Chiropractor, Dr. Alexander Jimenez looks at exactly what the recent study says concerning the identification and treatment of pelvic and hip anxiety fractures in athletes.
Stress fractures are a rare cause of pain in The overall sporting population with some reports indicating they account for just 2% of all reported accidents. A significantly higher incidence of stress fractures is observed in long distance runners and triathletes(1).
Stress fractures around the anus are Relatively rare but must be regarded as a differential diagnosis when athletes (particularly long distance runners and triathletes) accounts hip/groin or buttock pain during and after running. This article concentrates on stress fractures across the pelvic/ hip area including sacral, pubic rami and femoral neck. The anatomy, clinical presentation, diagnosis and therapy for each of these kinds of stress fractures will be discussed.
Why Stress Fractures Happen?
Stress fractures occur over time when bone can’t resist submaximal persistent forces. They’ve been described as either insufficient (if normal pressures result in fracture of a bone together with decreased bone density — ie within an elderly osteoporotic individual) or fatigue fractures (when abnormal stress is placed on normal bone plus a fracture happens — ie long distance runner)(2). This guide focuses on fatigue fractures.When bone is subjected to loading, then the Initial physiological response is a relative increase in osteoclastic activity (bone resorption) and thus temporary structural weakening occurs before new bone formation. If these stresses continue to occur without sufficient time to get the bone to adjust then continuing osteoclastic activity exceeds bone regeneration and microfractures happen(3).
