Science based chiropractor, Dr. Alexander Jimenez has a look at the legends and the realities of this very common injury.
Introduction
This paper targets one of the most famous body part injuries -- the Achilles tendon (AT). Injuries to the AT possess a somewhat mythical foundation. It is highly likely that the legendary Greek warrior Achilles ruptured his AT when shot by the bow fired by Paris, King of Troy.A sudden heel drop at a bud hole whilst conducting, a quick take-off in tennis or a sudden hop are mechanics that usually cause tendon rupture. Due to the exceptional strength of the AT, it's been suggested that rupture of the tendon is almost impossible without prior degeneration from the tendon, and that, coupled with a high mechanical force that's essential to rupture the tendon, may account for the greater incidence in the 30-40-year-old age category.
Only recently has surgery on the AT become the preferred choice of treatment. It was just following the First World War that surgery was attempted on a ruptured tendon; prior to this, distinct kinds of immobilization was utilized to attain a favorable result in a ruptured AT. In contemporary sports medicine, a lot more is known concerning the histological and biomechanical influences in AT rupture and much more is also known on the outcomes of surgical versus non-surgical repairs of this tendon.
This paper will present an in-depth explanation on the human anatomy and biomechanics of the AT, how an AT could be deciphered, what are the presenting symptoms and signs and the way the injury is best handled and rehabilitated.
Anatomy
The AT is the biggest tendon in the human body. It's formed from the conjoined tendons of the gastrocnemius and soleus muscles. The gastrocnemius extends downwards towards the heels and combines together with all the AT about 11-26 cm over the heel bone. The soleus extends further down to combine using the AT about 3-11 cm over the heel bone. Furthermore, the tendon of the vestigial plantaris muscle also blends with the AT on the medial side of the tendon.Since the tendon runs down to the heel bone it rotates 90° so that the gastrocnemius muscle fibers turn into operate anterolaterally and the soleus fibers turn to run posteromedially. The AT continues to the heel bone and inserts onto the calcaneus. It spreads because it approaches the heel bone so that it's wider at its insertion than at its own mid-portion. A little bursa sits posterior to the AT insertion and it protects it from any rubbing against an external surface (such as a shoe).
The mid-portion of the tendon is the most interesting since it's postulated that it is here that a relative avascular zone exists that may result in a rupture zone. As the thoracic receives a blood supply from the north side through the muscle and also on the south side via the heel bone insertion, the mid-zone between the 2 areas signifies a 'water drop' zone that has poor arterial nutrition. The arterial supply in this mid-zone comes from the fatty tissue that surrounds the tendon. With high mechanical pressure in the shape of tensile and compressive pressure, the tendon fibers can break down and degenerate. Due to this comparative avascular nature of the tendon inside this zone, the thoracic may enter a state of disrepair and become diminished and thus act much like a frayed rope which eventually snaps.
At length, the tendon is coated by a thin paratenon and epitenon and doesn't have a true synovial sheath. These structures include fatty tissue, thin membranes, blood vessels and connective tissues. These anatomical structures are also subject to harm and may be a source of pain in the AT.
Biomechanics Of The Achilles Tendon
It has been suggested that if it had been possible to dissect a healthy AT and bolt it to the ceiling, it would be possible to hang on a one-tonne weight before it would fail and rupture.Under load it will stretch and presume that a linear orientation. This happens at as little as 2% elongation, is subject to elevated load at 4 percent elongation along with the tendon will neglect macroscopically at 8% elongation.
The cross-sectional area of the tendon is correlated to the magnitude of the calf muscle complex and also height and age of the individual; that's is, the larger the calf and/or the individual, then the larger the tendon. The tendon (such as all tendons) is subject to loading and certainly will change and alter its internal architecture depending on the loads imposed upon it. It'll undergo hypertrophy in exercise-induced wealthy situations.
Histologically, the tendon is constituted of extracellular proteins such as elastin, proteoglycans and other molecules as well as fibroblasts (collagen manufacturers). The turnover time for this type 1 collagen is slow, and it takes about 50-100 weeks to the tendon fibers to flip over. Hence a balance exists between breakdown and synthesis in the veins that are healthy. It speeds up synthesis during growth spurts and following injury and it slows down through immobilization. This histological fact modulates the clinical choice to avoid long periods of immobilization post harm and to promote early movement from the thoracic to stimulate synthesis.
