Science based therapist, Dr. Alexander Jimenez looks at the anatomy and biomechanics of this quadriceps muscle and how to evaluate and treat injuries.
Strains of these proximal quadriceps happen in sprinting (particularly the acceleration stage), jumping and kicking a ball. With four muscles containing the quadriceps group, the rectus femoris is the more common muscle to pressure as the muscle moves over two joints and consequently is intimately affected by both hip and knee posture, whereas another vastus muscles are just influenced by knee motion and knee posture.
Strains into the rectus femoris seem to affect sports like football (soccer), Gaelic football and Australian Rules foot- chunk (AFL) due to the repetitive sprint efforts involved, the repetitive kicking involved, leaping and shooting during the match and the length of period of a common match (90+ minutes) highlighting exhaustion as being a prevailing element.
Rectus femoris muscle injuries have a tendency to take longer to heal than other muscle injuries such as injuries and also can be debilitating to the athlete, along with the re-injury rate is high particularly from the 'tendon' injuries.
Anatomy Of The Rectus Femoris Muscle
The anatomy of the rectus femoris is exceptional in that It's comprised of two limb heads which originate on the pelvis:1. The straight (direct) head that runs directly in the anterior inferior iliac spine (AIIS); and
2. The reflected (indirect) head that begins deeper on the hip joint capsule and anterior labrum.
The direct head blends with the rectus femoris muscle to form a muscle, which looks like the quills on a pen as the fibres run on one side of the anus. The head to form a tendon is then joined by the head that is direct. The head that is direct creates the shallow portion of the conjoined tendon and blends anteriorly with the anterior part of the muscle.
The indirect head forms the tendon that creates a muscle and passes through the rectus femoris muscle. It maintains its central position, as it mixes together with the muscle of the rectus femoris and the tendon spans downwards about two-thirds the length of the muscle. A good analogy of central tendon and the rectus femoris would be a dog: the muscle is represented by the meat. The presence of the tendon within the rectus femoris gives it a 'muscle in a muscle' look within the muscle belly.
As the tendon disappears two- thirds down the rectus femoris, the muscular belly and the tendon which creates the patella tendon and folds on the tuberosity of the tibia proceeds and blend.
Biomechanics
The rectus femoris spans two joints (hip and knee) and operates over a great selection of movement due to the broad excursions of hip flexion/extension and knee extension. It is subject to bizarre loads in twisting and sprinting, and is comprised of a large proportion of fast-twitch fibers, suggesting that it is a significant manufacturer of hip muscle power in hip flexion.The mechanism of injury is acceleration as its swing phase is started by the leg, in sprinting. At this stage of the cycle, the rectus femoris is eccentrically loaded as the knee is loaded as the hip begins to bend at the start of swing phase and starts to bend in the end of stance and into swing phase. The muscle is subjected to two opposing forces in this point of the cycle - a high eccentric load due to knee flexion as well as concentric load at the hip flexion stage.
The other common mechanism of injury is kicking. The phase is characterized by quick hip extension and knee flexion to kick a ball. Accelerated muscle action subsequently follows this later in the cycle that the knee goes to maneuver the foot into place to kick the ball and as the hip flexes to create hip torque. The ball contact phase then puts a sudden and large load on the rectus femoris in a position of quick muscle shortening.
It has been indicated that hip flexion strength is significantly more significant in reaching a distance, than knee extension strength. The rectus femoris takes up to a larger level then acceleration of their leg through hip flexion in the event the iliopsoas does not produce enough power. Therefore, injury and/or weak- ness in the iliopsoas may be a precursor to femoris injury.
During kicking the stance leg may suffer an accident. As the kicker plants the non-kicking foot, the quadriceps and hamstrings stabilize the knee. Since the pelvis then proceeds to move forward over the position leg, then the stance leg hip is taken into expansion since it functions to command the hip extension, and also a top load is set on the rectus femoris. As the leg moves right into flexion, further load is placed on the stance leg, and also also the stance leg muscles work hard to stabilize and manage the transmission of electricity throughout the pelvis and trunk onto the leg. Interestingly, the speed of muscle strain seems to be higher. A potential explanation is that surfaces allow for ground traction on the stance leg and thus higher forces are dissipated via the stance leg hip.