The First feature of a pressure reaction Viewed on imaging is bone oedema on MRI, also increased action on bone scanning. Bone scan in the acute phase has high sensitivity but low specificity, and increased uptake may also be caused by disease, bone infarction or neoplastic action(4). Latshaw et al stated that 60-70\% of x-rays in the acute period of a stress fracture (less than 2 weeks) show a negative effect (5). Because of its lack of radiation, high sensitivity and higher specificity MRI (even though its higher price) is often the most favored modality to determine stress fractures at the early phases.
A Number of different intrinsic and extrinsic factors are identified as risk factors for stress fractures. These include, but are not restricted to, sneakers, biomechanics, nutrition, stamina, versatility and hormonal or menstrual disturbances. These all need to Be considered when analyzing a patient with a suspected stress fracture. Johnson et al found in their investigation of 8 female athletes with sacral stress fractures the most significant risk factor for these types of fractures was a quick increase in impact action with a more vigorous exercise plan(6 pounds). A spike in workload must therefore be regarded as a significant risk factor for a stress fracture.
Sacral Stress Fractures
Anatomy
The sacrum usually consists of 5 fused Vertebrae (S1-S5) and is triangular in shape (see Fig.1).) It contrasts with the ilium in the sacroiliac joint and also has been described due to its shape and its role in the supply of forces because the keystone to the arch of the anus.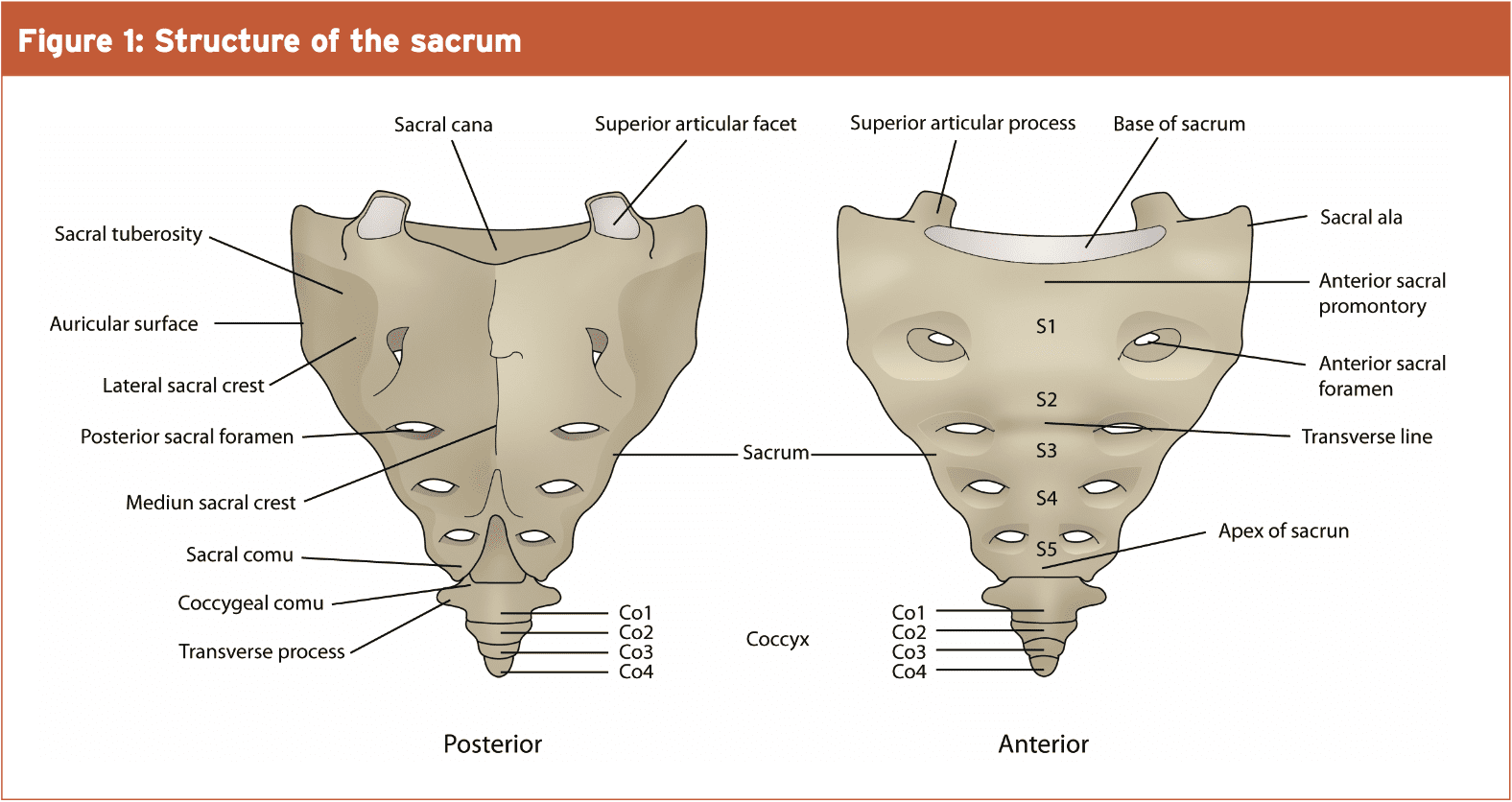
Figure 2 reveals the anatomy of the anatomy of the pelvis, and also how the sacrum (like an inverted arch) encourages the whole upper body weight and transports force into the pelvis.

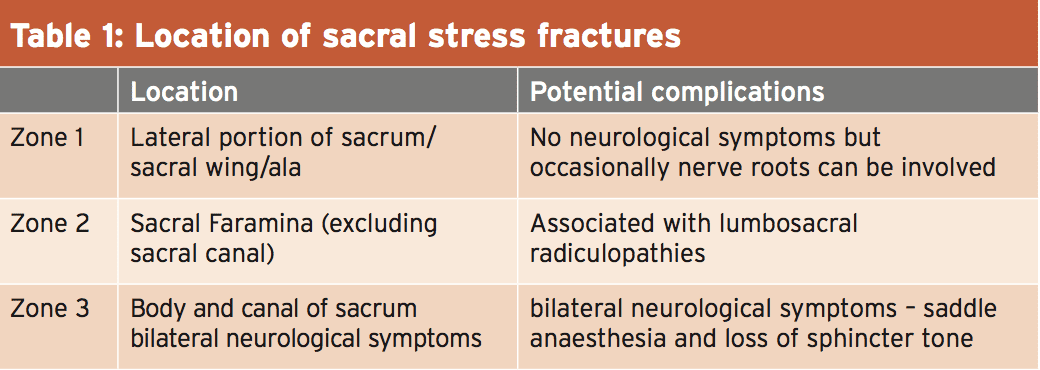
Fractures based on their place (see table1) (7).) Sacral stress fractures most often occur in zone 1 and therefore are more often seen in women. It has been suggested that the form of the female limb leads to less efficient weight reduction through the sacrum than the typical penile tissues(8pounds). But, it’s also true that several male elite Australian triathletes have endured sacral stress fractures in recent years.
