Science based chiropractor, Dr. Alexander Jimenez takes a look at the patho-anatomy of a side strain and outlines clinical tests to assess, treat and determine readiness for return to play for a cricket fast bowler.
Side strains are reported in a number of sports, such as javelin throwers, baseball pitchers, tennis players, golfers and cricketers. This article however will focus on side strains in cricketers. Australian cricket information (according to both national and state gamers) reports that in the 18 cricket seasons up to 2013-2014, side breeds had the second greatest incidence and the third greatest incidence of accidents that led to players lost games(1). More than 90% of the reported unwanted strains (called acute onset lateral back pain and also happen throughout the bowling delivery) at cricketers over the past twenty years have happened in fast bowlers(1).
What Is A Side Strain?
A side strain in cricket happens most commonly when bowling. Fast bowlers will describe that through a single delivery, they believed abrupt onset, sharp lateral trunk pain on the side contralateral to their bowling arm(two). On most occasions the bowler is not able to continue bowling (while this isn't always the case) and also often the player will leave the area. The mechanism of injury is thought to be related to the bowler; their quest to increase ball speed, vigorously pulling the front arm (contralateral side to their bowling arm) down causing a strain (see figure 1).Clinical Presentation
The quick bowler will commonly report an acute localized sharp lateral back pain (frequently at the mid axillary line) which occurred during their delivery. They might also clarify pain with breathing, coughing and coughing, and they are sometimes quite uncomfortable moving around particularly rolling over in bed. The pain may radiate slightly into the abdominal area. From this description alone a side strain is highly likely. Some useful clinical evaluations that help to confirm the identification (and track its development) are as follows:- Palpation -- A player with a side strain will be extremely tender over one or more of the lower four ribs (most commonly at the mid axillary line).
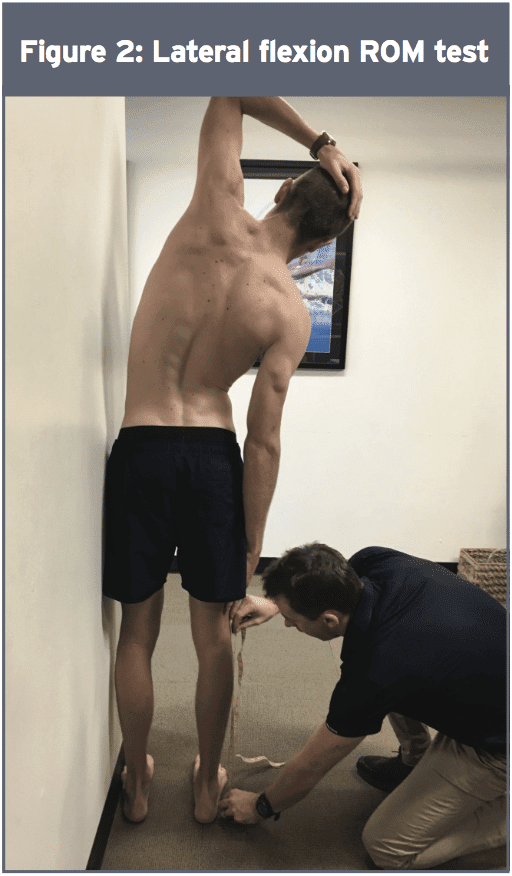
- Lateral flexion assortment of motion (ROM) evaluation ROM (see Figure 2) -- The participant stands side on to a wall with feet pelvis width apart, and the pelvis and the lateral border of one foot up against a wall. The hand closest to wall is placed on their mind. Together with the pelvis remaining connected with the wall, the player is then requested to only laterally flex away (avoiding truck flexion or extension) from the wall so far as they can and the therapist steps how far in the ground their middle finger may reach their leg down. This evaluation in the early stage is often both restricted and painful. The therapist steps both the distance and where the restriction is felt -- such as 'jamming' on ipsilateral side or 'stretch' on contralateral side. These results can then be compared with all the non-injured side and/or previous measures. This evaluation is also used as a monitoring tool during a year to determine 'normal selection and feeling' and may pick early indications of tightness. Post injury, players need to have the ability to return to complete lateral flexion assortment of motion and their normal limitation feeling.