The tendon increases its potency from adolescence until about 30 years of age, after which it steadily declines in strength. It's believed that it is only about 60 percent as strong at age 60. Therefore, gross stomach injury happens in the over-30-year- old group and it's this group that endures the high percentage of tendon ruptures.
Types Of Injuries
There are quite a few possible pathologies that behave on a continuum in the event of an Achilles tendon rupture. The initial pathology is usually an irritation of the peritendon that develops into an injury to the tendon substance. As the tendon becomes more damaged, it will weaken and may then finally rupture.
The defining features of these pathologies are:
1. Peritendinosis
a. Edema and scarring of paratenon (fatty areolar tissue around tendon);
b. Acute pain and swelling;
c. Seen in runners who increase distance or change surface.
2. Tendinosis
a. Intra-substance degeneration of tendon;
b. Occurs when the tendon is subjected to high cyclic loads and does not repair between loads.
3. Tears (partial or complete)
a. Vulnerable zone of avascularity 2-6cm above calcaneal insertion.
1. Peritendinosis
a. Edema and scarring of paratenon (fatty areolar tissue around tendon);
b. Acute pain and swelling;
c. Seen in runners who increase distance or change surface.
2. Tendinosis
a. Intra-substance degeneration of tendon;
b. Occurs when the tendon is subjected to high cyclic loads and does not repair between loads.
3. Tears (partial or complete)
a. Vulnerable zone of avascularity 2-6cm above calcaneal insertion.
Demographics
The normal sufferer of an AT rupture is a 35-40-year-old male. Males rupture their ATs in a ratio of 10:1. This might be partly hormonal and mostly behavioral (that is, this age group may generally still be quite active). AT rupture in this age category is much younger than in other tendons such as the supraspinatus from the shoulder which will dominate from the 50+ age category. In the end, AT ruptures can often happen in middle aged men who have had some time away from competitive sport for a 5-10 year period who subsequently return to social sport.Ball sports like tennis and basketball have a tendency to control the cohort of those suffering an AT rupture since these sports involve abrupt dorsiflexion or plantar flexion force from a dorsiflexed position. Common offending functional moves might be stepping right into a pot hole, sprinting off the baseline in landing or tennis and leaping. This mechanical force is usually coupled with a degenerative element that ends in a weakened tendon because of repetitive micro-trauma and hypovascularity of this tendon. The inherently weaker limb using a sudden implemented force then ruptures. Interestingly, professional athletes only form a small fraction of those suffering rupture, together with recreational athletes comprising the majority of ruptures.
Furthermore, it has also been proven that quinolone antibiotics and long-term corticosteroid use might increase the risk of tendon rupture. Finally it's been found that the COL1A1 TT genotype protects an athlete from an acute soft tissue rupture, AT ruptures included. This could drive future studies in using chemical analysis to predict high risk groups for tendon rupture (Collins et al 2009).
Signs & Symptoms
SubjectiveThe vast majority of acute ruptures clarify no preceding symptoms of malfunction or pain from the Achilles. Although Achilles pain isn't a predictive indication of future tendon rupture, the proportion of patients who have pre-rupture symptoms does rise with age.
The majority of ruptures are typical with respect to their own symptoms and physical signs and also the mechanism is generally straightforward. The first sensation is really a sharp pain and they may feel/hear a snap- ping sensation. The sufferer will commonly complain that they've taken a hit to the back of the calf as though they have been kicked or hit with a tennis racket. This may replicate a sharp stabbing pain that then subsides to no pain, and it's possible that up to a third of patients have painless ruptures. But, walking can then replicate the pain especially as they try to push off the toes and they will be grossly weak in their push-off.
Objective
Often the clinician will feel a real difference in the tendon with potential instant swelling where the AT should be. They may observe that the calf muscle can pack up into the calf; however, this may be jaded by swelling and edema after a few hours. The website of this palpable defect is usually 2-6 cm above the heel bone.
Functionally they will hobble and find it hard, if not impossible, to push up on the foot. But a percentage of ruptures may be missed since the individual may continue to have the ability to push off using their toe flexors or if the plantaris has been uninjured.
