Science chiropractor, Dr. Alexander Jimenez explores ankle movement -- and discusses why it is so Important
Introduction
Given that we're a bipedal bunch, the joint that connects the foot into the rest of our body is going to have a considerable influence on our movement.Most men and women get pretty good at compensating for any motion deficiencies they might have. It seems, however, that one of the most troublesome moves to compensate for, without hurting oneself, is a lack of ankle dorsiflexion (DF) range of motion (RoM).
There is some evidence to suggest that a deficiency of DF will cause compensatory moves elsewhere. Understandably the research showing that these movement patterns lead directly to injury are few and far between, but there are a few.
So the logic seems sound, the evidence in 'normals' is suggestive and you'll find a small number of research pertaining directly to injury. On the other hand, the literature to demonstrate that enhancing deficiencies will really reduce following injury is nonexistent. I feel this should not stop us from pursuing our own logic, and therefore in many circumstances this will mean trying to 'normalize' an athlete's DF.
Identifying Hypomobility
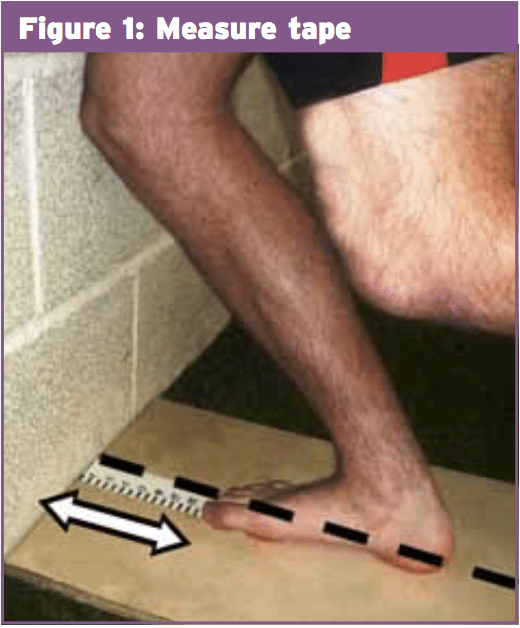
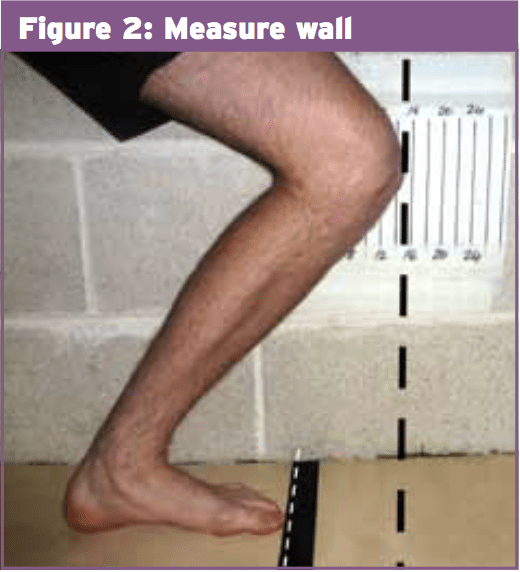
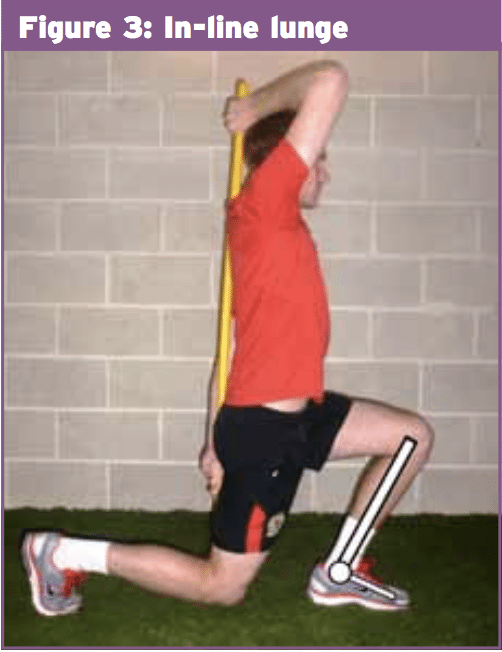
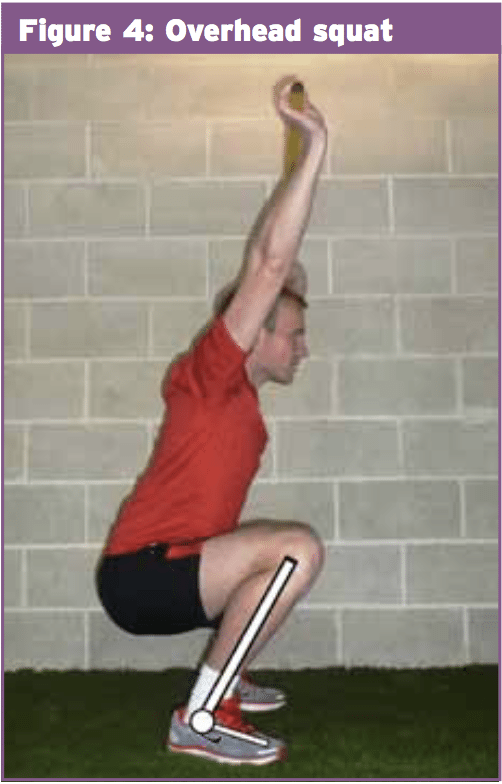
Measurement of DF is straightforward enough (Figures 1 and 2), also supplying subjects keep their heels on the floor and foot nicely aligned I'd suggest it's also fairly reliable; one screening study working with sports folks agrees(1), and so does a study on validity and reliability from 2012(2). The test in Figure 1 is far more prone to cheating by athletes, as it is too tempting to push 'just that little bit farther'; nonetheless, the test from Figure 2 is somewhat slower. I find a camera