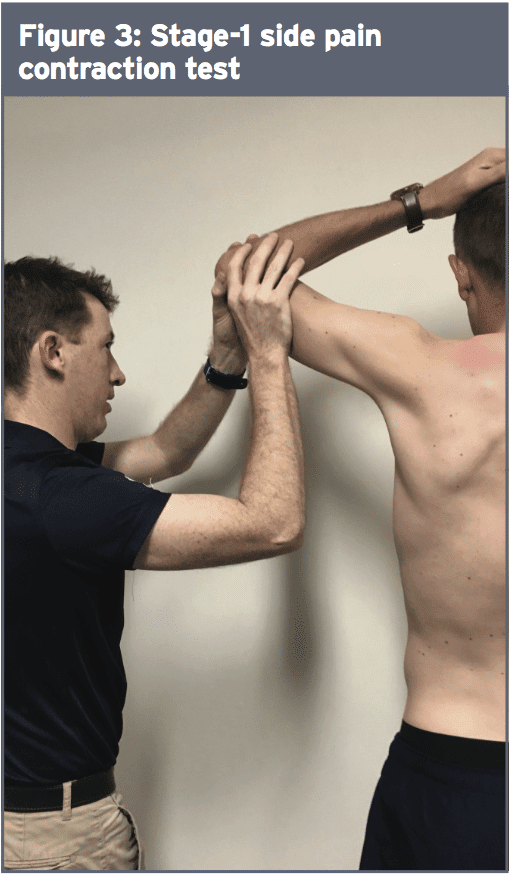
Side Pain Contraction Tests
(Note -- these evaluations are progressive with stage 1 being the easiest and stage 3 the toughest. Once a player is pain-free on a single point, the testing could be improved to the next phase.)- Stage 1: Isometric shoulder adducted in 90-degree abduction – Player places hand of side that is injured on head, with elbow remaining in line with body in coronal plane. The therapist places hands just proximal to elbow and the player attempts to adduct shoulder. The therapist pushes up as the player pushes down to ensure an isometric test (see figure 3).
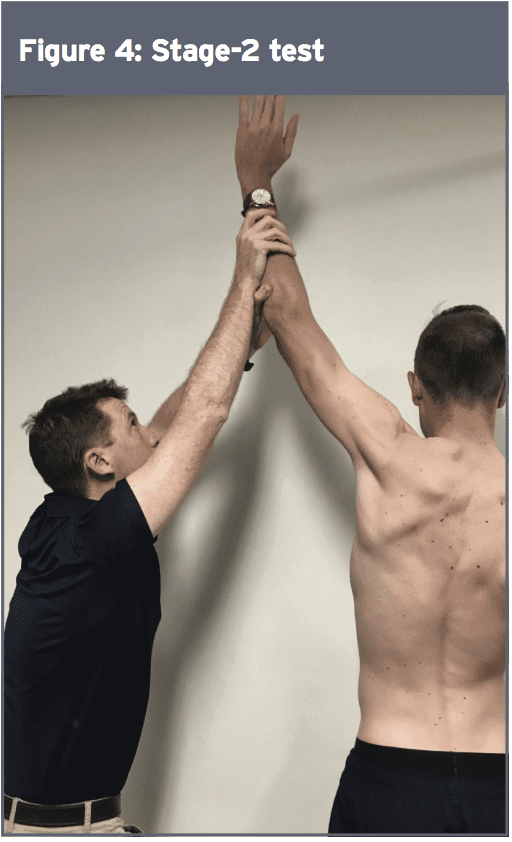
- Stage 2: Isometric shoulder adduction from elevation – Player fully elevates the hand of side that is injured. The therapist places hands just proximal to elbow or wrist, and the player attempts to adduct shoulder. The therapist pushes up as the player pushes down to ensure an isometric test (see figure 4).
