed that camera lesions can predispose the athlete to early osteoarthritis of the hip with up to 40 percent of OA hips revealing signs of a camera lesion(2).
2) Pincer impingement -- this refers to over- coverage of the acetabulum with a normal appearing femur. Acetabular abnormalities that may lead to pincer impingement contain a retroverted acetabulum, protrusion acetabula or osteophytic development. This type of impingement is commonly found in middle-aged guys.
3) Mixed presentation of both camera and pincer impingement -- this describes the situation where both cam and pincer impingement exist. It's important to under- stand that all these are anatomical variants and therefore are not in themselves the pathology but they might predispose the athlete to hip pathology both in the long and short term.
How Is FAI Diagnosed?
Subjective Assessment
FAI is most commonly seen in male athletes. They will frequently report a long history of hip stiffness or groin pain. They may report that their hip pain started with a minor trauma but never solved. They often report that their "hip flexors" happen to be tight particularly after prolonged sitting and that they might never sit back. Labral tears must be suspected when the athlete refers to a click or grating, giving way or locking feeling(1).Objective Assessment
FAI should be suspected in athletes that have limited hip ROM particularly into internal rotation in 90 degrees of hip flexion. This may be quantified in either supine or sitting. These athletes will probably also have a debilitating FADIR and restricted and debilitating FABER(4). Several evaluations are described as diagnostic for a labral lesion; those comprise: FADIR, FABER, impingement provocation test and Fitzgerald test. In Leibold's systematic review they discovered that the current best evidence that a negative finding for these tests gives the clinician good proof that there is not any labral tear present; however, no evaluation has adequate specificity to confidently predict when a labral tear is present(5).Imaging
Imaging is needed to validate the clinical investigation of FAI. Osseous abnormalities may be seen on x ray (but may be missed). If a bony impingement is suspected then a CT scan has improved precision nonetheless, you must be aware of the greater radiation dosage associated with CT scanning and a CT scan doesn't specifically diagnose labral or cartilage lesions.MRI may be utilized to recognize articular cartilage and labral pathologies; however, for imaging the labrum MR arthrography seems to create exceptional results(4).
Treatment
Conservative Therapy
At this stage there is no obvious evidence on when conservative or operative therapy are required. In circumstances where imaging shows minor signs of FAI and no additional significant pathology of the hip, conservative treatment should be trialled.1) Education
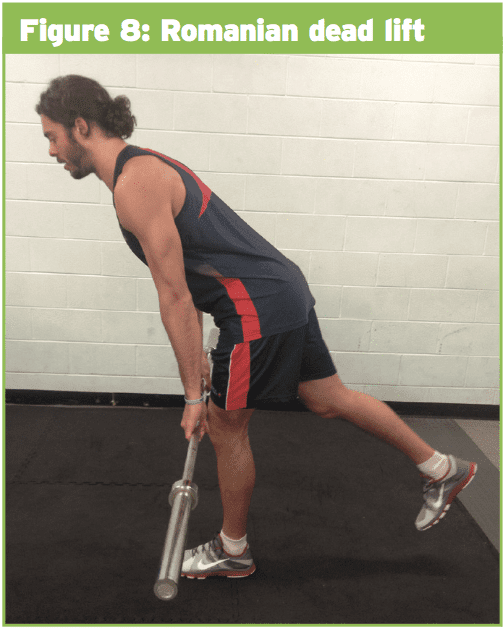
These athletes should avoid exercises and positions which impinge the hip (cool F angle >90deg) ie deep squats, leg press particularly in incline machine along with large step-ups. Some common positions which needs to be prevented are sitting at low seats where knees are higher than hips, sitting cross- legged and position using a hip hitched to a side. These athletes, even if they sleep in their side, must be encouraged to utilize a pillow between their knees and feet to help keep their fashionable from flexion and adduction.