may be helpful here; it is good for illustrating issues to athletes, and can be more compelling than a numerical measurement on a page when you return. This is very helpful when an athlete has a subsequent trauma, as you can both see where their older 'normal' was; if that is different to 'normal' in their other hand, this will provide you a much more valid dimension to use. In a clinical sports setting, we seldom let athletes operate until they are within 2cm of normal, so if they had a pre-injury side-to-side difference in RoM this can be quite relevant. Lining up the camera lens with the front of the knee is imperative to be able to prevent parallax error.There are certainly more functional DF tests with good reliability on the market (once testers are satisfactorily trained(5)), if that's a degree of screening you'd like to extend to. However, a very simple dimension of DF (like Figures 1 and 2) may add additional detail to the big picture if these functional tests (Figures 3 and 4) highlight deficiencies.
The Rationale
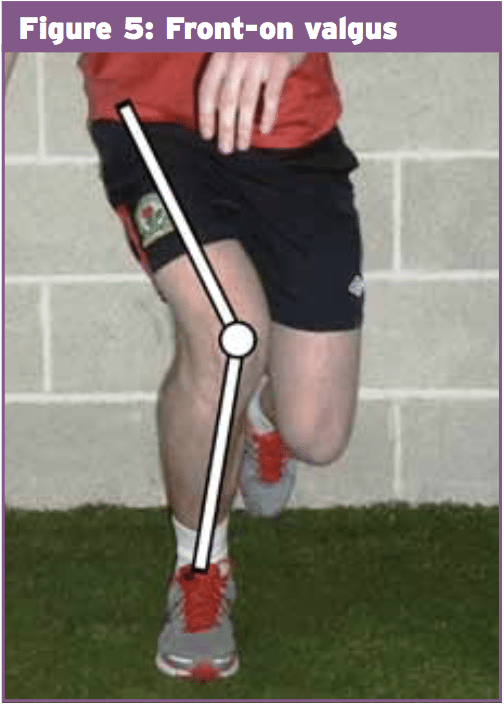
The rationale here is straightforward enough; athletes utilize triple flexion (in the hip, shoulder and knee) to attenuate the forces of landing, during running, jumping and cutting. When there is inadequate DF RoM from the ankle to get this done, another joint may then need to compensate, and musculotendinous structures will be functioning in a less than optimum position.To be able to attenuate more pressure, the knee will tend to use either more flexion, more valgus/frontal airplane knee excursion (FKPE)(Figure 5) or both. (see SIB posts 102 and 110 to learn much more on FKPE and its own role in harm). Any structure above or below the ankle could of course end up bearing the additional weight here; consider (or see SIB 113) the spinal column (Figure 6), or the feet(6).