Lumbopelvic stability seems to play a part in the incidence of rectus femoris strain. Kicking and sprinting require a lumbopelvic platform so as to be able to transmit the large forces involving the back and the thighs. Bad management of pelvis and the lumbar spine will lead to load. In consequence, if the athlete cannot generate enough abdominal strain to form a stable pelvis to sprint or kick a ball, the rectus femoris (amongst others) will be required to boost its force production to compensate for the lack of abdominal control.
Injuries To The Rectus Femoris
A number of differential rectus femoris injuries exist. The discussion will concentrate on:- 'bull's eye' lesions
- Peripheral rectus femoris strains
- rectus femoris tendon injuries -- one-tendon harm and complete ruptures.
Bull's eye Lesions
The central tendon which divides the two heads of the rectus femoris muscle separates from the direct mind of the tendon and runs upward through the muscle. An injury to the tendon that was blended to its own contribution and the mind is termed a 'bull's eye' lesion as it has a resemblance to a bull's eye.As no pathology is present in the direct mind and its own contribution to the central tendon in this instance the tendon is still intact. As this indirect mind of the central tendon is injured, a fibrotic scar forms around this tendon that then gives the appearance of a chronic 'bull's eye' on MRI imaging. New muscle-tendon junctions shape round the central tendon widening the interval between the muscle and the tendon that is central.
Histologically the damaged tendon demonstrates dense mature fibrous tissue with edema. The region fills in with damaged and normal muscle fibers to create fresh 'pseudo'- muscle tendon junctions.
It's recognized that these kinds of injuries predominate in kicking-based sports like AFL football and Gaelic football, and contribute to longer rehab periods.
Tendon injuries
Partial injuries
Partial tears of the rectus femoris present as acute onset thigh pain. Uncomfortable and although painful, these may not be limiting to the athlete at the brief term. They could be able to compete with a distress in the thoracic and they can notice they cannot get exactly the space on the kicks. The athlete may detect pain, weakness and disorder, as they become chronic.One-tendon tears
The reflected/indirect head will be involved with a one-tendon rupture whilst the head stays intact. This can create a type effect as the ruptured reflected head goes against the head that is whole.Complete tears
Although rare tears of the two heads might happen. It's been revealed that the extreme duration of the rectus femoris tendon (nearly two-thirds the length of the quadriceps) make it unlikely to be completely torn.It is more common to rupture the indirect head and in the event the direct mind is involved it will be a two-head rupture of direct and indirect head.
Signs & Symptoms
In any of the demonstrations, the patient subjectively complains of:- a tender anterior thigh
- weakness in the hip with hip flexion lack of function with acceleration and kicking.
- a ‘tearing’ sensation or ‘popping’ sensation in complete tendon tears
- a noticeable retraction of the muscle distally if ruptured.
Clinical Assessment
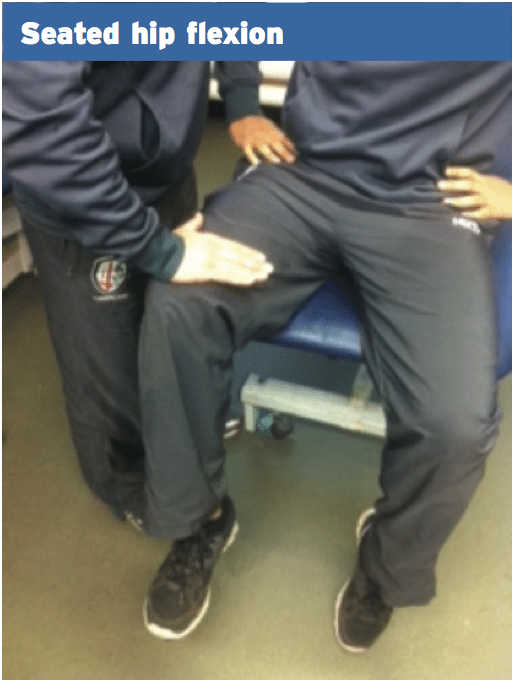
The examination begins with viewing any noticeable defects . With muscular retraction and ruptures it'll be common to observe a lump form in the thigh muscle as the stomach of the muscle pulls down as a result of tension generated in the long rectus muscle. Tests for the rectus femoris include:1. Seated hip flexion. This is an inner-range muscle test that is quite sensitive to rectus femoris tendon injuries. This will demonstrate fatigue and pain in the event of an injury. The athlete is asked to maintain the knee over the knee by 2-3 inches and the assessor pushes downward on the thigh requesting the athlete to meet with up with the pressure.