2) Soft tissue work and manual treatment
Soft tissue work through TFL, ITB and adductors can be very beneficial to reduce tone in these muscles. This may be completed in a variety of various ways such as trigger point massage, work, roller and dry needling. Manual therapy methods to restore normal arthrokinematics of the fashionable are also quite useful in decreasing symptoms.
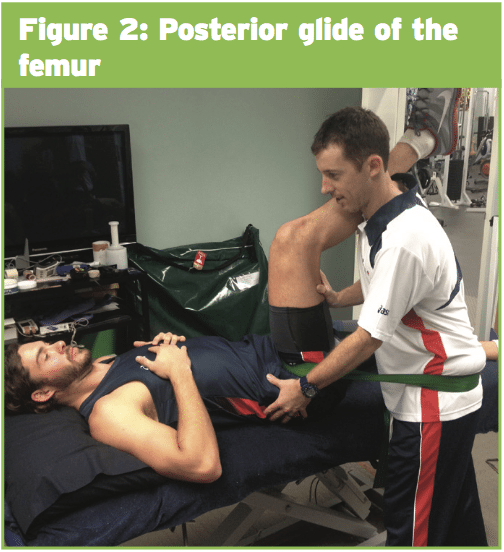
Normally as the hip flexes, the femur glides slightly posterior and conversely since the hip extends the femur should glide slightly anteriorly in the acetabulum.
Considering these arthrokinematics, manual therapy methods which posteriorly slide the femur are very useful in athletes that have inferior posterior glide of the femur during hip flexion (see Figure 2). Approaches that anterior slide the femur may be useful in athletes who lack hip extension. Lateral glides of the femur have also been demonstrated to be rather helpful to reduce symptoms and increase range in athletes with FAI.
What Are The Finest Rehabilitation Exercises To Do?
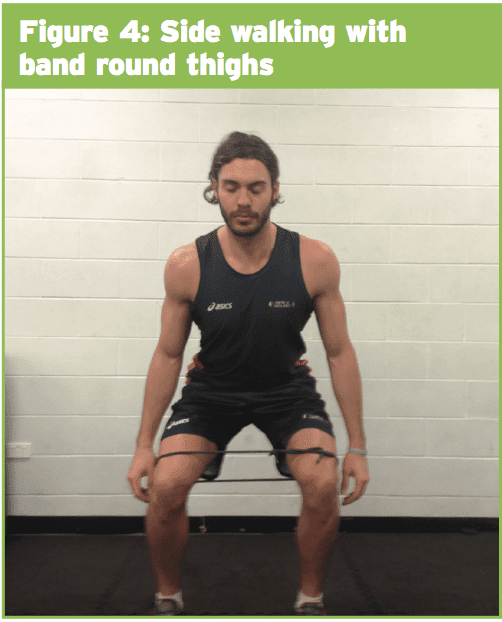
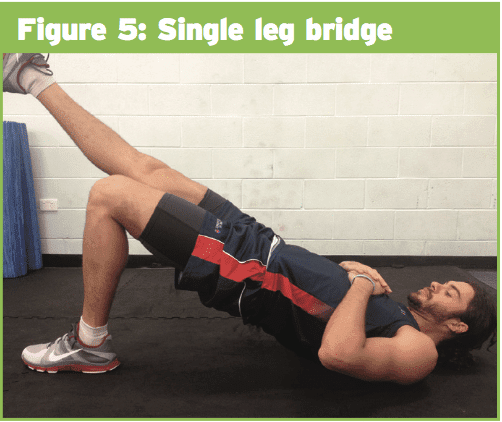
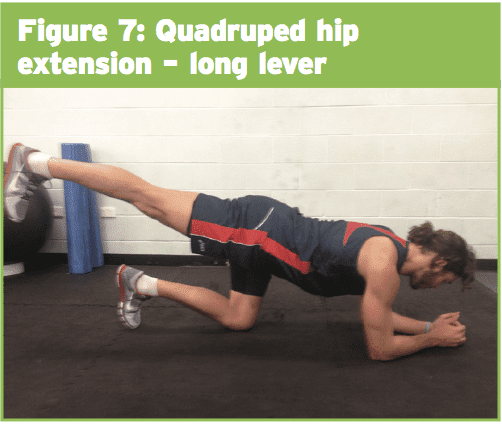
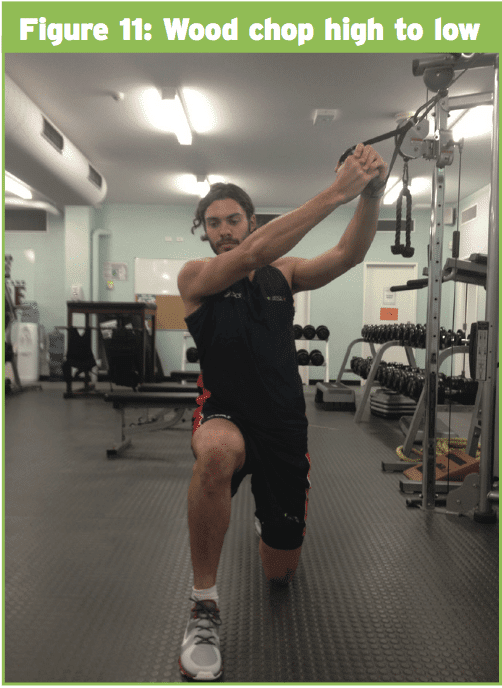
In most instances of hip pain, exercise therapy is vital to ensure long-term effects of therapy. Particular focus should be given to the hip abductor and hip extensor muscles.The hip abductor synergy includes of glut medius, exceptional glut max and TFL. Frequently in athletes, TFL is overactive and the gluteal part of the abductor synergy is weak. Recently, Selkowitz and colleagues, using EMG, set out to