- Poorer movement patterns are associated with reduced DF RoM during a lateral step down task in healthy subjects(7);
- Normal subjects with artificially limited DF on a double squat show increased FPKE(8);
- In a study of soccer players, those with less DF RoM exhibited higher FPKE during a drop landing task(9) ;
- A 2013 study showed that subjects with lower DF RoM altered their kinematics during vertical jump by lifting their heels and changing their trunk position(10).
There are a variety of interesting studies showing restricted DF RoM to be associated with, or a risk factor for, injury. For example, away from the knee specifically, this is seen for lower limb injuries in Aussie rules players and Naval Trainers, and standard injury risk in cricketers(12,13,3). Soldiers with reduced DF RoM also had 4.6:1 odds of developing a metatarsal stress fracture compared to those without(6).
Decreased DF was also implicated in the development of patellofemoral pain syndrome (PFP) at runners(15); this could possibly be clarified by the current study previously(8) in which increased knee valgus/FPKE and decreased quadriceps activation were seen when DF was restricted, very similar to the typical demonstration of PFP.
Correction
I have encounter no noteworthy evidence either way for whether 'normalizing' that this dorsiflexion will lead to an actual reduced injury risk in our athletes. One 2013 study, however, did reveal that in chronic foot injuries, mobilization of DF facilitated improved joint angles during landing, resulting in a more positive foot position(16). So, with avoidance in mind, we will need to look at what we do understand and apply some logic.It appears sensible that where any shortage is marked and unilateral (maybe the end result of an old/recent injury) there should be good profits to be made. Anecdotally, not just if changes come more easily, but asymmetries generally have a greater impact on motion patterns and injury risks. Where shortages are bilateral and more standing in character I feel that the profits will be harder to come by and less inclined to be effective, in order a preventative/screening problem it may be bad value for money.