Investigations
The standard investigation is MRI using T2 T1 and fat suppression images in axial plane and the coronal plane. Axial T2 with reduction is in identifying strain injuries to the rectus 18, easily the image and they'll show high signal . MRI will show perifascial fluid, muscle fiber disturbance, T2 hyper-intensity and scarring/fibrosis.Grade 1 breeds is compatible with interstitial hemorrhage and edema and will show a appearance on all pulse sequences. Grade 2 strains show partial disruption of the M-T intersection with feathery interstitial high signal. Grade 3 tears show complete disruption and retraction of the tendon. Bull's eye rhythms reveal glowing high sign surrounding the low- signal tendon on axial T1 or fluid-sensitive sequences (Gyftopoulos et al 2008).
MRI will assist in identifying a number of attributes:
- exact location of the injury
- the size of the injury. Both the cross- sectional area (CSA) and also the length of the injury (cm). The size of the injury is predictive of time to return to sport
- visualize if it is central tendon vs peripheral rectus femoris injury.
Rehabilitation Of Muscle Strain Injuries
There is no universally approved management strategy for muscle strain injuries in the rectus femoris. What's accepted is that 'bull's eye' lesions do take longer to heal than muscle-tendon injuries and straightforward muscle. Ruptures that are complete will be discussed later in this particular piece.
Stage 1: Acute management
1. RICE and crutches for first 48 hours.
2. Physiotherapy: soft tissue therapy to rectus femoris as it develops widespread trigger points in presence of injury.
3. Stretching: generally aggressive stretching is avoided in the early rehab phases as it does seem to delay healing, in contrast to hamstring strains that tend to do well with early stretching.
4. Strengthening: limited to knee extension initially.
5. Pelvic balance: regular chiropractic, osteopathy and soft tissue therapy (massage and dry needling) will be necessary to balance the pelvis and the muscles that contribute to pelvic muscle tone such as the iliopsoas, adductors, TFL and gluteals.
6. Core stability: low-level activation of the deep spinal stabilizers can be instigated at this point.
7. The time frame for this stage on acute muscle-tendon strains can be variable and between 4-8 days.
1. RICE and crutches for first 48 hours.
2. Physiotherapy: soft tissue therapy to rectus femoris as it develops widespread trigger points in presence of injury.
3. Stretching: generally aggressive stretching is avoided in the early rehab phases as it does seem to delay healing, in contrast to hamstring strains that tend to do well with early stretching.
4. Strengthening: limited to knee extension initially.
5. Pelvic balance: regular chiropractic, osteopathy and soft tissue therapy (massage and dry needling) will be necessary to balance the pelvis and the muscles that contribute to pelvic muscle tone such as the iliopsoas, adductors, TFL and gluteals.
6. Core stability: low-level activation of the deep spinal stabilizers can be instigated at this point.
7. The time frame for this stage on acute muscle-tendon strains can be variable and between 4-8 days.
Stage 2: Restrengthening
1. Continue with soft tissue management of rectus femoris tone as well as pelvic muscle balancing.
2. Continue with and progress core stability training.
3. Attempt to achieve full strength in knee extension prior to hip flexion. The strength programs can run in parallel for the knee extension power and hip flexion power; however, delay strong hip flexor work until the athlete has knee extension strength and achieves full range. Some examples of rectus femoris strength exercises are shown below.