This is achieved by squeezing the calf to mimic a jet contraction that then should transmit pressure to the Achilles and make plantar- flexion in the foot. With no Achilles, force isn't sent and plantar flexion does not occur.
Imaging
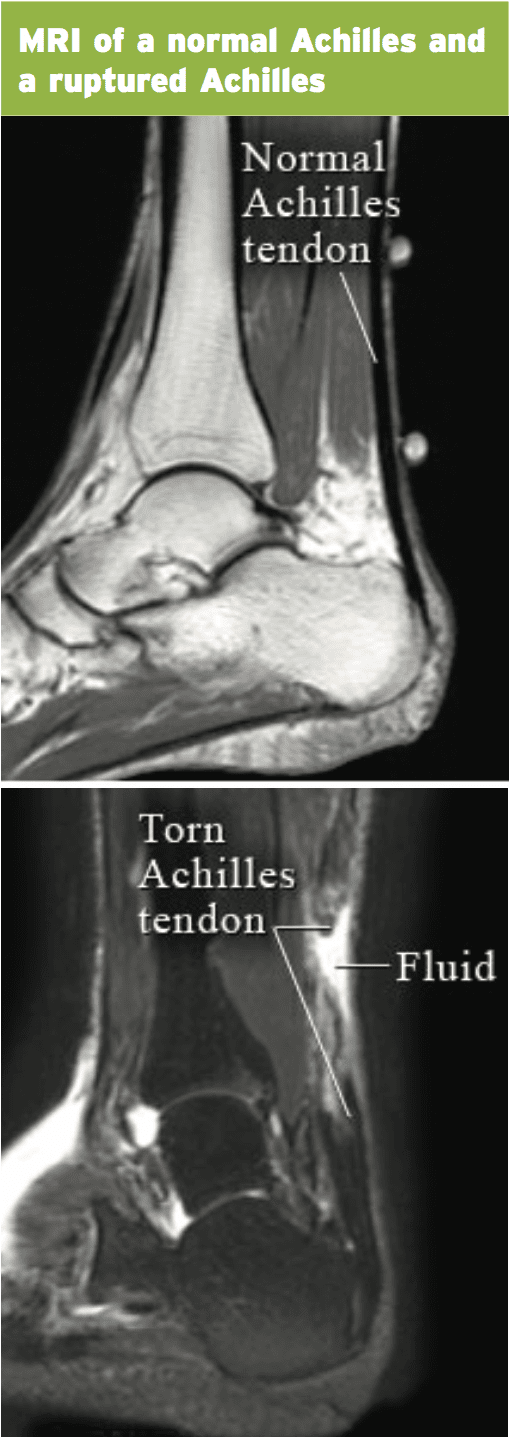
It's also useful for viewing the total amount of tendon available that can allow approximation of the tendon ends with an allograft if surgery is the preferred treatment option. Ultrasound will reveal thickening and hypoechoic areas in partial thickness tears. Full thickness tears will show posterior shadowing (because the sound beam is refracted in the thoracic ends) and also reveal retraction with tendon debris. Ultrasound may also show fat herniation.On the MRI a torn tendon will reveal equilibrium on the T2 picture whereas in degenerated tendons they will show a dark area on T2.
Differential Diagnosis
Although diagnosis of a whole tendon rupture should be relatively simple, a few differential investigations may confuse the examiner. These include:1. Flexor hallucis longus tendon rupture;
2. Plantaris rupture;
3. Tibialis posterior rupture;
4. Calcaneus fractures.
Treatment
Conservative cast immobilizationThe decision to manage a ruptured AT depends on a number of interacting factors. These include:
1. The length of the tendon diastasis (separation) – anything below 5mm diastasis may do well with conservative management;
2. Sport – surgeons tend to lean towards surgery in power athletes (sprinters, foot- ballers, rugby players) as the amount of tendon force encountered due to calf muscle contraction will be high. Although the tendon will still heal quite well if managed conservatively, it is felt that functionally a conservatively managed tendon will ‘stretch’ out and this will affect force transmission across the myotendinous junction. Inactive individuals may do well with conservative management;
3. Age–older patients tend to be less active than their younger counterparts therefore exposure to high tendon force will be less in the older population;
4. Country – it is still common for Scandanavian countries and some European countries to prefer conservative management in AT rupture.