The listing of structures that could be impacted by these compensations is infinite. I would include in this group any athlete having an greater strain or strain in any areas round the ankle. Any athlete with a famous DF deficit ought to be persuaded to have this sorted out to the good of not just their ankle but a lot besides.
Consequently, should you wish to enhance an athlete's DF, what resources do we have available to us? First let us talk my favorite techniques.
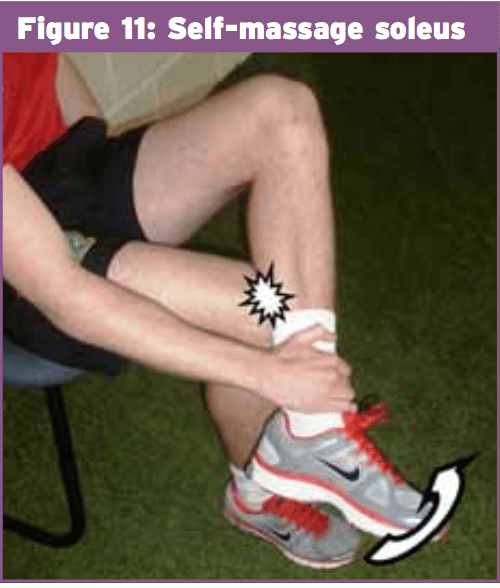
Patient-Generated Techniques
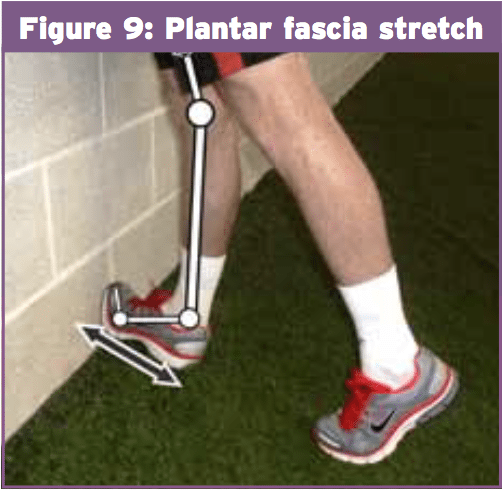
Plantar Fascia Stretch
Extending the knee and feet should have the effect of tightening up the fascial structures (shallow back lineup) and helping place a bias on the plantar fascia.Therapist-Generated Techniques
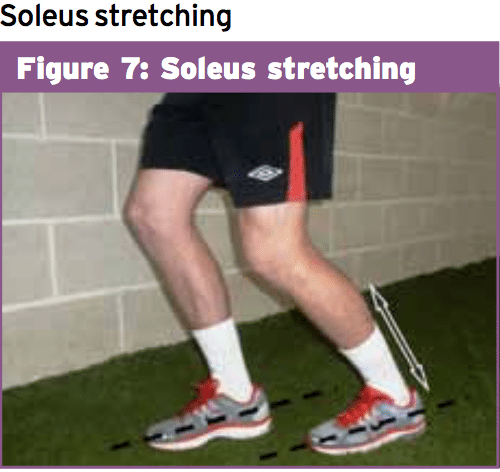
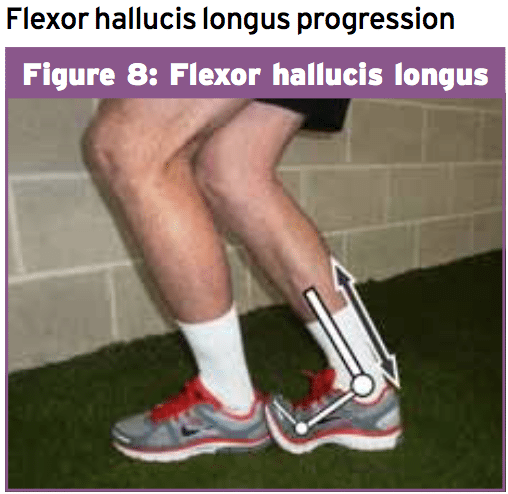
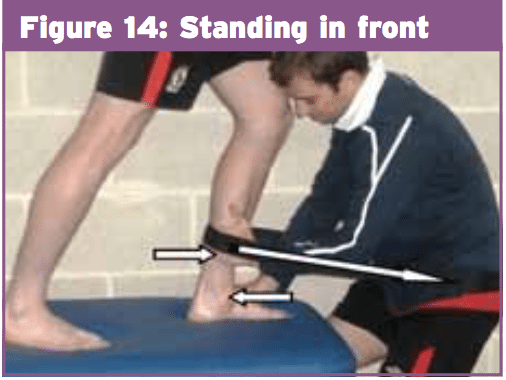
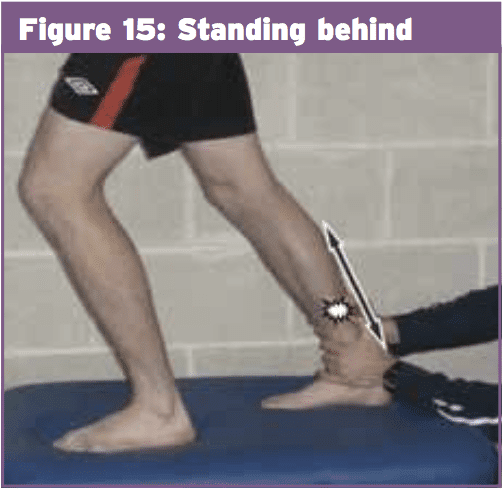
My favorite techniques are the ones which allow you to access a number of constructions in the 1 position and to add active motion whenever possible.Step Lunging
This position is much more of a progression. Not only does this add weight-bearing to the mix, but it also allows for a few more practical and lively motion to be added.Conclusion
For my money, these simple methods of identification and therapy are well worth the attempt. The tests only take a moment and once a deficit is identified the treatments are only a logical development. The remedies also have the benefit of between the athlete and keeping them active, which makes this a team effort rather than being overly passive. They also lead us nicely into a 'test, re-test' scenario so both you and the athlete could determine which techniques work to them and how they then change their more functional tests.References
1. Dennis RJ, Finch CF, Elliott BC, Farhart PJ. The reliability of musculoskeletal screening tests used in cricket. Phys Ther Sport. 2008 Feb;9(1):25-33. Epub 2007 Nov 8.