4. This stage may run over 7-10 days depending on presentation.
Stage 3: Return to running
1. Full stretch on passive knee bend (PKB) in prone.
2. Full hip flexion power (inner range) in sitting as compared to the opposite side.
3. Able to hop 3 x 10 pain free.
4. Hip flexion strengthening and continue to run in parallel with a return to running program.
5. Running retraining is performed on alternate days (train high/train low days).
a. Stage 1: easy 2km jog pain free
b. Stage 2: 30-20-30m (acceleration/ hold/deceleration) 3 x 4 reps. Build to 100% over a number of sessions.
c. Drop acceleration distance down to 20m, therefore 20-20-20m 3 x 4 reps at 100%
d. Once able to sprint, can incorporate long kicking and aggressive change of direction.
Progress is variable depending on lesion in muscle strain injury. Timeless muscle strains or M-T junction strains that are mid-thigh can advance. Bull's eye lesions have a tendency to take longer and therefore are influenced by ongoing pain, weakness and disorder. Cross et al (2004) set fundamental tendon injuries return to play as being 14-43 (average as 27) days and peripheral breeds as being placed at 5-15 times to return to play.
The proposed reason for that is protracted return to play with fundamental tendon injuries is due to the shearing effect of the central tendon (indirect head) with the direct head. The central rib almost creates when injured a muscle in this distinctive anatomical arrangement and a muscle creates the shear effect that is undesirable. Therefore the shear effect does not happen to the tendon, the damage isn't in peripheral rectus injuries.
Return To Play Protocol For Surgically-Repaired Rectus Femoris Injuries
In the event of complete indirect head rupture and/or direct head rupture, a surgical outcome may be considered necessary to return the athlete to full function. The rectus femoris tendon can be exposed surgically and repaired with anchor sutures that allow continuity between the torn tendon ends. The typical time frame for a surgical repaired rectus femoris rupture is 12-15 weeks.
The rehabilitation time frame can be broken down into 3 x 4-5-week stages.
Stage 1: Protection (4-5 weeks of range of movement and weight- bearing limitation)
The rehabilitation time frame can be broken down into 3 x 4-5-week stages.
Stage 1: Protection (4-5 weeks of range of movement and weight- bearing limitation)
- The athlete will initially be placed in a knee motion-limiting brace to prevent any knee flexion that may ‘stretch’ the repaired tendon. This may be in place for up to four weeks.
- The athlete will be instructed to avoid any hip extension past 10 degrees of flexion initially. The range of hip exten- sion will be gradually allowed to increase over the initial four-week period so neutral extension is achieved by four weeks post-repair.
- The athlete will be non-weight-bearing and partial weight-bearing for the initial four weeks. Aim to achieve full weight- bearing by 4-5 weeks post-op.
- The athlete will require soft tissue therapy to mid and distal rectus femoris.
- Maintain hip mobility into flexion, rotation and abd/adduction.
- Muscle stimulator can be used on rectus femoris in protected position and in disuse atrophy mode only. No strong contraction.
- Gradual increase in range of movement and loading through the proximal hip into flexion.
- Focus on low load and low speed with a gradual increase in both over a 4-5 week period.
- Continue manual therapy to improve hip mobility and soft tissue to rectus femoris to improve tissue compliance.
- Direct scar massage to improve fascia and scar tissue compliance.
- Progress and develop concentric strength prior to eccentric strength.
Theraband Isometric Hip Flexion & Concentric Knee Extension
- Actively take the knee from flexion into extension. This is concentric and then eccentric rectus femoris using the knee as the moving segment.
- Perform 3 x 20 reps. Slow and controlled reps with abdominal activation.