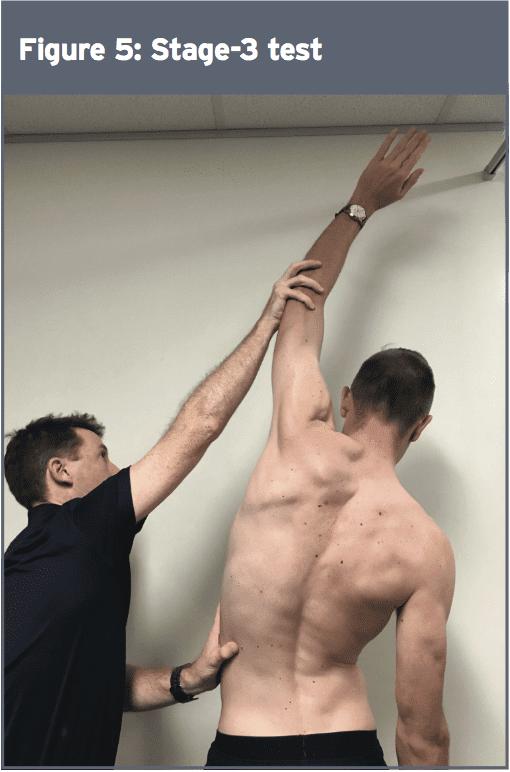
- Stage 3: Isometric shoulder adduction and ipsilateral side flexion from full shoulder elevation and contralateral side flexion – Player fully elevates hand of side that is injured and then laterally flexes truck to the contralateral side. The therapist places hands just proximal to wrist (or elbow) and the player attempts to adduct shoulder and lateral flex trunk towards the injured side. The therapist pushes up as the player pushes down to ensure an isometric test (see figure 5).
Alternative Contraction Tests
- Sit up/crunch with resistance – Player lies in crook lie with hands across chest. They then do a straight crunch. To further load the oblique muscles, a rotation can be added to the crunch. If these are not painful then the therapist may add resistance to increase the demand of the test (see figure 6).
