El Paso, TX’s chiropractic scientist Dr. Alexander Jimenez investigates the anatomy, possible causative factors and the pathophysiological basis of intersection syndrome.
Intersection syndrome is an overuse injury of the dorsal aspect of the forearm. It occurs in sports which demand repeated wrist flexion and extension, ie rowing, sailing, racquet sports and weight lifting. It’s described as a non-infectious inflammatory process at the intersection of the second and first dorsal extensor compartment(4). It has been suggested that during recurrent wrist flexion/extension friction may grow between both of these pockets in their crossover point, causing intersection syndrome (2).
Anatomy
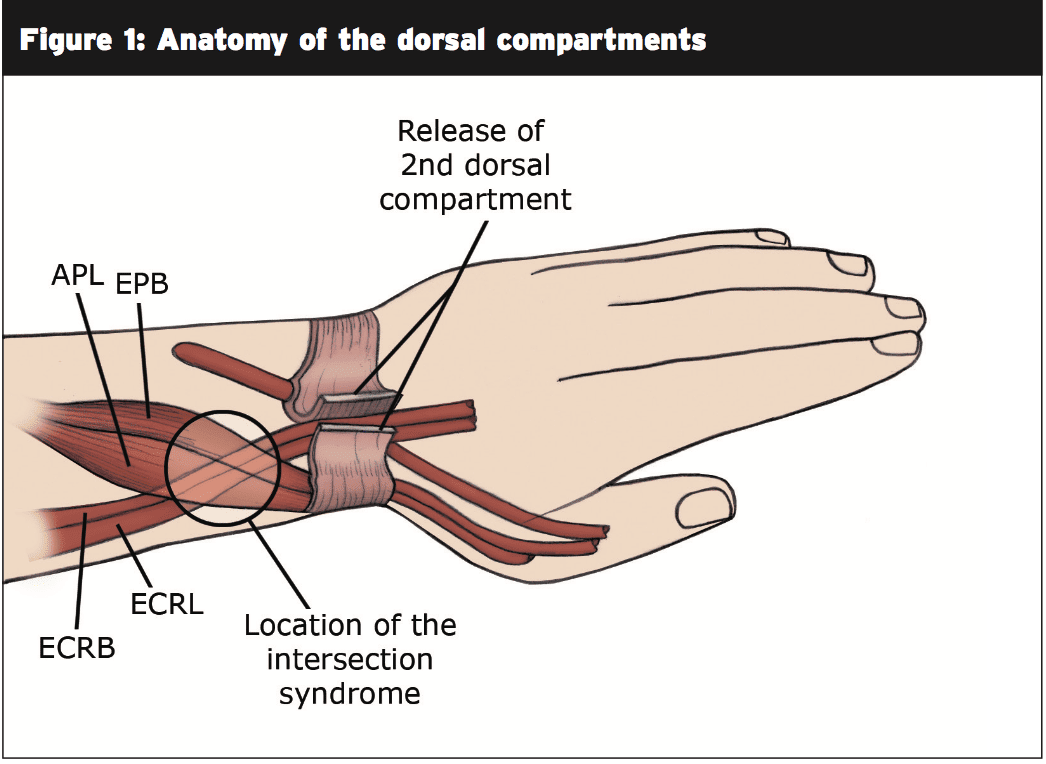
The first dorsal compartment consists of the muscle bellies of the Abductor Policis Longus (APL) and Extensor Policis Brevis (EPB) whilst the second dorsal compartment comprises the joints of Extensor Carpi Radialis Brevis (ECRB) and Extensor Carpi Radialis Longus (ECRL)(6).) The muscles of the initial dorsal extensor compartment (APL and EPB) originate deep at the side of the forearm and since they course distally they become shallow and crossover the second dorsal compartment (comprising of ECRL and ECRB). Intersection syndrome occurs in the ‘crossover’ point of the first and second dorsal pockets.This crossover point is located between 3.5 and 5cm proximal to Lister’s tubercle(5) (see Figure 1).
 Each dorsal compartment of the wrist tends to get its sheath nonetheless, communication between the second, third and fourth compartments does occur (two). Additionally occasionally each tendon from the second dorsal compartment is contained within its sheath(two). In Draghi’s ultrasound study they found that this occurred in 5 of the 21 forearms studied (23.8 percent). They noted that despite these anatomical variations, tenosynovitis of the extensor carpiradialis brevis (ECRB) has been observed in all forearms studied with intersection syndrome (2).
