In part II, Chiropractor, Dr. Alexander Jimenez details what’s involved from the post-surgical rehabilitation of a hamstring avulsion.
Post-Surgical Rehabilitation
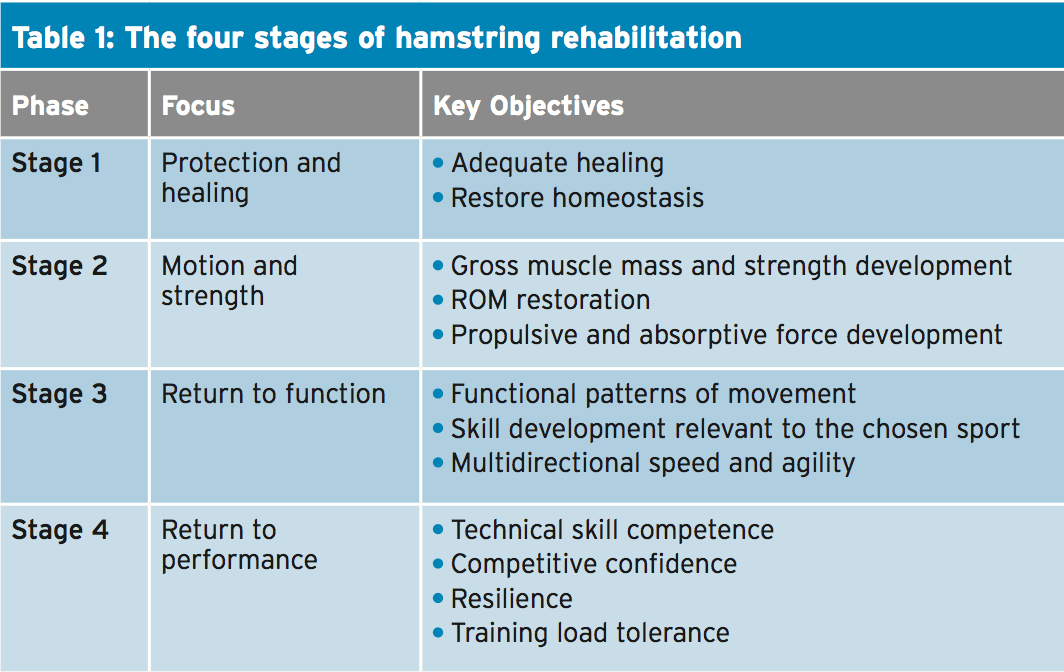
When planning and delivering the stages of the rehabilitation programs, an awareness of the effect of load exposure, load attenuation and induce generation is critical to provide us with a clear understanding of the landmarks which need to be attained and the pace at which they could pursued. The ideal way to approach the procedure will be to stage the approach to load resilience and performance employing a phased or landmark- based strategy with every stage feeding in the next. In keeping with the strategy, we don’t move in line with the passage of time, but the achievement of goals that are functional.Of hamstring surgery rehabilitation, the four stages are:
1. Stage One: healing and Protection
2. Stage Two: Restoring muscle strength and variety of movement
3. Stage Three: Integrated functional adaptation
4. Stage Four: Sports-specific retraining.
Protection & Healing
Post-surgery the patient will be kept touch weight bearing on crutches with short steps and may be kept in a hip-motion limiting brace to prevent hip flexion to avoid damaging the tendon. It has been suggested that the brace is fixed to then and 0-30 ° for the first 3 weeks 0-60 ° for the next 3 weeks. The brace is then removed and physiotherapy is started (1). However, not all surgeons feel that a hip motion limiting brace is necessary and if not used then the patient is instructed to avoid hip flexion past 45° (2). If the surgeon feels that knee extension should also be limited (in the case of repairs of failed conservative management whereby surgery has been delayed) then the knee might be fixed in a knee brace up to 60-90° to prevent extension and the brace is gradually opened up over the six to twelve weeks.In this stage intervention is limited to managing muscle tone issues and open chain hip abduction/adduction exercises. It is expected that this stage will take 6-8 weeks.