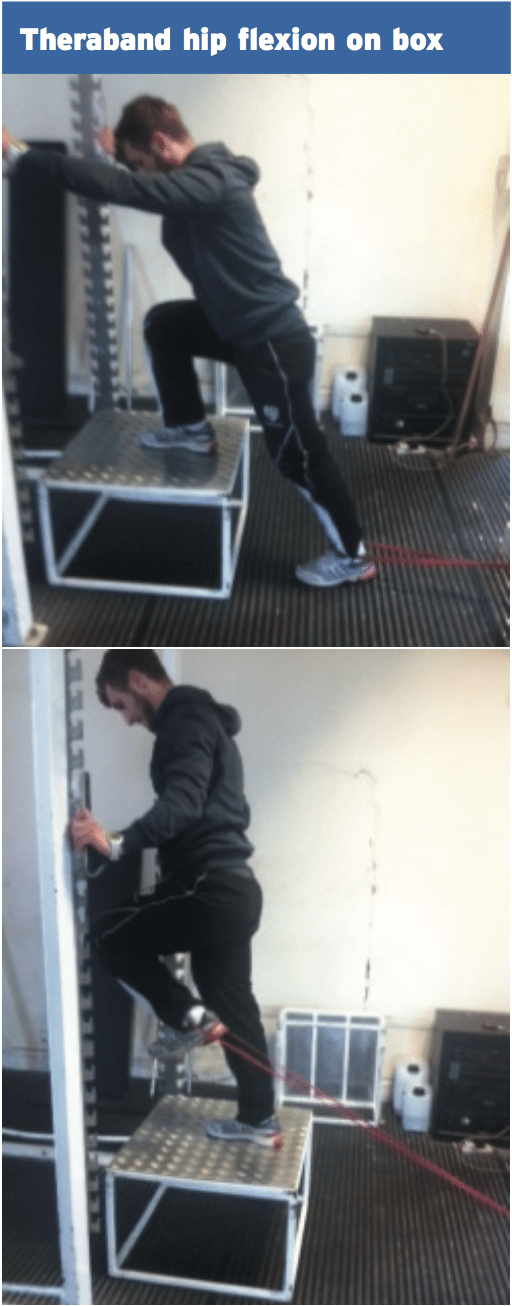
Theraband Hip Flexion On Box
- Wrap a band around the affected foot.
- Stand on a box with hip in full extension.
- Drive the affected hip up into flexion.
- Hold and return to start position.
- Perform 3 x 10 reps. Increase effort with thicker bands.
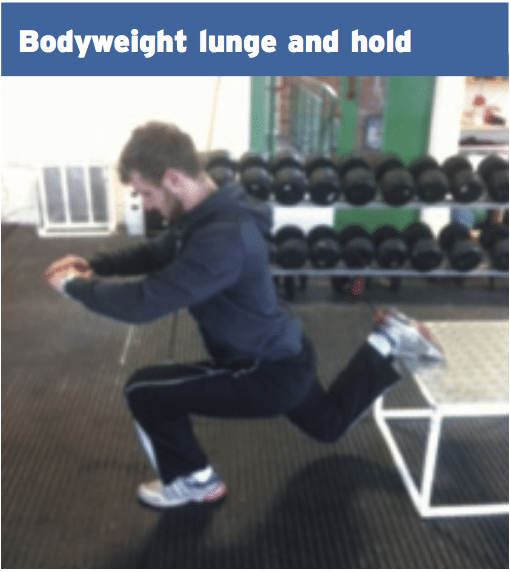
Bodyweight Lunge & Hold
- Split the stance on a box. This is a split squat position.
- Slowly descend so that the thigh approaches parallel to floor position.
- Hold and return to start position.
- Perform 3 x 10 each leg.
- Bodyweight step-ups and step-downs
- Start and quickly develop posterior chain strength and hip abductor/ adductor strength.
Stage 3: Return to function (4-5 weeks)
- Progressively load anterior hip.
- Functional leg strength – squats, dead- lifts, lunge, step-ups.
- Start eccentric focus on rectus femoris:
Reverse Nordics
- Kneel on floor.
- Keep hips in neutral extension.
- Slowly lower backwards taking knee into more flexion. This loads the rectus femoris eccentrically.