Each dorsal compartment of the wrist tends to get its sheath nonetheless, communication between the second, third and fourth compartments does occur (two). Additionally occasionally each tendon from the second dorsal compartment is contained within its sheath(two). In Draghi’s ultrasound study they found that this occurred in 5 of the 21 forearms studied (23.8 percent). They noted that despite these anatomical variations, tenosynovitis of the extensor carpiradialis brevis (ECRB) has been observed in all forearms studied with intersection syndrome (2).Pathophysiology
Even though the exact cause is unknown historically, the most common concept for its pathophysiological basis of intersection syndrome is that repeated wrist flexion/extension leads to friction between the joints of their first and second compartment leading to tenosynovitis and/or stenosis(3).Several common standards on US are reported that include:
- peritendinous oedema
- Fluid-filled tendon sheaths of intersection in the point
- Interruption of the hyperechoic plane that separates these two compartments
- Tendon thickening and signals of tendinosis(6).
Additional research has to be conducted but the thicker tendon seen on ultrasound in intersection syndrome might be a result of the same cell-driven reaction as seen in tendons of the thoracic in which a unaccustomed load causes an increase in proteoglycans that are hydrophilic (attract water) causing a milder tendon.
Patients may also present with tenosynovitis of the third extensor compartment (which includes extensor pollicus longus — EPL) as well as the next compartment. This could be because of either tenosynovitis of the EPL or due to communication between the second and third compartments(two). The first compartment and any other compartment of the wrist does not communicate. Interestingly, peritendinous oedema isn’t necessarily restricted to the crossover website(4). Lee et al discovered the peritendinous oedema occurred over an area up to 12cm long and could be found to extend distally past the radiocarpal joint that. This implies that these extensor compartments are not bound by the extensor retinaculum(4).
Considering these findings intersection syndrome could be considered as having two different kinds of pathology:
1. Tenosynovitis (swelling of the fluid-filled sheath surrounding the tendon) probably because of friction;
2. Tendinopathy (thickened limb) — cell-driven response to spike in workload.
Clinical Presentation
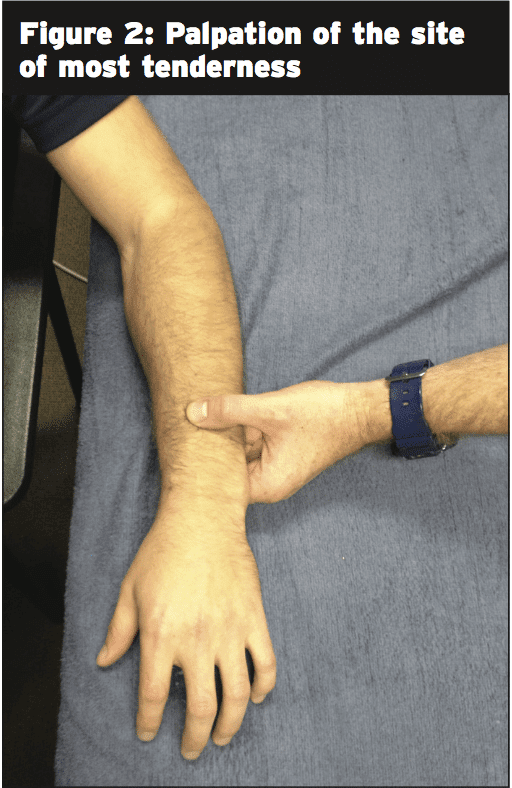
Athletes with intersection syndrome complain of pain, erythema, swelling, tenderness to palpation and sometimes crepitus(4). Symptoms can present over a period of many weeks but it can also occur as an acute onset(4).Common causative factors of intersection syndrome include:
- Spike this would include any changes in intensity, quantity or frequency which could overload the joints;
- Muscle Weakness — due to rest interval can lead to increase load of these muscles of the wrist;
- Equipment — in rowing a change in handle could be enough to increase the load on the forearm joints if this is done via a training phase that is high;
- Technique errors — changes or errors may also increase load on these tendons.