Clinical Presentation
An athlete with a sacral stress fracture will Frequently present with acute onset back, buttock or hip pain they explain occurred suddenly during a jog and they will report that they had been not able to continue that run. They might have limited back motions, and might or might not have pain on palpation of the sacrum. Often they have no neurological symptoms. Pain or tightness will likely be experienced walking and they’ll have pain on leaping on the side. They also commonly report pain on single leg loading tasks — for example placing trousers on.Diagnosis
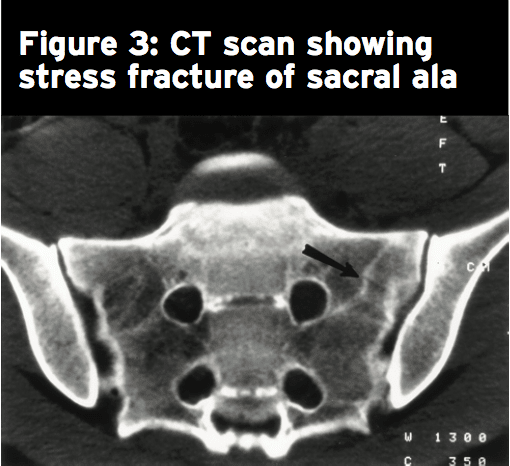
Because of the excessive overlying soft tissue, Complex bone anatomy and/or connective tissue, plain radiographs seldom show a sacral stress fracture(8). Bone scan, MRI or CT may be used to discover a sacral stress fracture; MRI is most frequently the modality of choice as a result of dearth of radiation. Fig 3 shows a stress fracture of the back ala. CT and MRI findings indicate that sacral stress fractures occur due to repeated compressive forces resulting in shear microfractures of their trabecular bone(6). These fractures seldom create a visible callus on plain radiograph therefore MRI or CT must be used to follow up imaging when inferior recovery is supposed(8).Treatment
As these are secure cracks, treatment Progression is largely depending on the athlete’s symptoms and can advance from non-weight bearing to weight bearing to slow return to operate as symptoms subside. Usually a span of 6 weeks with no running followed by a 6-8 week period of gradual return to running is demanded. Most published literature shows a full return to activity by 4 months, with rare instances taking 14 months(8).Repeated CT scans 4 and 8 months after Diagnosis often show no symptoms of previous fracture, which indicates a rapid and complete recovery of this well-vascularised trabeculae microfractures when compared to fractures that involve the less well- vascularised cancellous bone. Johnson et al showed that those girls who had the best diets, regular menses and fewer before anxiety injuries or menstrual irregularities healed the fastest(6).
Pubic Rami Stress Fractures
Anatomy
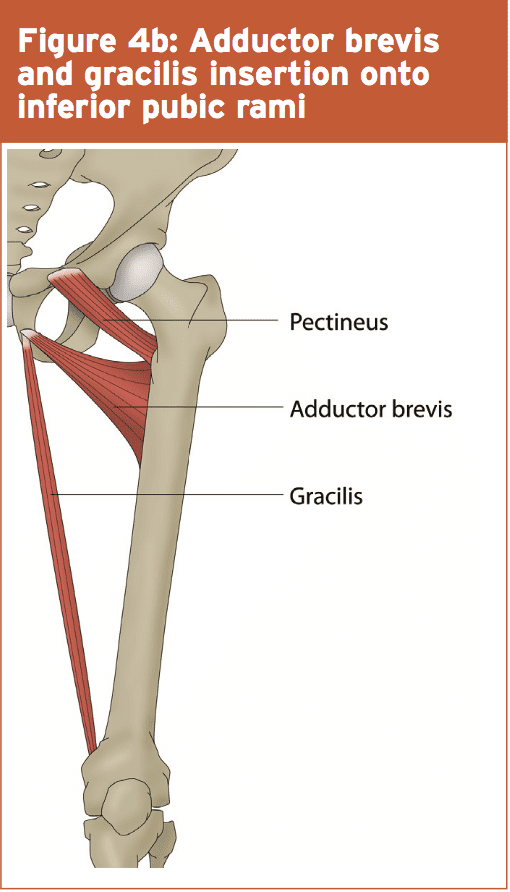
The inferior pubic ramus slopes down And medial out of the superior ramus, and becomes thin as it stinks. It’s the attachment site for the adductor magnus, brevis and gracilis as well as obturator internus and externus (see figures 4a and 4b). They generally occur in the inferior pubic rami adjoining to the pubic symphysis. Miller suggested that these fractures occur because of repetitive forces transferred to bone through muscle contraction or fatigue(9). In a study on female army recruits Hill et al proposed that over-striding throughout sanity was potentially a mechanism for pubic rami pressure fractures(10).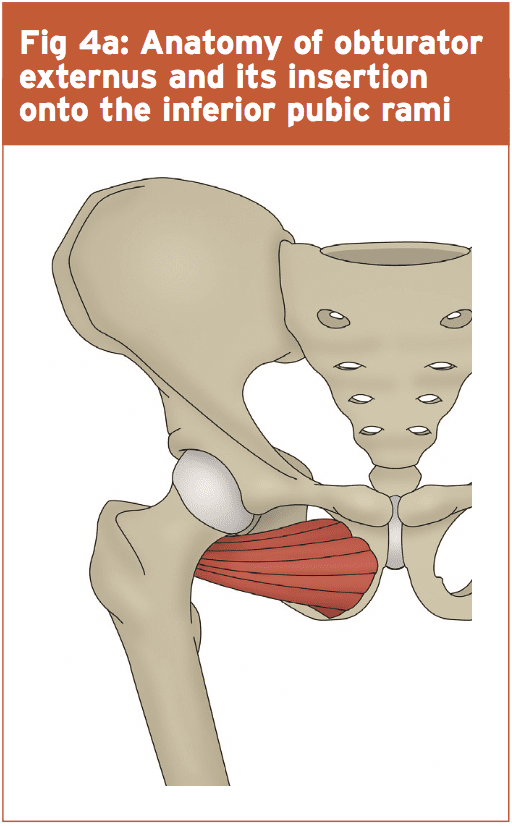
Clinical Presentation
These fractures often present in competitive races or even intensive coaching sessions. They generally occur in the back of the adductors and/or external rotators of the hip. Athletes with pubic rami pressure fractures may complain of pain in the hip, buttock, inguinal or adductor area that develops with activity and decreases with rest. They generally limp and on clinical testing suffer from passive hip abduction, resisted hip adduction and resisted hip external rotation. Noakes et al said that a stress fracture of the diaphragm might be made with confidence even without radiographic evidence in the following 3 criteria will be met(11)1) Running is impossible due to acute Discomfort in stomach region;
2) Discomfort in groin with kneeling position on leg (positive standing test);
3) Deep palpation revels exquisite, nauseating tenderness localized to pubic ramis.