Conservative functional management still has great results when compared with surgically-repaired tendons. Thermann and Zwipp (1989) compared 19 operative tendons versus 25 functionally-managed ruptures with a specialized walking boot and also found that results are comparable if the flaw is less than 5mm in length. After 25 weeks, patients in the two groups had complete healing free of re-rupture and the role- ally controlled group resumed sport much sooner than the operated group.
Mattila et al (2013) collected information over a 25-year period in Finland and found that the speed of surgically-treated AT ruptures had declined markedly through the years, suggesting that surgeons are leaning towards non- operative treatment more frequently and enjoying good functional outcomes.
More modern walking boots together with the capacity to control the angles of dorsiflexion have led the progress of competitive operational rehab in conservative AT management. The standard protocol may be to cast immobilize for 2-3 months and then to remove the cast and employ a functional prop (Aircast or CAM walker) with the ankle originally limited to 10-20 degrees of plantar- flexion (or even utilizing heel wedges in an Aircast) and then gradually opened up (or wedges gradually removed) over an additional six- week interval. Therefore, the individual will be liberated to mobilize normally 8-10 weeks post injury. The subsequent strength program will be like this program described further on in the surgical management of AT rupture.
Surgery
The decision to work to surgically repair a ruptured AT depends on the factors mentioned above under conservative management. In the end, if the clinical decision for surgery is indicated, the results are fairly similar to conservatively managed patients. The kind of operation used and the immediate immobilization protocol will fluctuate depending on the surgeon and the anticipated compliance of the patient.It's common practice now to allow operational mobilization post-surgery through use of a functional walking boot (see Aircast previously). Surgery followed by early mobilization at a functional walking boot has shown better results than just immobilizing the tendon using a cast for 2 weeks. Early mobilization reduces re-rupture rates and also individual compliance is better using a practical walking boot. The post-surgical limb is braced at a situation of plantar flexion originally to offload any stretch to the tendon via the use of heel wedges, and the wedges have been