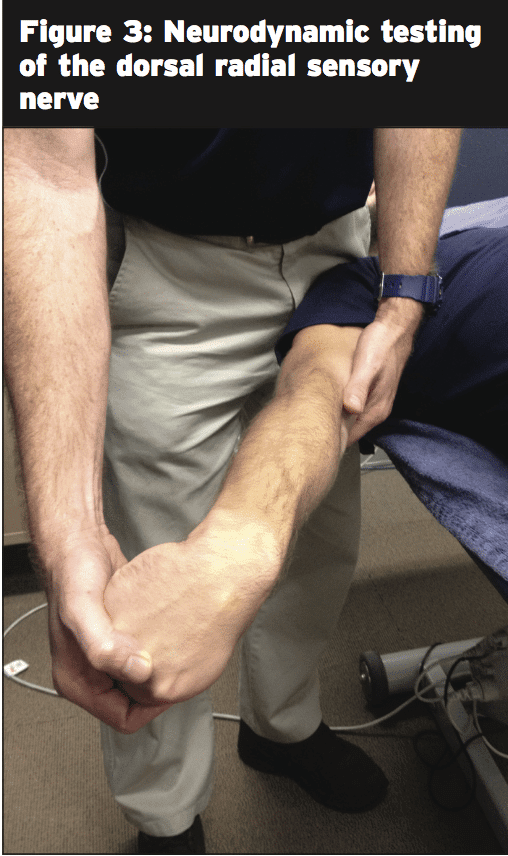
To exclude Wartenburg’s syndrome (entrapment of the dorsal radial sensory nerve) neurodynamic testing should be accomplished with the fist clenched, flexed thumb and ulna deviated wrist(7) (see Figure 3). When neural tissue is included (as in the event of Wartenburg’s syndrome) tension is described on the radial side of the distal forearm. This sense of tension is diminished when the shoulder is raised.
Management
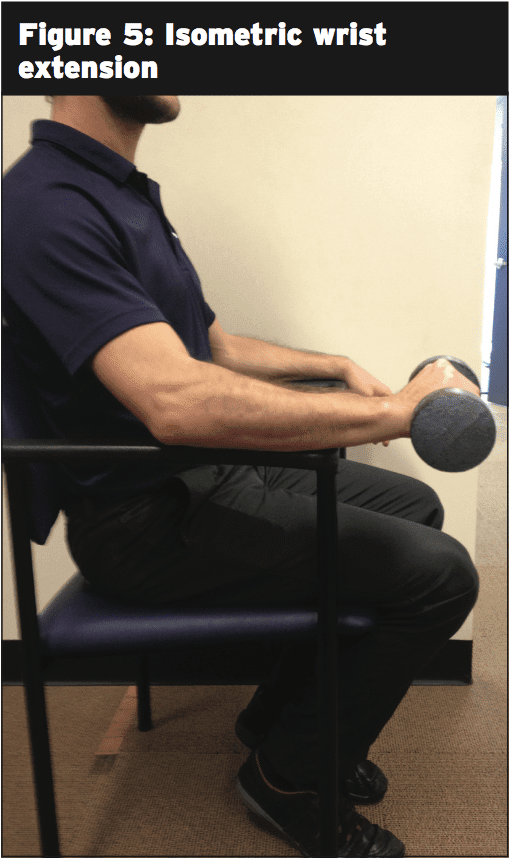
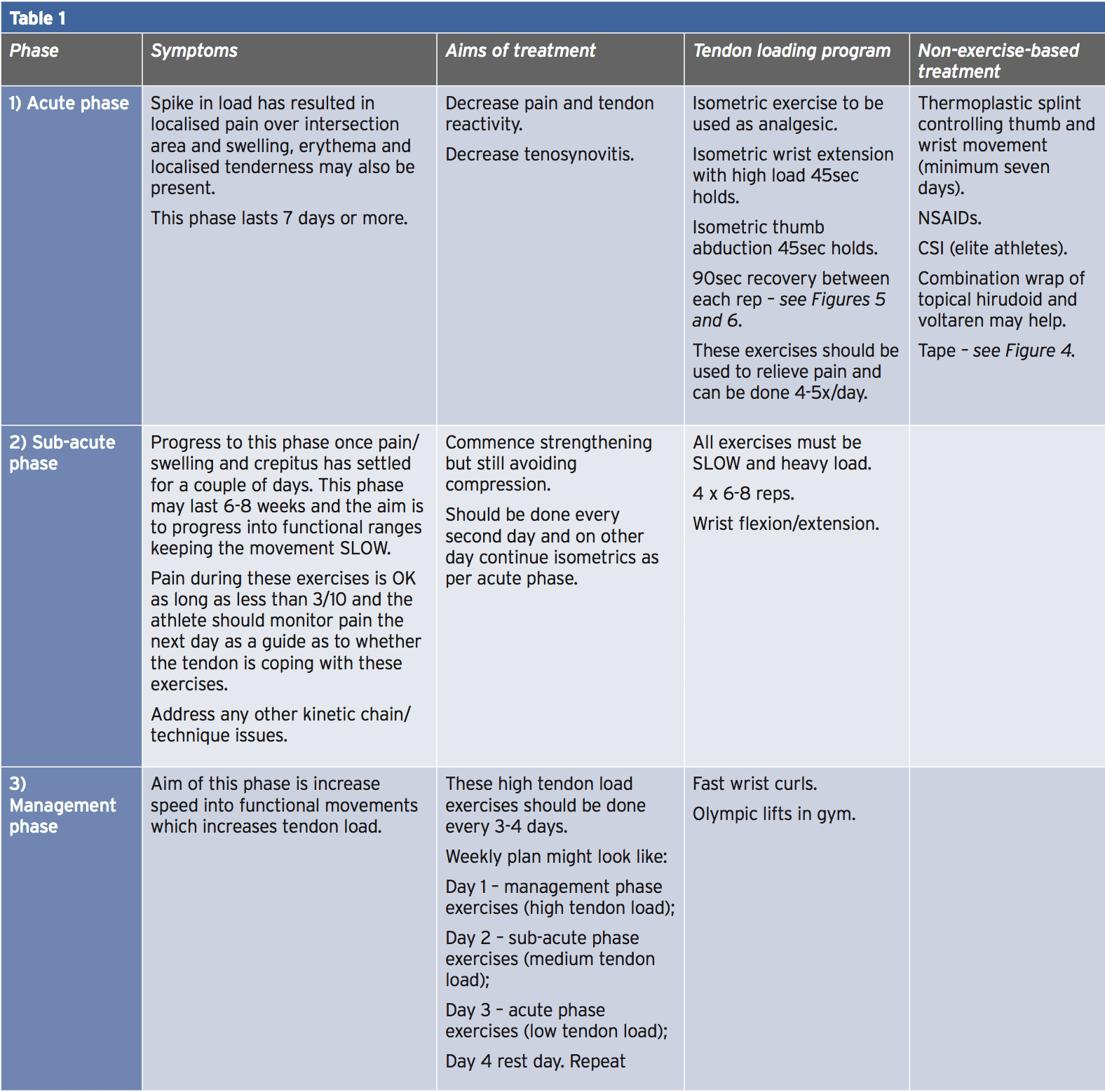
For a successful result early intervention is required. Treatment should be directed in settling the part whilst keeping in mind a element may be present. Traditionally management of intersection syndrome has included a combination of relaxation, NSAIDs and splinting and employing this method 60% of individuals have reported improvement within 2-3 months(3). Taping continues to be utilized as a very useful adjunct to treatment with Kaneko et al reporting a 100 percent improvement in five middle-aged females using ulna-directed tape of the dorsal forearm (see Figure 4). They reported progress in crepitus, swelling and tenderness in all five areas(3). CSI shot has also been used with great effect in recalcitrant cases or in the phases.Within an athletic people a strength-based approach in healing tendinopathies of the limb, utilizing the very same principles as would be worthwhile contemplating to initially help to acquire tendon strength then to keep constant tendon load during camp, tournament or a training block.
As with reduced limb tendon injuries, a program ought to be broken into phases.
These phases could be described as:
1. Acute phase;
2. Sub-acute phase;
3. Maintenance phase.
Table 1 summarizes a rehabilitation principle for an athlete having an intersection syndrome.