identify that which exercises especially target the gluteal muscles whilst reducing action of this TFL(7). The results of their study identified the five exercises that showed strong stimulation of gluteus medius and superior glut maximal using the least action of TFL (in healthy volunteers).
1) Clam -- activation of glut med and glut maximum was maximized while the pelvis was at a neutral position (vs a reclined position) and the hip was flexed to 60deg(6) (see Figure 3).
3) Single-leg bridge (see Figure 5).
4) Quadruped hip extension -- short and long lever (see Figures 6 and 7).
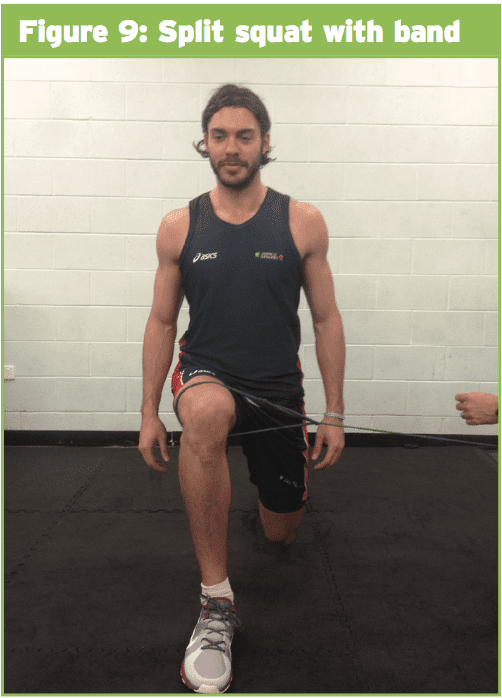
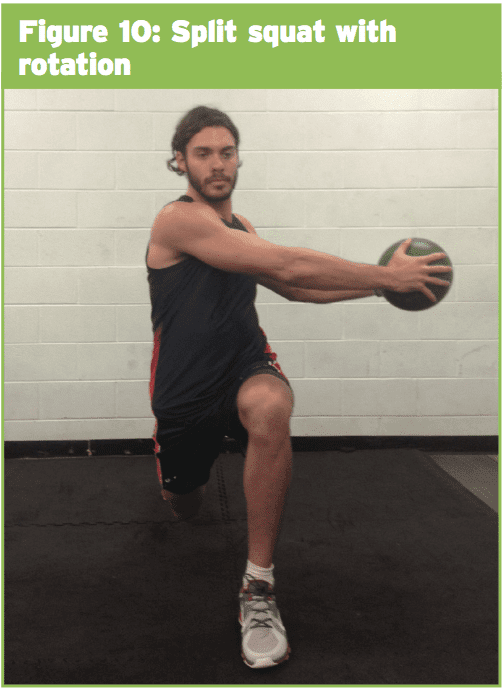
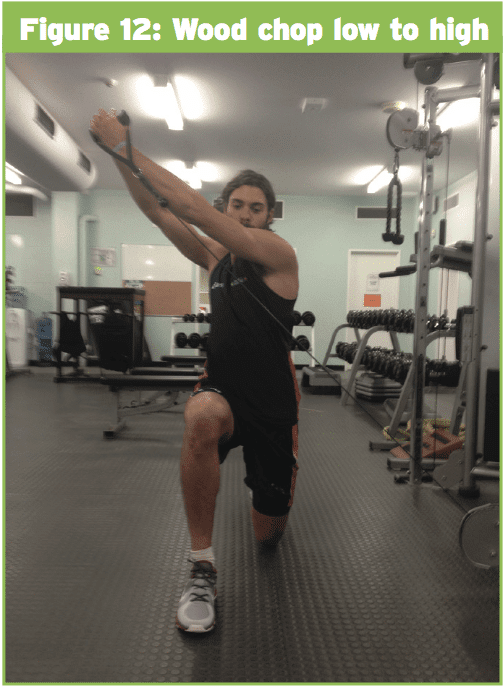
1) Split squat with band (see Figure 9);
Operative Treatment
If conservative therapy fails or if a significant bony lesion or labral tear is identified then surgery might be required. The objective of surgery is to not only repair/treat the labral lesion or chondral pathology but also relieve any rectal abutment. Historically this has been done through an open process but most surgeons now are doing these processes through arthroscopy. Chondral pathology might be seen and delaminated components will be trimmed/shaved and chondroplasty, drilling and micro fracturing may be used to help stimulate fibrocartilage regrowth. Labral tears related to FAI occur most commonly on the anterosuperior rim. Where possible these ought to be repaired instead of resected, as eliminating large parts of the labrum alter hip mechanics, which might lead to further damage. To restore the normal anatomy of the femoral head/neck junction if a cam lesion exists, a femoral osteoplasty/ chielectomy should be performed.Conclusion