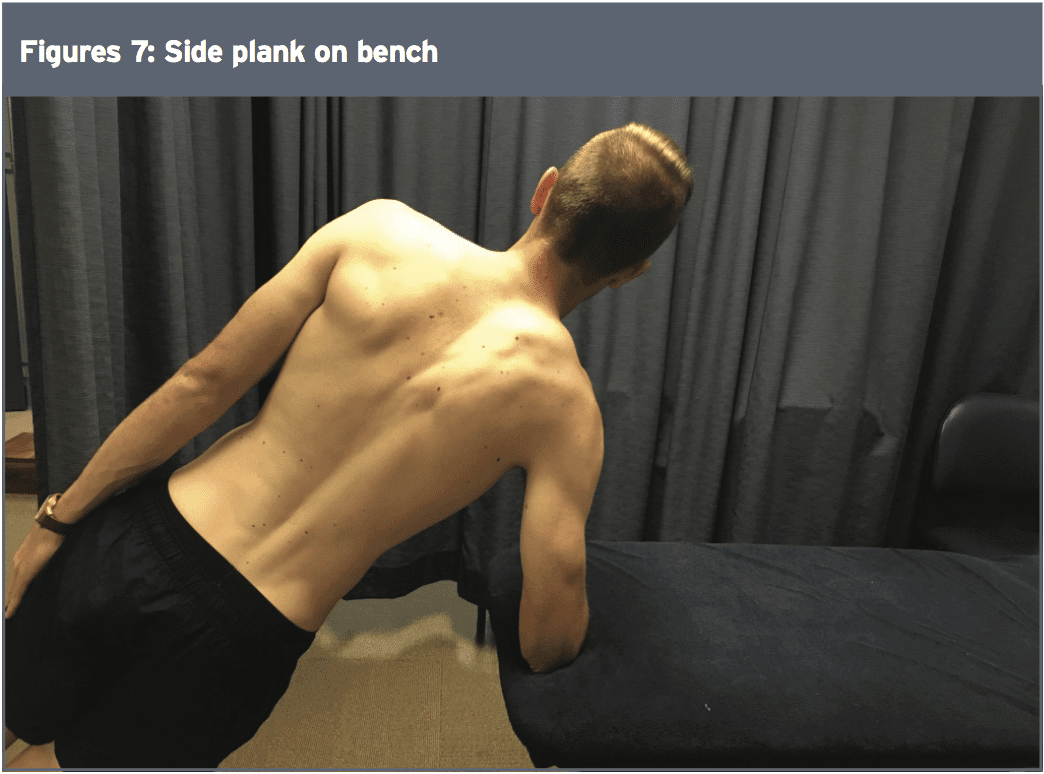
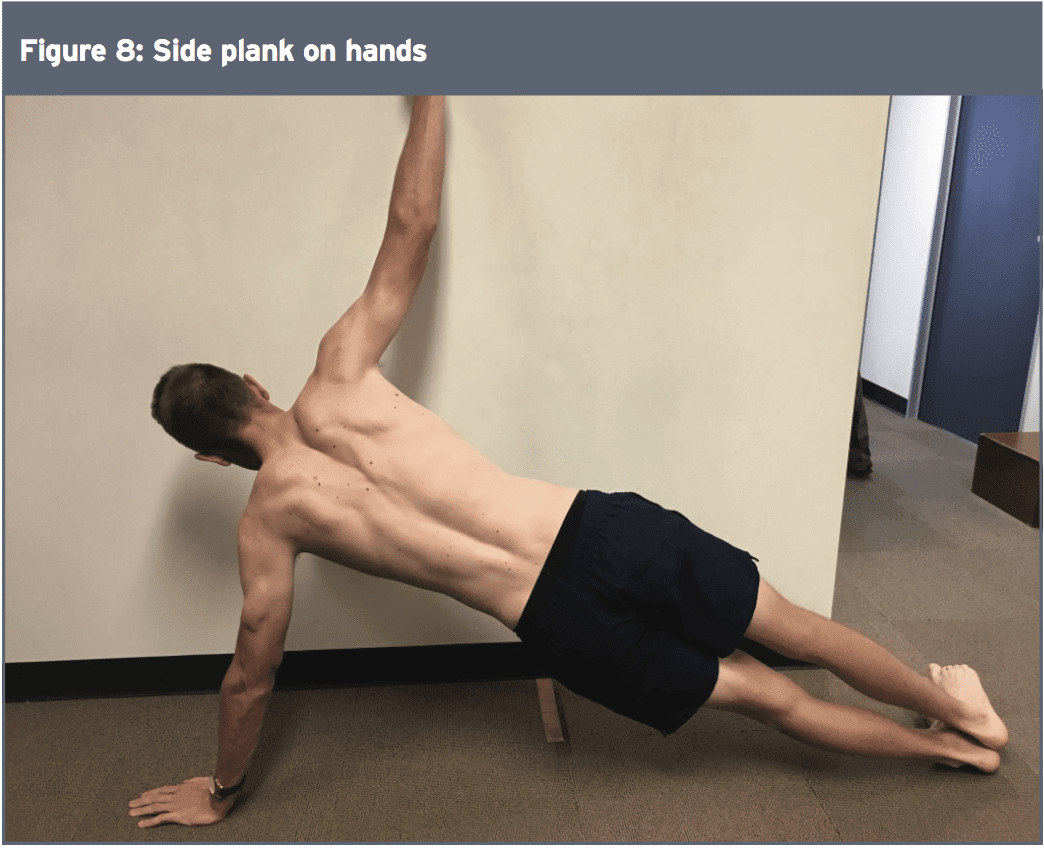
- Side plank – This test can be very painful initially. The side plank is not only a good assessment test, but it can also be used to monitor and progress treatment. Initially a side plank may only be able be possible on knees or with elbows on bench (height of bench and time should be recorded – see figure 7). As a player progresses the difficulty of the test can be increased by increasing time of hold or decreasing height of bench until they are on the floor. Alternatively, the difficulty can be increased by asking the player to do it on their hands rather than their elbow (see figure 8).