gradually removed over the interval the practical boot is worn. When the boot is eliminated, it is frequently suggested that a single wedge is utilized and slowly removed two months after removal of this boot.
Most surgeons will utilize one of two variants for surgery: either open or percutaneous.
The vast majority of surgeons will urge post-surgical blood thinners (warfarin) and antibiotics.
Rehabilitation
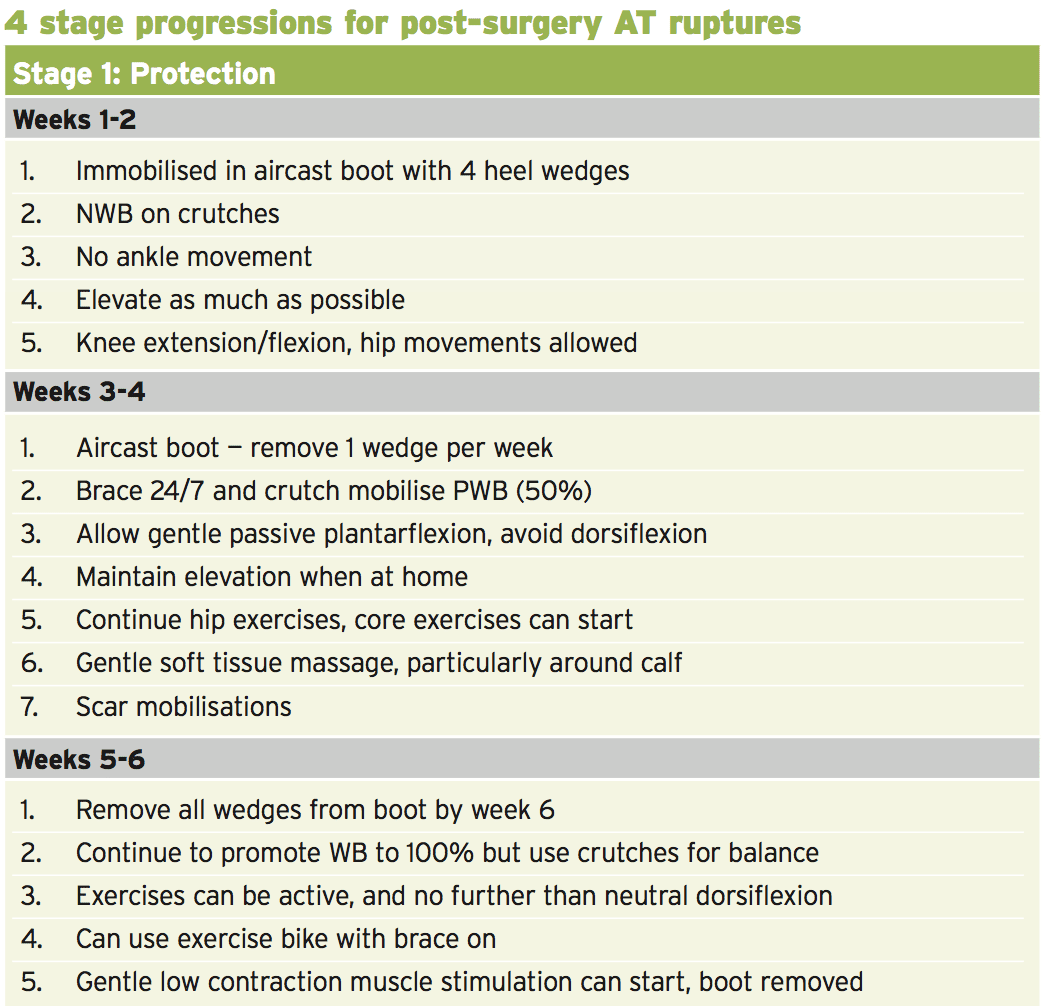
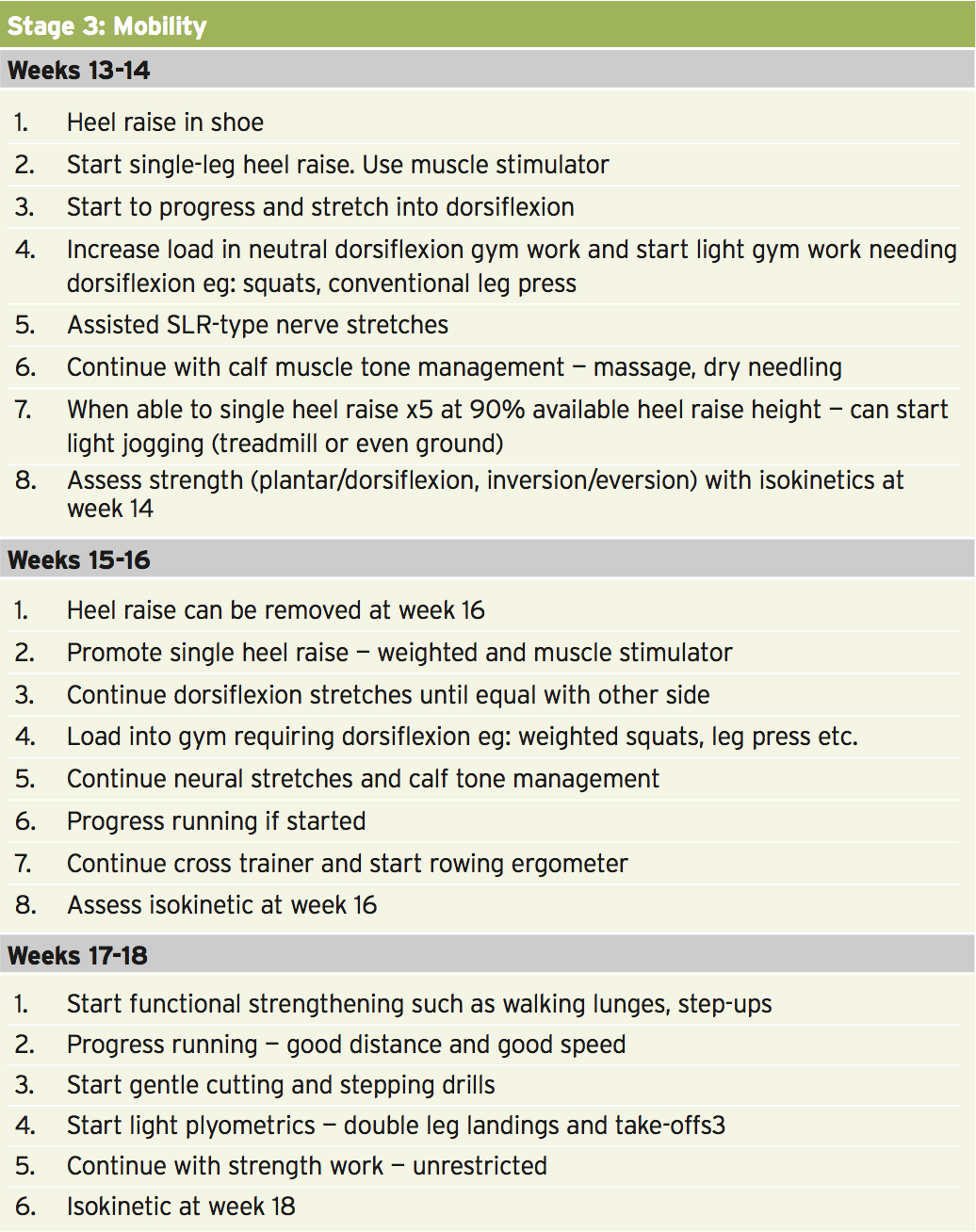
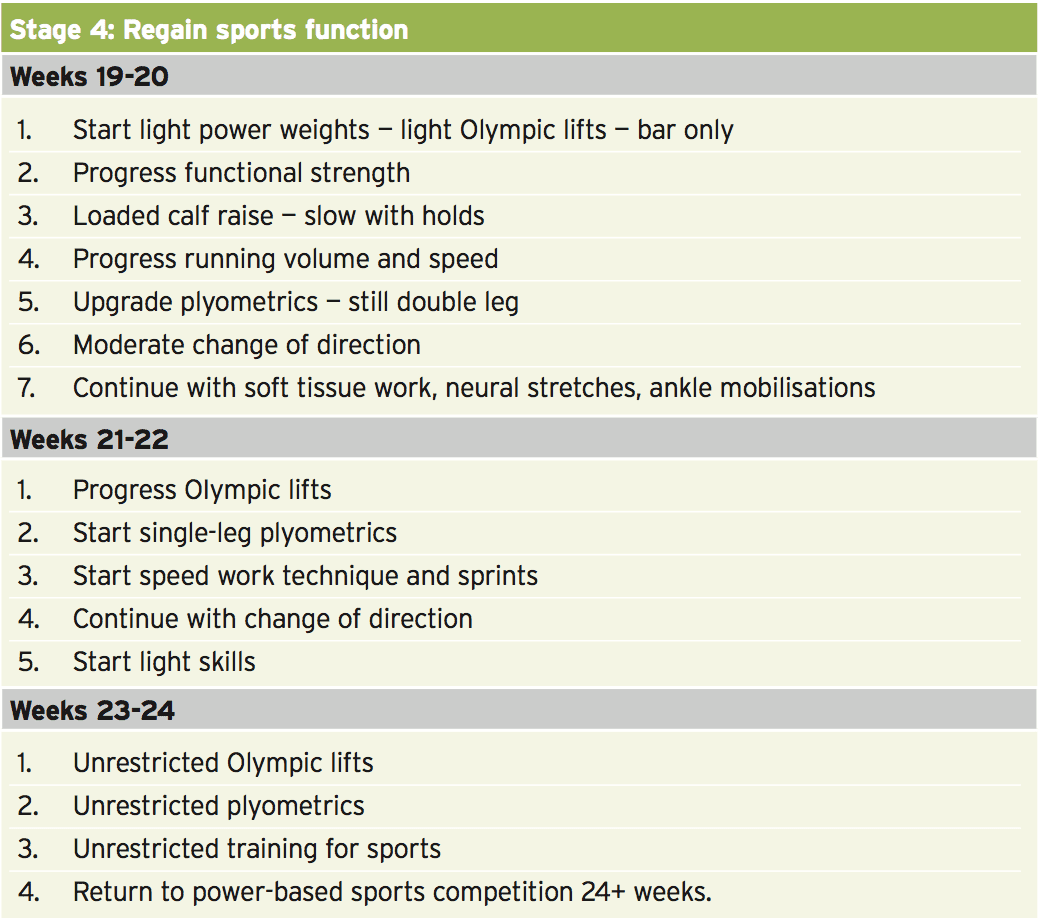
The approved time frame to come back to pre- accident levels ranges from 5-9 months depending on the athlete. Just like most long-term rehab protocols, the rehab stages can be broken down into progressive six-week stages (described below). The particular goals post- surgery are:
1. Range of movement
This is purposely limited initially to allow full tendon healing; therefore, the patient will be functionally limited to avoid dorsiflexion in the early stages. However, long term the range of movement does return quickly and it is uncommon to suffer long-term stiffness in the AT. The biggest threat to a good outcome is tendon elongation, thus it is important to limit dorsiflexion range in the early part of the rehab process.