Stage Two:
Restoring Muscle Strength & Range Of Movement
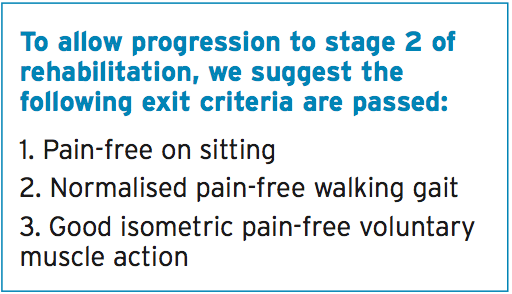
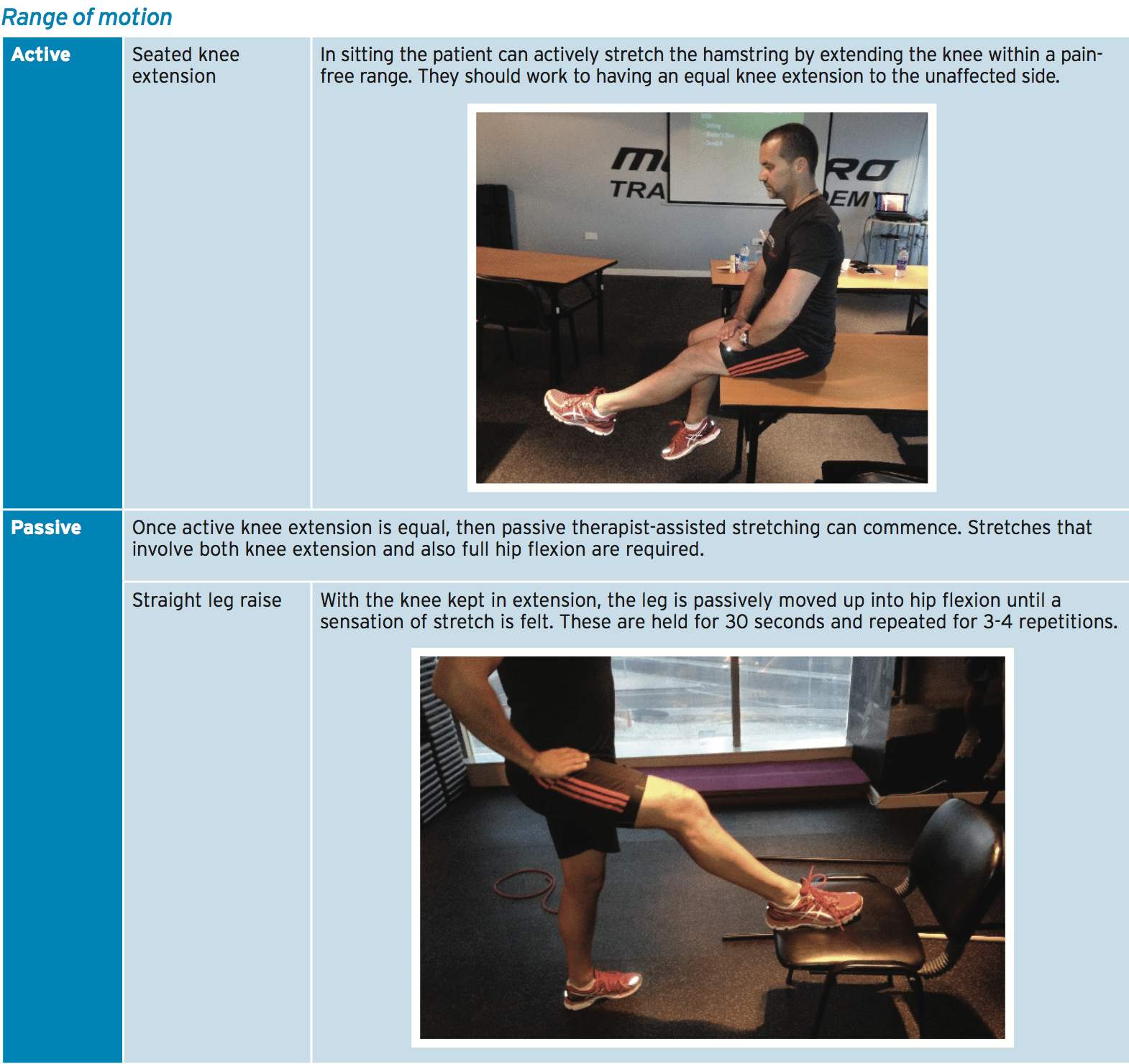
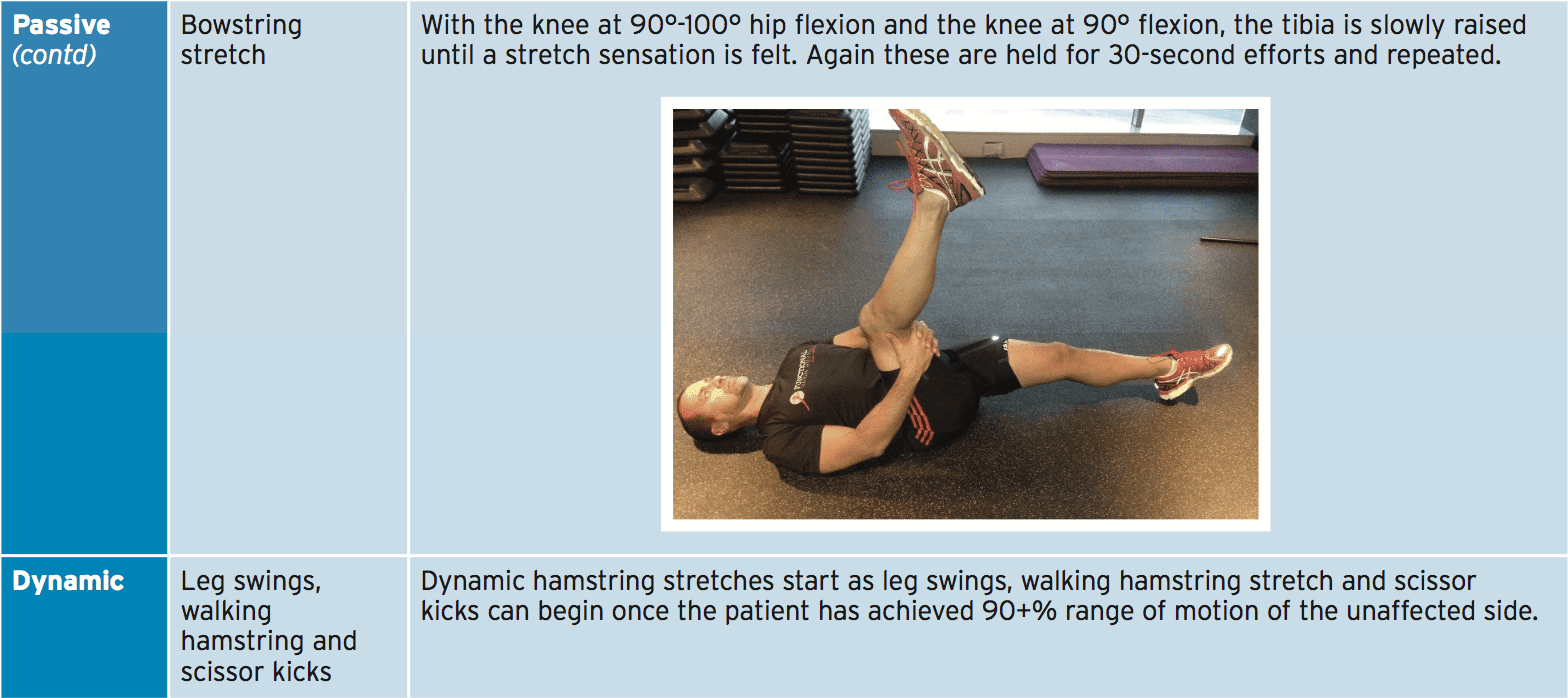
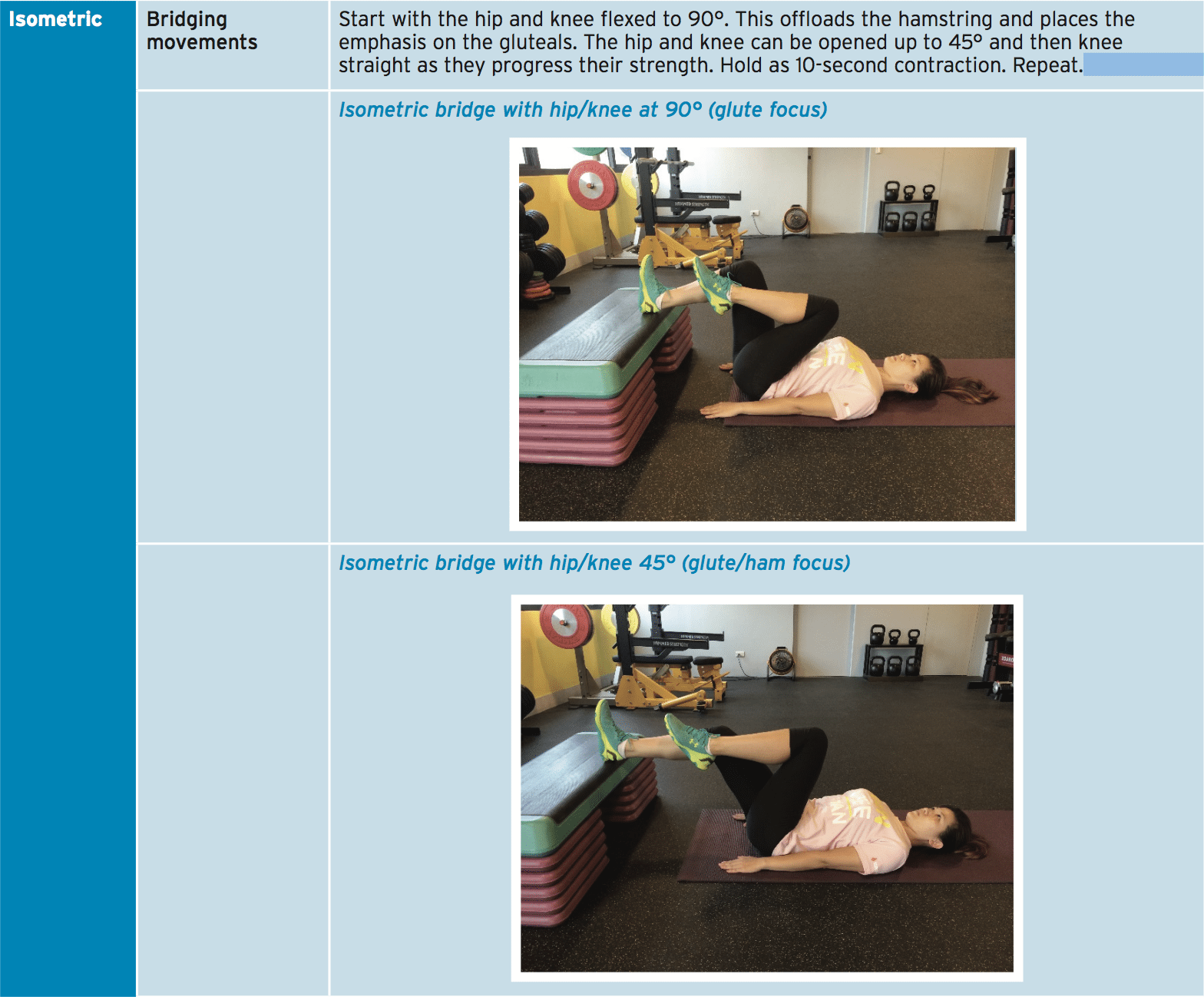