As with tendinopathies it is crucial to maintain loading that is consistent after a rehabilitation program that is good has been undertaken and symptoms have resolved. The athlete with a history of intersection syndrome ought to be encouraged to continue to maintain load and prevent spikes in load.
Conclusion
Intersection syndrome is a pathology which has tendinopathy components and both tenosynovitis. As such for a successful treatment outcome rehabilitation programs must deal with these issues both. A rehab program should be divided into three stages to assist progressively load the tendon. Once symptoms resolve the program needs to be repeated to maintain efficacy and help avoid “spikes” in load which is commonly related to onset of symptoms.References
1. Chauhan A et al, (2014) Extensor Tendon Injuries in Athletes. Sports Medicine Arthroscopy and Review, Vol 22 No1 45-55
2. Draghi F and Bortolotto C, (2013) Intersection Syndrome: ultrasound imaging. Skeletal Radiology, Vol 43, 283-287
3. Kaneko S and Takasaki H, (2011) Forearm pain, diagnosed as intersection syndrome, managed by taping: a case series. Journal of Orthopaedic and Sports Physical Therapy, Vol 21, No7 , 514 – 519
4. Lee R et al (2009) Extended MRI findings of intersection syndrome. Skeletal Radiology, Vol 38, 157-163
5. Lima J et al (2004) Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal Radiology, Vol 33 627-631
6. Montechiarello S et al (2010) The intersection syndrome: Ultrasound findings and their diagnostic value, Journal of
Ultrasound, Vol 13 70-73
7. Walker M (2004) Manual physical therapy examination and intervention of a patient with radial sided wrist pain: A case report. Journal of Orthopaedic and Sports Physical Therapy, Vol 34, No12 , 761-769