Introduction
Chondral surface defects in the knee are common in the athlete (2,3,7,14). It has been shown that approximately 63-66percent of knees which are investigated under regular arthroscopy will have some way of chondral defect either on the femoral condyles, posterior patella, trochlear groove or perhaps the tibial plateau (in some instances more than a chondral defect).Chondral surface accidents can affect all kinds of athletes from runners to athletes From the competitive cutting and pivoting sports such as soccer, tennis and court sports like netball and basketball. Injury to the articular cartilage between the femur and the tibia and the ribs between the patella and femur can happen due to sudden load like twisting on the knee in a lunge position, or it may result from persistent trauma as a result of small loaded knee flexion movements that breakdown the cartilage over time.
Most these chondral injuries are low grade cartilage fissuring which could be managed conservatively and don’t need surgical intervention. However, a cartilage injury at a knee may progress to more severe osteoarthritic changes if not managed properly and this may lead to more serious functional impairments as the athlete gets elderly(3,6,13). Because articular cartilage is avascular, the transportation of inflammatory mediators and cells to the site of tissue injury is restricted; consequently, cartilage has no intrinsic capacity to heal itself (12). Therefore managing cartilage defects in athletes is getting more widespread attention in the literature.
Chondral Lesion Pathophysiology
Articular cartilage is the white, shiny covering tissue that covers the end of long bones and is made up of chondrocytes (articular cartilage cells), water, proteoglycans and collagen. At the knee that this hyaline cartilage covers the femoral condyles, the tibial plateau and the posterior surface of the patella and these are collectively called ‘chondral’ surfaces. The frictional coefficient of articular cartilage was compared with being five times easier than rubbing ice on ice. This enables an extremely smooth gliding surface and reduces the shear force across 2 bones. A large part of the cartilage is both fluid and so it is also capable to withstand compressive forces very well because the fluid is able to ‘move’ under the load and absorb this load (19). With this specific capability to distribute load, peak pressures imposed on subchondral bone are minimized. However regardless of the durability of thoracic below normal joint loading, excessive joint loading may harm it, causing loss of joint motion, instability, deformity and pain(3).Single event-type accidents usually happen from the younger sports individual; for example, a sudden forceful lunge, a patella dislocation, or a significant instability episode into the knee that may also injure the anterior or posterior cruciate ligament. It has been demonstrated that forces greater than 25 newtons per square millimetre are enough to damage the articular cartilage as a one-off event (21). In such events, the shear force across the joint using an added compressive and/or torsional component may shave off a segment of cartilage and generate a chondral or osteochondral defect or the joint compression may indent the cartilage to cause substantial chondral damage. Even if these severe events do not result in full thickness chondral defects, they can begin the cascade of cartilage degeneration that may then result in a full thickness loss in cartilage over time.