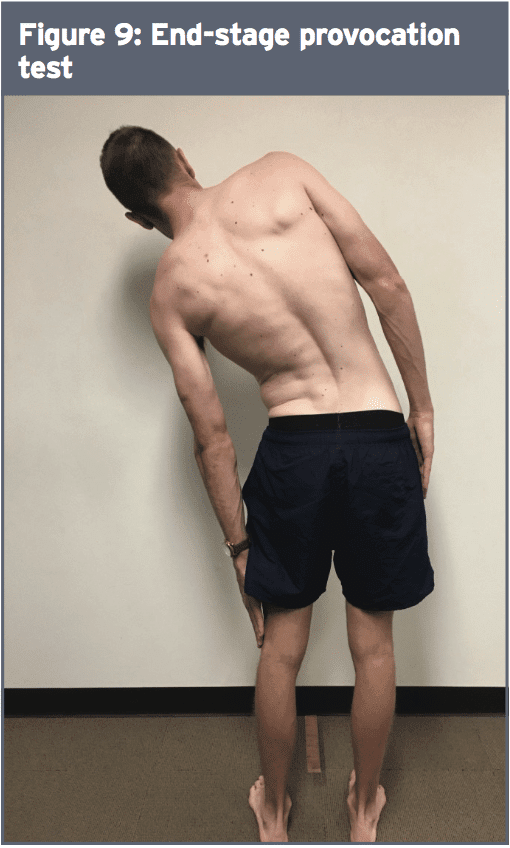
Once a player has no pain on breathing or cough and has full pain-free range of motion then these two movements can be combined. Player fully lateral flexes to side of pain and takes as deep a breath as possible. Any pain is noted (see figure 9). If this is pain free then a cough can be added in full side flexion. If this test is pain free, the player can then progress to some bowling at moderate intensity.
Imaging
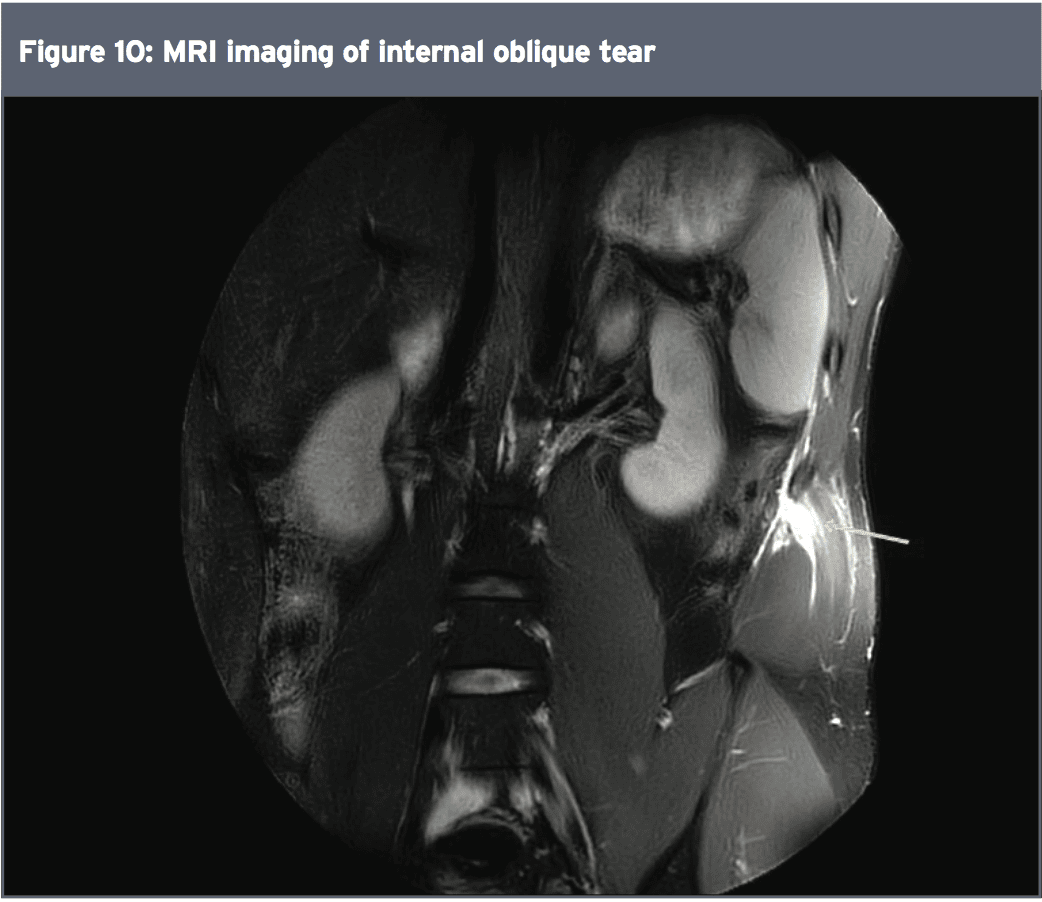
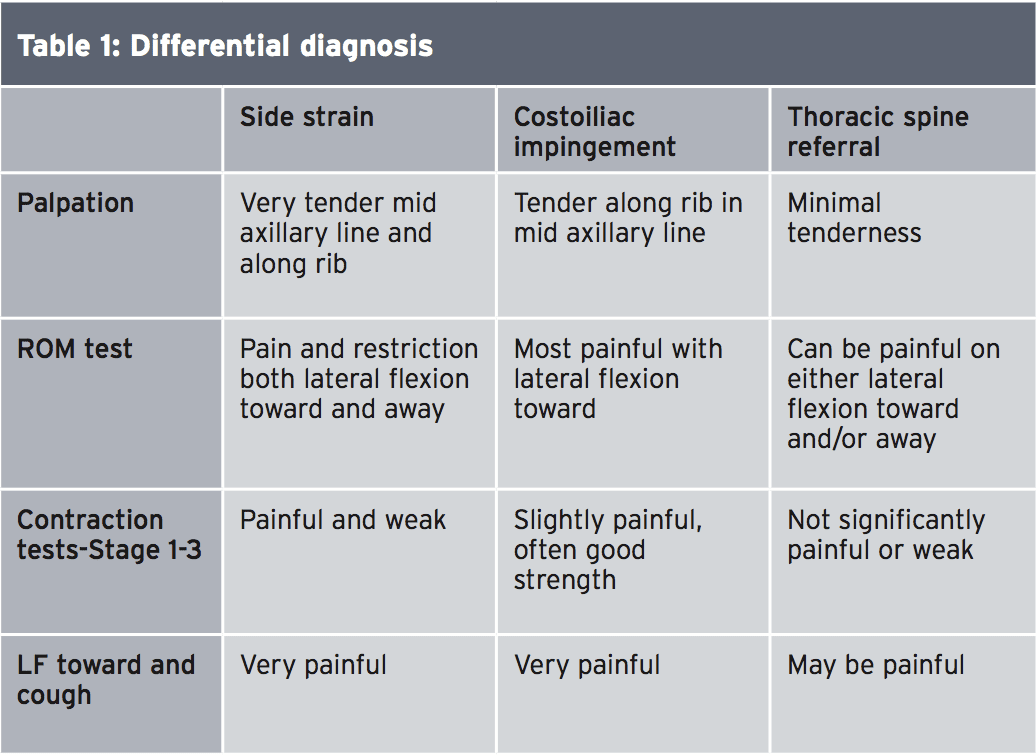
Identification of a side strain is generally a clinical diagnosis based on the explanation of positive and injury findings summarized previously. Imaging is however beneficial in deciding the degree of damage and precise structures involved(two). Ultrasound may be used however, MRI is the modality of choice. On MRI, an acute side strain is characterized by high signal on T2 image at the muscular, rib/costal cartilage port, and frequently shows partial or complete rest of the abdominal musculature(two). The internal oblique at its attachment on the 11th rib is the most frequent muscle hurt. But, pathology has also been reported in external oblique, transversus abdominus and abdominal muscular attachments of their 9-12th ribs(1,2). MRI imaging may also show rib or costal cartilage damage, including bone strain, bone avulsion or periosteal stripping(1). With these harms, hematoma may be viewed tracking between the internal and external oblique musculature(1). Figure 10 shows a MRI image of an elite level fast bowler with a tear of the inner muscle as it attaches onto the 11th rib.Differential Diagnosis
Other possible diagnoses that should be considered when analyzing a bowler with side pain are:- Costoiliac impingement. This happens as a consequence of a drop in space between the lower ribs and pelvis, and might be due to either a hypertrophied internal/external oblique muscle, rib hypertrophy or a hypersensitive scar from a former side strain.
- Referral from thoracic spine and/or either costotransverse or costovertebral joints.