2. Strength
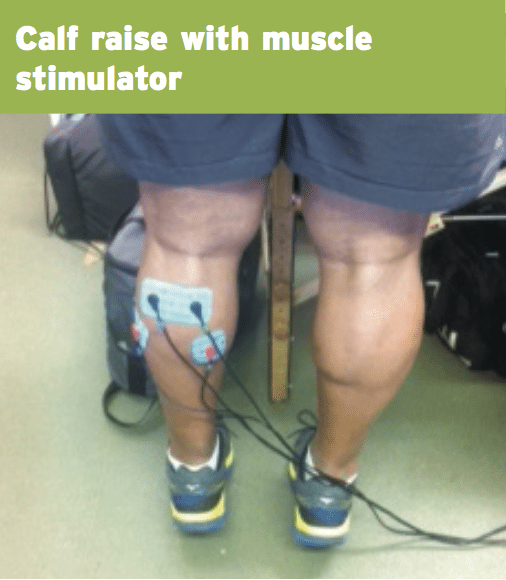
This is the most significant complication of an AT rupture. It is important to start some gentle isometric calf exercises early in the rehab process and to progress the calf muscle contractions quickly through the rehab process. It is not uncommon to see a permanent 10-30% strength deficit from the non-affected side.
3. Function
The earlier post-surgery the patient is able to weight bear and mobilize safely in a walking boot, the less complication they will have when they start running.
This is purposely limited initially to allow full tendon healing; therefore, the patient will be functionally limited to avoid dorsiflexion in the early stages. However, long term the range of movement does return quickly and it is uncommon to suffer long-term stiffness in the AT. The biggest threat to a good outcome is tendon elongation, thus it is important to limit dorsiflexion range in the early part of the rehab process.
2. Strength
This is the most significant complication of an AT rupture. It is important to start some gentle isometric calf exercises early in the rehab process and to progress the calf muscle contractions quickly through the rehab process. It is not uncommon to see a permanent 10-30% strength deficit from the non-affected side.
The earlier post-surgery the patient is able to weight bear and mobilize safely in a walking boot, the less complication they will have when they start running.
Conclusion
AT rupture is a relatively uncommon long- term accident suffered primarily from the 30-40- year- old male. The causative factors include pre-existing limb degeneration combined with high mechanical pressure due to forced dorsiflexion and/or strong plantar flexion from a dorsiflexion posture. Therefore it's more widespread in mid sized runners, tennis players and basketball players.The AT rupture may be handled either conservatively through utilization of a practical boot such as an Aircast boot or CAM walker, or operatively via a number of surgical options. In either case, the rehabilitation period is protracted and may take as little as five months or as long as nine months based on type of direction and physical characteristics of their athlete and the game involved.
The key feature of return to game post- injury will be gross strength, tendon elongation and how these influence on purpose. The majority of post-injured AT ruptures return to game within six months and the risk of re-rupture is comparatively tiny.
References
1. Thermann H and Zwipp H (1989) Achilles tendon rupture. Orthopade. 18(4); 321-333.
2. Mattila et al (2013) Declining incidence of surgery for Achilles tendon rupture follows publication of major RCTs: evidence-influenced change evident using the Finnish registry study. British J of Sports Medicine. 0; 1-4.
3. Collins et al (2009). The COL1A1 gene and acute soft tissue ruptures British Journal of Sports Medicine. 44; 1063-1064.