- Perform 3 x 10 and increase speed as a progression.
Ball Bounce
- Bounce a medicine ball off the knee.
- Start with 2kg ball and progress the ball weight as strength improves.
- This trains rapid eccentric hip flexor in a shortened position.
- Work on sets of 10-15 reps.
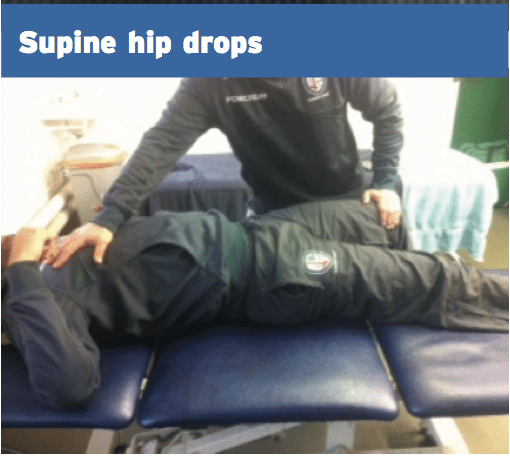
Supine Hip Drops
- Hold affected hip in slight flexion.
- Forcefully push clients hip into extension and direct them to hold your pressure.
- Increase amount of push and depth of thigh to increase extension component.
- 3 x 15 reps, rapid contractions.
- Return to running
- Pool jog – high knee drive
- Alta G if available 70-80% BW Field base run through. See above plan for return to running post-strain injury.
- Interval training
- Active deceleration over short distance
- Agility
- Return to kicking
- Progress soft ball to ball that is hard.
- Increase distance and quantity the flipping meniscus programs for femoris injuries.
Preventative Programs Rectus Femoris Injuries.
1. Identify at-risk athletes. Injury to preceding injury into the alveolar and the rectus femoris have been identified as risk factors. Also shorter athletes (less than 1.82cm) have a greater chance of quadriceps injury in addition to leg dominance in kicking.
2. Hip extension flexibility. An asymmetry in hip extension flexibility from left to right has been found to be a risk factor in rectus femoris injury. Poor hip extension flexibility in additional hip flexors like psoas and iliacus might be a precursor to rectus femoris injury. Greater hip torque needed for hip flexion from the association between the femoral nerve as well as the rectus and psoas was postulated to some risk factor for femoris injury.
3. Eccentric strength. The rectus femoris due to its biarticular arrangement is subject to bizarre loads in the knee flexion and hip extension in terminal position to swing phase as well as wind up for kicking.
4. Core stability. Keeping a stable toenails structure is necessary to prevent unwanted 'torque leakage' round the hips during kicking and extending. Unwanted excess anterior and posterior pelvic tilt because of inferior pelvic stability can predispose the rectus femoris to the changing of 'torque' to the hip flexors such as the rectus femoris due into a strain injury.
5. Training monitoring.
With systems like video tracking and GPS, it is possible to modify the athletes training load and intensity . It is anticipated that in the return to competition, the athlete/player may not be able to withstand the levels of volume and intensity as a non injured player in the same position. Trainers, the athlete along with all support staff have to be made conscious of training abilities that are anticipated early in the return to competition phase.
References
1. Cross et al (2004) Acute quadriceps muscle strains: MRI features and prognosis. American Journal of Sports Medicine. 32; 710-719.
2. Balius et al (2008) Central aponeurosis tears of the rectus femoris: practical sonographic prognosis. British Journal of Sports Medicine. 43; 818-824.
3. Mendiguchia et al (2013) Rectus femoris muscle injuries in football: a clinically relevant review of mechanisms of injury, risk factors and preventative strategies. Br J of Sports Med. 47: 359-366.
4. Gyftopoulos et al (2008) Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. AJR: 190.
5. Hassleman et al (1995) An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J of Sports Med. 23(4): 493-499.
6. Straw et al (2003) Surgical repair of a chronic rupture of the rectus femoris muscle at the proximal musculotendinous junction in soccer player. British J of Sports Med. 37: 182-184