Treatment
At the first stages, the principal intention is to decrease pain especially if coughing, breathing and sneezing are debilitating. This can be done via the usage of pain-relieving medication in the acute phase. After the player can deep breathe and cough afterward cardiovascular training can commence -- initially with bike or walking and then progressing to running as pain allows.Once tenderness starts to resolve, hands on treatment can also be useful. This includes:
- Soft tissue work throughout abdominal musculature including obliques, and rectus abdominus.
- Thoracic spine and rib mobilisation.
- Gentle stretching to contralateral side, together with deep-breathing drills to help expand ribs.
- Dry needling.
1) Isometric: side planks – start on bench and progress to floor (as per the assessment test)
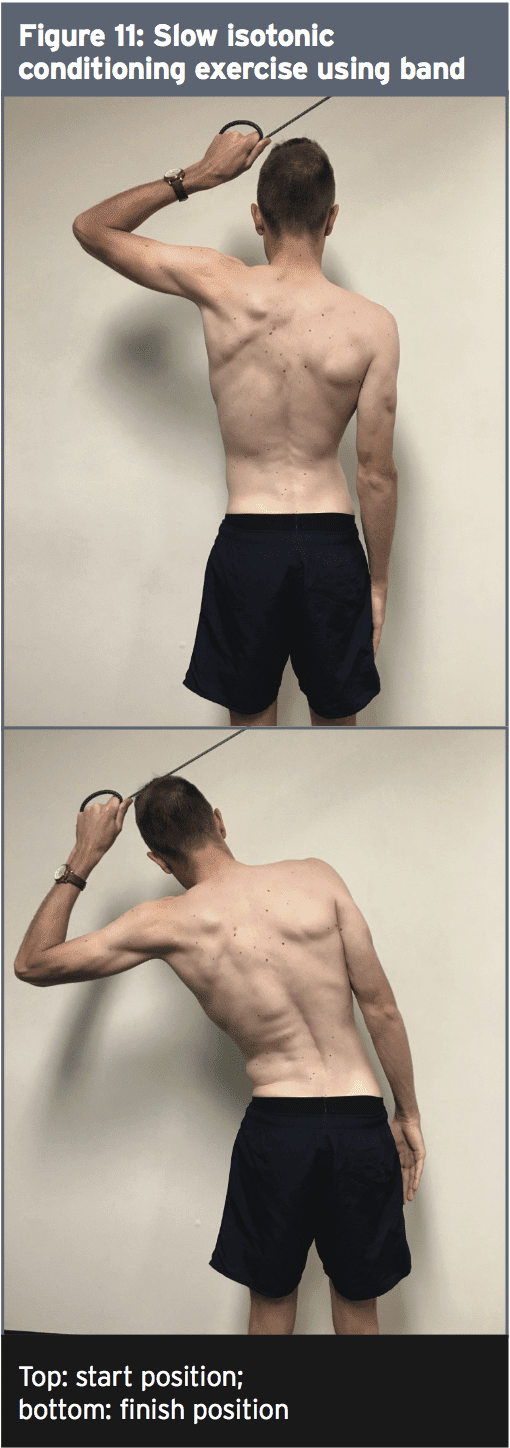
2) Slow isotonic: through range with band or pulley machine – see figure 11.
2) Slow isotonic: through range with band or pulley machine – see figure 11.