Hip pain is a frequent reason for loss of training time in various different sports. This report has outlined the various types of FAI and possible conservative treatment options. Rehabilitation exercises are a critical part of the rehabilitation program of athletes with hip pain and a number of exercises that specifically target the gluteal muscles have also been described.References
1) Brukner and Khan (2012) Clinical Sports Medicine. 4th edition
2) Kasserjian A, Cerezal L, Llopis E (2006) Femoroacetabular Impingement. Topics of Magnetic Resonance Imaging Vol 17, No5 , 337-345
3) Ganz R, Parvici J, Beck M, Leunig M, Notzli H, Sienbenrock K (2003) Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clinical Orthopaedics and related research No 417, 112-120
4) Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Sobelle K (2009) What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthopaedica 80 (3) 314-318
5) Leibold R, Huijbregts P, Jensen R Concurrent criterion-related validity of physical examination tests for hip labral lesions: a systematic review. The Journal of manual and manipulative therapy vol 16 no 2 e24-e41
6) Wilcox E, Burden A (2013) the influence of varying hip angle and pelvis position on muscle recruitment patterns of the hip abductor muscles during clam the exercise. Journal of Orthopaedic and Sports Physical therapy Vol 43, No 5 325-332
7) Selkowitz D, Beneck G, Powers C (2013) Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lata? Electromyographic assessment using fine wire electrodes Vol 43, No 2 54-66