Diagnosis
Plain radiographs may reveal undisplaced fracture lines however a lack of radiographic evidence in the early stages is not unusual. Bone scan, CT or MRI could be used to identify fracture and bone oedema could be evident on MRI.Treatment
These fractures have a high recovery rate following 6-10 weeks of rest however they have a small hazard of non-union and re-fracture when sufficient rest has not been undertaken(11). Those fractures which show delayed marriage will likely reveal complete recovery when further conservative direction is performed(9). Progression of treatment ought to be guided by pain and thus initially, crutches might be required if walking is painful.Femoral Neck Stress Fractures
Anatomy
The femoral neck is the flattened, pyramid shaped piece of bone that connects the femoral head to the femoral shaft. Athletes with femoral neck stress fractures may record hip/groin pain when running. This pain typically has an insidious onset and usually worsens with the intensity or length of a run. It can initially only happen at the end of a rush but while the stress reaction worsens the pain gifts earlier later on, and longer period is necessary after the jog to get symptomatic settlement. Athletes with femoral neck stress fractures can possess hip/ groin pain in rest, and may wake with pain at night. They frequently also report pain with rolling up in bed, active straight leg raise and single leg posture.
Diagnosis
Conventional radiographs are usually negative from the acute setting but might show signs in situations where symptoms are present for two weeks or longer.Treatment
As mentioned, tension side pressure fractures require instant orthopedic opinion due their risk of displacement. Compression facet fractures are often handled invisibly with safe weight bearing and ongoing monitoring to evaluate healing. Initial phases of management should include non-weight posture on crutches till no pain whatsoever, then advance to partial weight bearing to full weight bearing over a period of 4-6 months(10). A slow return to run program can be initiated at 8-12 weeks when the athlete can walk without pain/symptoms.Return-To-Running Strategy
With all stress fractures across the anus, A gradual return to run plan is an important component of the rehabilitation process. To ensure progressive loading with spikes in work load, then the yield to conduct plan ought to be at least as long as time off from working out. By way of example if an athlete had a knee strain fracture which took 6 weeks of no running afterward athlete requires at least a 6-week gradual return to running strategy before they might be at their previous conducting load.A Lower-limb strengthening program can be put into place quite early in the rehabilitation process initially beginning with non-weight bearing exercises, which may be improved as the athlete is in a position to weight bear with no pain. Early strengthening can help decrease muscle Loss and tackle any biomechanical difficulties. As the fracture heals and the tolerance for Load enhances, these exercises can be Developed to higher-load exercises to prepare the body to the return to working out.
References
1.BMJ Open. 2012 Nov 19;2(6)
2.Current Sports Medicine Reports 2006; Vol 5 37-43
3.Sports Medicine and arthroscopic review 2012. Vol 20 No 4 206-213
4.British Journal of radiology 2012; 85 1148-1156
5.American Journal of Sports Medicine 1981. Vol 9, No 1 54-57
6.American Journal of Sports Medicine 2001 Vol 29, No4 498-508
7.Clinicla cases in mineral and bone metabolism 2011; 8 (3), 19-23
8.Current Sports medicine reports 2007. Vol 6 39-42
9. Sports Medicine 2003; Vol33, No13, 1003-1012
10.Journal of Bone and Joint Surgery 1996. Vol 78, No3, 383-386
11.American Journal of Sports Medicine 1985. Vol 13, no 2 120-123