1) no pain on breathing, coughing or sneezing
2) full ROM and no pain with ipsilateral lateral flexion
3) no pain and good strength with stage 1-3 contraction tests
2) full ROM and no pain with ipsilateral lateral flexion
3) no pain and good strength with stage 1-3 contraction tests
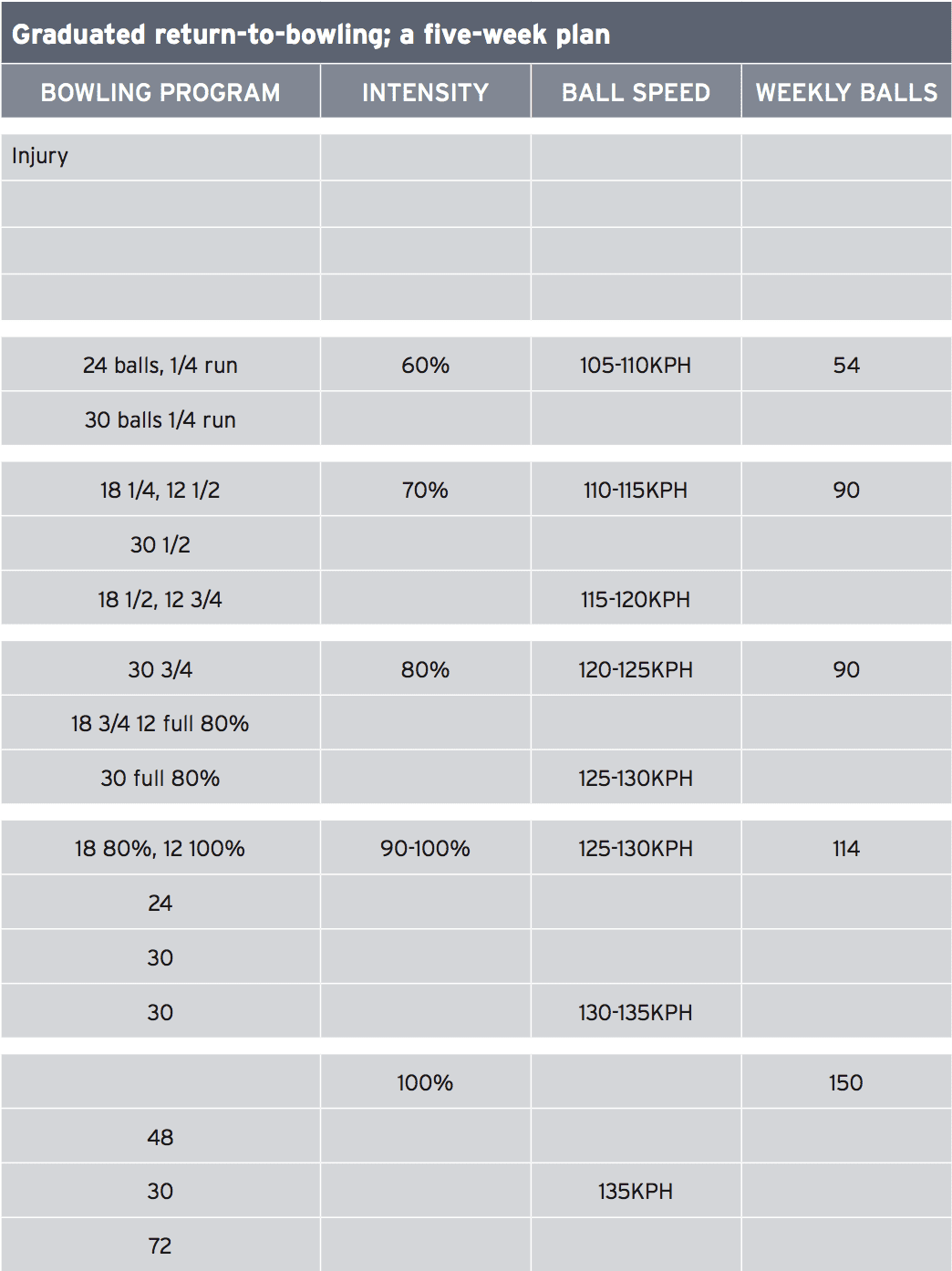
The duration of time to return to play with this harm varies substantially with reports ranging from one to seventy times(1). Rehabilitation should be directed by a player's symptoms rather than based on scanning results or a predetermined time. In season recurrence rates are high with this injury, and as such, the return to bowling plan requires to a graded return to both intensity and volume.
Table 2 shows an example of graduated return to bowling plan for a player who returned to play at week six. Anecdotally, harms that involve the rib/costal cartilage tend to take longer than those that simply involve muscle. However, further study is needed comparing scan time and results to come back to play until this is confirmed.
Conclusion
Negative breeds are a common and significant injury to cricket fast bowlers as they often require considerable periods of rehabilitation and inability to perform. The clinician should be aware that this harm has a high 'within-season' recurrence rate and a graded return to high-intensity bowling is integral part of the rehab process. Further studies have to determine risk factors and also the relationship between imaging findings and time frames for returning to play.References
1. J Sci Med Sport. 2017 Mar;20(3):261-266
2. British Sports Med 2004 38 (5): e21