The chronic repetitive-type lesions normally occur in older athletes and the elderly population. With repetitive loading the cartilage undergoes Several mechanical and histological modifications (3,12):
a. Loss of proteoglycans and cartilage swelling;
b. Increase in diameter of chondral collagen fibres;
d. Progressive chondral thinning.
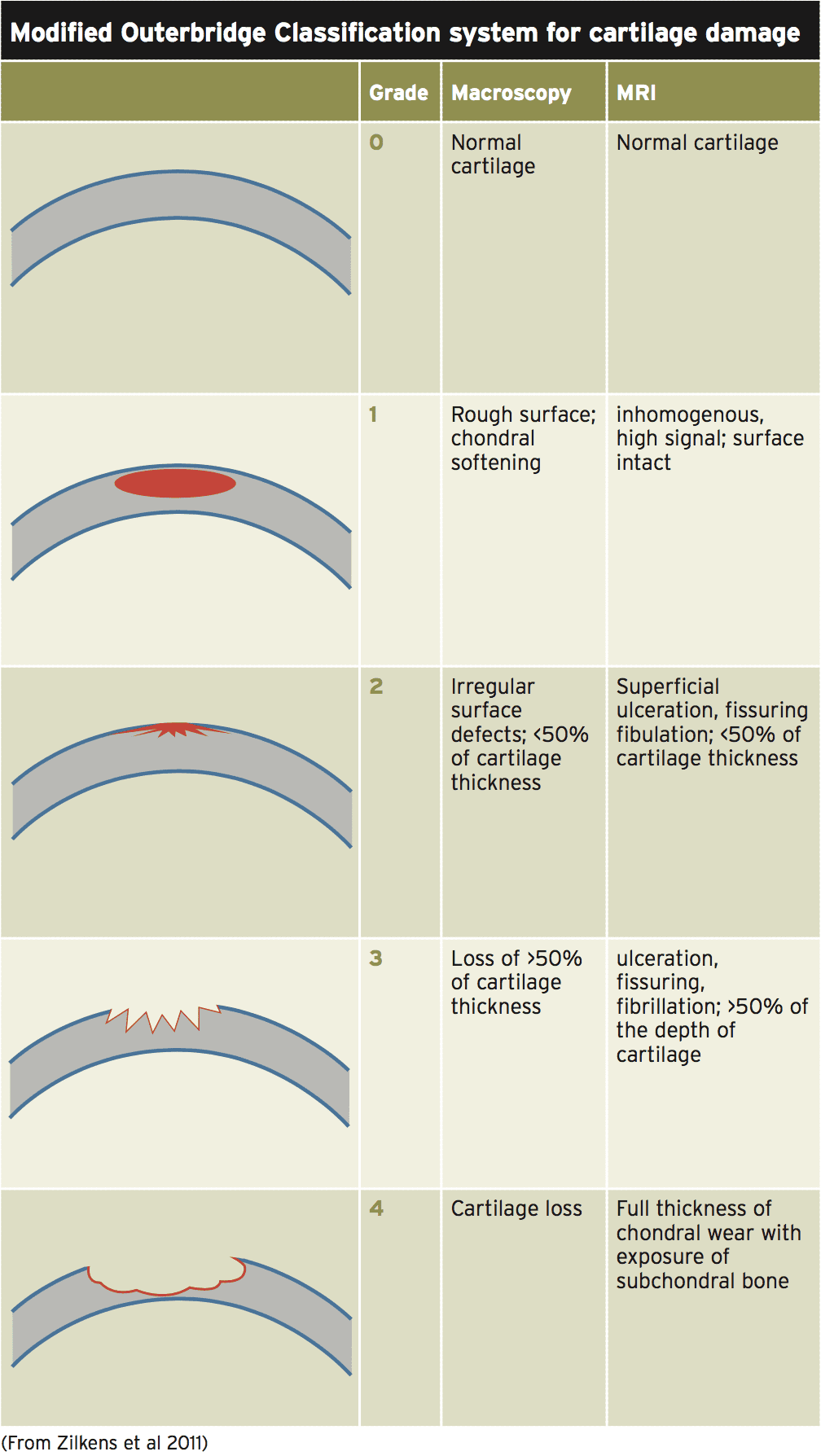
The progressive cascade of events in chondral injury generally include (Outerbridge classification(18):
1. Grade 1. Early softening and swelling of the articular cartilage;
2. Grade 2. Fissures and cracks in the surface of the cartilage;
3. Grade 3. Acute fissures and cracks Greater than 0.5inch;
4. Grade 4. bone. 4. Exposure of the subchondral bone.
Table 1 above shows how the Outerbridge classification relates to expected MRI findings in the cartilage(26).
Signs & Symptoms
Typically harms to the articular cartilage will introduce as pain and functional limitation within the knee. Movements that load the knee into flexion such as jogging, climbing stairs, lunging and loaded knee flexion for example squatting will probably be pain-limited. Many times a knee joint effusion will probably be present, and due to gross knee joint effusions complete knee extension might be restricted.The athlete may remember a certain knee loading movement that has created the articular cartilage injury such as a loaded twisting movement on a flexed knee ; or more commonly the pain can start insidiously after repetitive knee flexion loading movements. The knee might have problems with episodes of grabbing, providing way and bending in the presence of more significant cartilage injuries.
The sports medicine practitioner will be alerted to a possible chondral lesion from the Athlete because the continuing knee joint effusion, Possible locking and catching sensations And the operational limitations like pain Will encourage the sport medicine Practitioner to seek out some imaging modalities. MRI has the best ability to visualize the chondral defects minus the Need to direct arthroscopic assessment(4). Exact MRI findings to anticipate in chondral Lesions, refer to Chang et al (2011)(4).
Management
Sometimes some patients with full thickness cartilage defects may be functionally unaffected in the early phases after this injury; however, over time these may turn out to be quite debilitating and will cause slow and progressive loss of knee function(10).A range of interventions are suggested that may aid cartilage recovery with no need for major surgery and long-term treatment. Platelet-rich plasma (PRP) injections have been suggested as a way to stimulate cartilage recovery(22). PRP is also thought to have an anti-inflammatory action on the connective tissues, promoting early advancement in function of their joint . PRP is believed to exert its influence via direct stimulation of chondrocytes and mesenchymal stem cells of the subchondral bone and, especially in the early phases, through an immediate anti-inflammatory action in the synovial membrane. However, research to the long-term advantages of PRP as a standalone therapy for chondral defects haven’t been well conducted and in the meantime it seems that PRP may be used as an adjunct to boosting a healing environment to get a chondral defect after a surgical intervention.