2. Chisholm MD, Birmingham TB, Brown J, Macdermid J, Chesworth BM. Reliability and validity of a weight-bearing measure of ankle dorsiflexion range of motion. Physiother Can. 2012 Fall;64(4):347-55.
3. Dennis RJ, Finch CF, McIntosh AS, Elliott BC. Use of field-based tests to identify risk factors for injury to fast bowlers in cricket. Br J Sports Med. 2008 Jun;42(6):477-82. Epub 2008 Apr 7.
4. Backman LJ, Danielson P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in juniorelite basketball players: a 1-year prospective study. Am J Sports Med. 2011 Dec;39(12):2626-33. 2011 Sep 14.
5. Minick KI, Kiesel KB, Burton L, Taylor A, Plisky P, Butler RJ. Interrater reliability of the functional movement screen. J Strength Cond Res. 2010 Feb;24(2):479-86.
6. Hughes LY. Biomechanical analysis of the foot and ankle for predisposition to developing stress fractures. J Orthop Sports Phys Ther. 1985;7(3):96-101.
7. Rabin A, Kozol Z. Measures of range of motion and strength among healthy women with differing quality of lower extremity movement during the lateral step-down test. J Orthop Sports Phys Ther. 2010 Dec;40(12):792-800. Epub 2010 Oct 22.
8. Macrum E, Bell DR, Boling M, Lewek M, Padua D. Limiting Ankle Dorsiflexion Range of Motion Alters Lower Extremity Kinematics and Muscle Activation Patterns during a Squat. J Sport Rehabil. 2011 Nov 15. (Epub ahead of print).
9. Sigward SM, Ota S, Powers CM. Predictors of frontal plane knee excursion during a drop land in young female soccer players. J Orthop Sports Phys Ther. 2008 Nov;38(11):661-667.
10. Papaiakovou G.Kinematic and kinetic differences in the execution of vertical jumps between people with good and poor ankle joint dorsiflexion. J Sports Sci. 2013;31(16):1789-96.
11. Basnett CR, Hanish MJ, Wheeler TJ, Miriovsky DJ, Danielson EL, Barr JB, Grindstaff TL. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int J Sports Phys Ther. 2013 Apr;8(2):121-8.
12. Gabbe BJ, Finch CF, Wajswelner H, Bennell KL. Predictors of lower extremity injuries at the community level of Australian football. Clin J Sport Med. 2004 Mar;14(2):56-63.
13. Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999 Sep-Oct; 27(5):585-93.
14. Malliaras P, Cook JL, Kent P.Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players. J Sci Med Sport. 2006 Aug;9(4):304-9. Epub 2006 May 2.
15. Lun V, Meeuwisse WH, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. Br J Sports Med. 2004 Oct;38(5):576-80.
16. Delahunt E, Cusack K, Wilson L, Doherty C. Joint mobilization acutely improves landing kinematics in chronic ankle instability. Med Sci Sports Exerc. 2013 Mar;45(3):514-9.
17. Loudon JK, Reiman MP, Sylvain J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review. Br J Sports Med. 2014 Mar;48(5):365-70. doi: 10.1136/bjsports-2013-092763. Epub 2013 Aug 26.
18. Landrum EL, Kelln CB, Parente WR, Ingersoll CD, Hertel J. Immediate effects of anterior-toposterior talocrural joint mobilization after prolonged ankle immobilization: a preliminary study. J Man Manip Ther. 2008;16(2):100-5.
19. Fujii M, Suzuki D, Uchiyama E, Muraki T, Teramoto A, Aoki M, Miyamoto S.J Man Manip Ther. 2008;16(2):100-5. Does distal tibiofibular joint mobilization decrease limitation of ankle dorsiflexion? Man Ther. 2010 Feb;15(1):117-21.
Epub 2009 Oct 17.
20. Mulligan, BR. 1. Manual Therapy: NAGs, SNAGs, MWMs, etc. 6th Edition. New Zealand: Plane View Services Ltd.; 2010