Surgery For Chondral Defects
The types of operation available for full thickness chondral defects include:1. Abrasion;
2. Drilling;
3. Osteochondral autografts transfer;
4. Osteochondral allografts;
5. Repair with artificial resorbable scaffolds;
6. Autologous chondrocyte cell implantation (ACI);
7. Matrix assisted autologous chondrocyte cell implantation (MACI processes);
8. Microfracture technique for chondral resurfacing;
9. Mechanical fixation of osteochondral fractures.
The microfracture procedure was initially suggested by Steadman in 1980. The microfracture process is one stage arthroscopic, minimally invasive procedure that’s based on the principle that stimulating the bone marrow via micropenetration of the subchondral bone contributes to subsequent recruitment of platelets, expansion factors and mesenchymal stem cells to stimulate chondral repair(23,24,25). The resultant ‘bleeding’ into the chondral defect contributes to an accumulation of fibrocartilage that ‘fills’ the defect or gap in the cartilage. This can be encouraged by Rand (1985)(20) that make the point a supply of cells along with a matrix, an intact subchondral bone surface and some mechanical stimulation are required in order for healing of articular cartilage to occur.
In this procedure, each of the damaged cartilage is removed so as to acquire steady lesion margins, surrounded by healthy cartilage, and perfectly vertical borders. This is necessary so as to permit the clots to adhere in a secure manner to the base of the lesion and also to decrease the direct load on the lesion, thereby allowing a better fix. It’s important that the subchondral bone is not influenced during the debridement of the cartilage borders. Small ‘microfractures’ in the subchondral bone are all made with an awl at 45°. Achievement of the right thickness is confirmed by arthroscopic visualization of fat droplets in the joint following drilling (13).
However, not all of ‘microfracture’ procedures are fully profitable. Having a ‘microfracture’ procedure the lesion is fixed with fibrocartilage and this kind if cartilage has a reduced capacity to absorb mechanical load. As fibrocartilage comprises more collagen and less proteoglycans than normal intra-articular hyaline cartilage, and a much greater concentration of type I contrasted with type II collagen, it is more prone to potential wear and tear damage(2). Furthermore, while hyaline cartilage is normally subjected to load in compression, fibrocartilage is usually subjected to load in pressure, which means that the latter isn’t biomechanically suited to serve as articular cartilage. Actually, repeated mechanical stresses can eventually lead to collapse of a fibrocartilage repair.
In general, microfracture processes appear to reveal significant functional improvement in chondral defect effected knees(2,17,23,24,25). The vast majority of the improvement happens in the first year, however it generally takes two to three years to see maximum improvement in knee function. Ongoing complaints of symptoms will be common in the initial year. Studies have shown that it’s generally quite effective on lesions that are smaller than 400mm(2) and in patients below the age of 40(11,14,15,16).
It is still the surgical therapy of choice in athletic knees to the following reasons:
1. Most competitive athletes are under the age of 40 and ‘microfracture’ suits this age group the best;
2. It’s minimally invasive as the operation is performed only once;
3. The return to competition is much quicker than the more physiologically time-dependent processes like MACI (these need a two-year rehabilitation period);
4. Athletes are back in functional rehabilitation about eight weeks post- surgical negating the detrimental psychological effects of long-term rehabilitation in athletes.
Conclusion
The purpose of this was to discuss the appropriate physiology of articular cartilage, how it could be hurt in the athlete and what will be the presenting symptoms and signs. A discussion on the potential management approaches were discussed with specific emphasis on ‘microfracture’ procedures as initially described by Steadman at 1980. These processes are usually the first option for surgeons on athletes since they’re minimally invasive compared to other chondral repair processes and have normally the fastest recovery times with great results in athletes with smaller lesions. Part two of the piece will explain in detail the post-surgical rehabilitation required following a microfracture procedure.References
1. Am J Sports Med; 2004. 32:211–5.
2. Orthopedics. 1998. 21: 761-768.
3. Iowa Orthopaedic Journal. 1992. 12; pp 50-57.
4. Magn Reson Imaging Clin N Am; 2011. 19(2): 323–337
5. Arthroscopy. 1997. 13:456–60.
6. Osteoarthr Cartil. 2008. 16:337–342
7. Med Sci Sports Exerc; 2010. 42(10):1795–1801
8. Eur J Radiol; 2006. 57:32-36.
9. Arthroscopy; 2002. 18:730–4.
10. Clin Sports Med. 2010. 29; 257-265.
11. Arthroscopy. 2006. 22(11):1180–6.
12. J Bone and Joint Surgery Am. 1982. 64; pp 460-465.
13. Joints. 2013. 1(4); 167-170.
14. Cartilage. 2010. 1(2):113–120
15. American Journal of Sports Medicine, 2005. vol. 33 (11), pp. 1639–1646.
16. Am J Sports Med. 2006. 34(9):1413–8
17. International Orthopaedics. 2012. 36; 43-50.
18. J Bone Joint Surg Br; 1961. 43:752–757
19. Clin Sports Med. 2005. 24(1):1-12.
20. Comtemp Orthop. 1985. 11; pp 13-30.
21. J Bone Joint Surg; 1977. 59-A(8):1068- 1075.
22. Arthroscopy; 2013. 29:1399-1409.
23. J Knee Surg; 1980. 15:170-176.
24. The Journal of Arthroscopic and Related Surgery. 2003. 19(5): pp 477-484
25. The Journal of Knee Surgery. 2003. 16(2), pp. 83–86.
26. Orthopedic Reviews. 2011. 3(e9); pp 34-41.