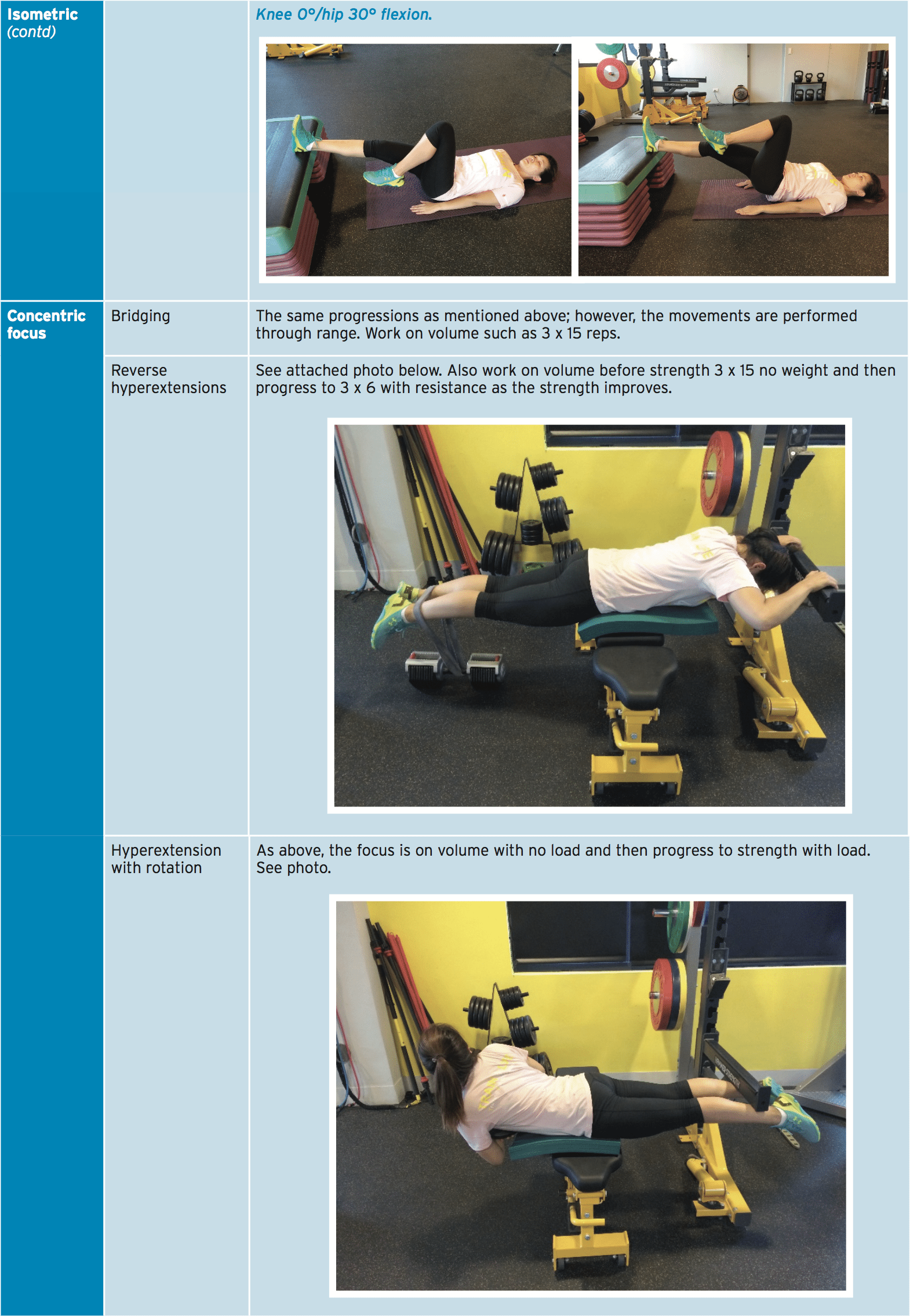
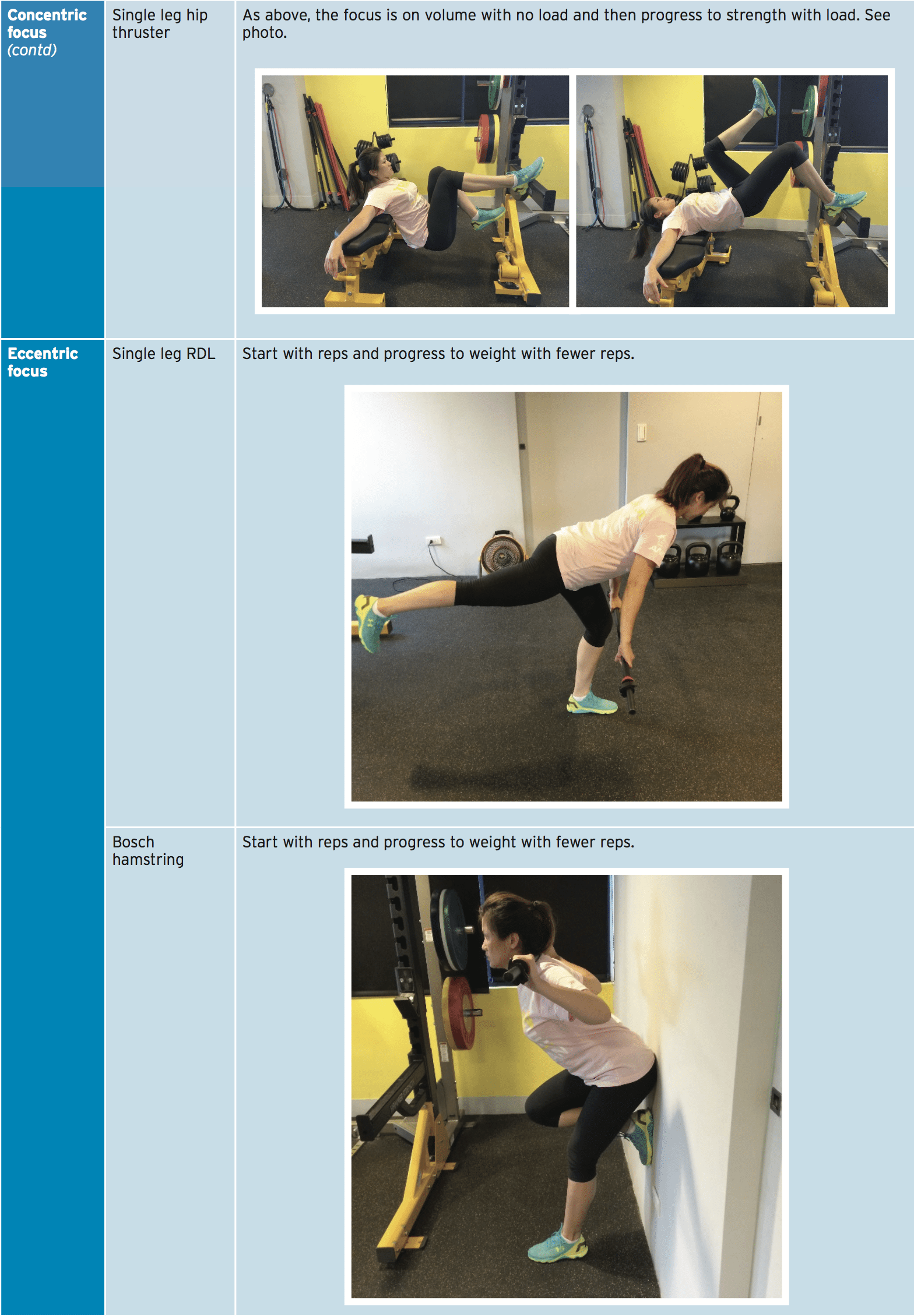
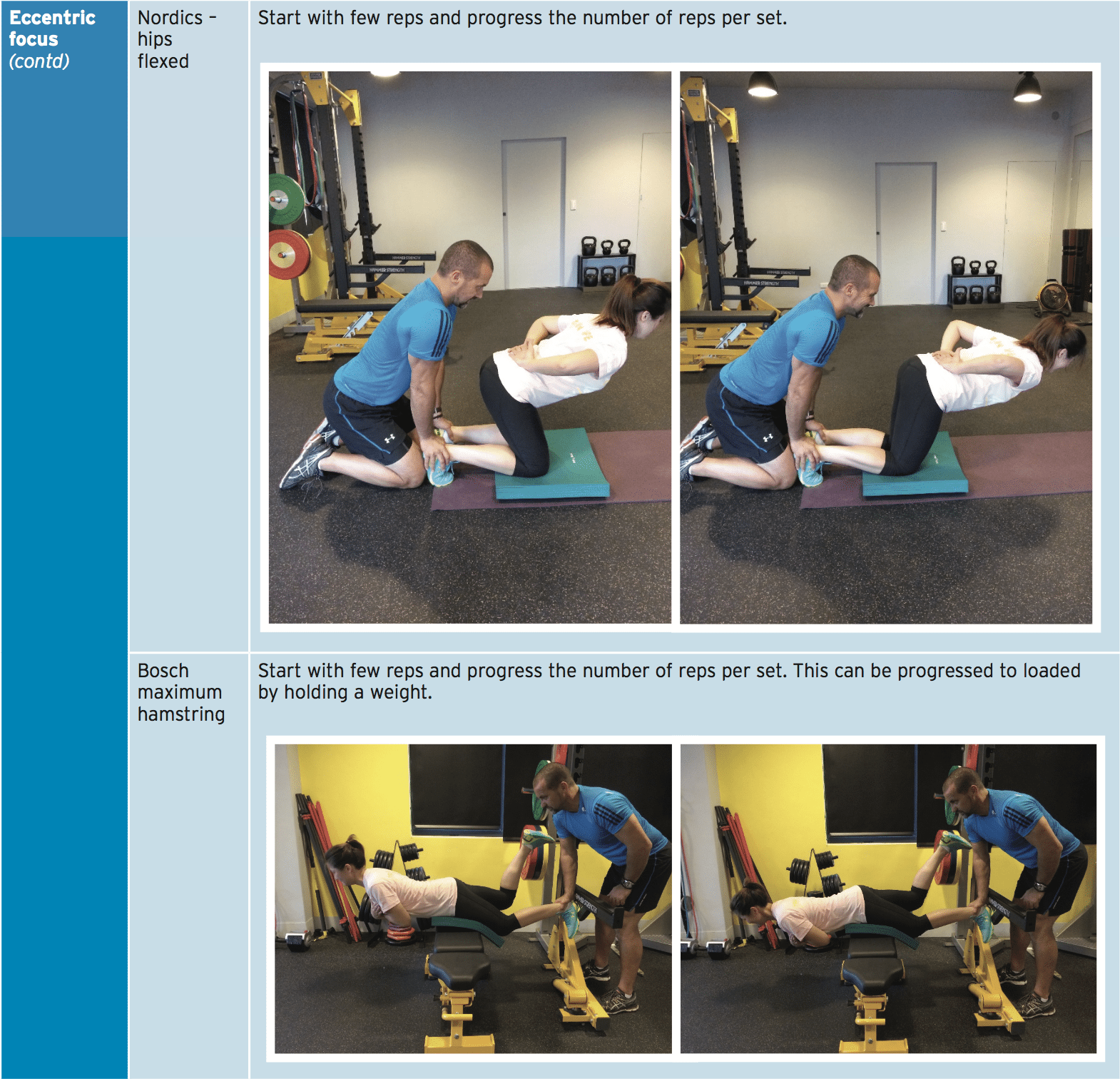
Once the patient is mobilizing full weight bearing and has progressed off the crutches and surgeon is happy that the patient has soft tissue healing to begin loading, more intensive physiotherapy commences to regain range of movement and to restore muscle strength. This will usually start at 6-8 weeks post-operative.As the soft tissue structures may still be vulnerable to high load or higher stretch positions, the recommendation is that the patient starts with active stretching in this stage and light load isometric contractions. The contraction type can be progressed to then and concentric eccentric as the hamstring adapts to the loads.
Physiotherapy Interventions
1. Active soft tissue treatment. Direct tissue massage, dry needling, friction therapy all can start to acquire in the hamstring. Soft tissue work will should directed towards other soft tissues such as deep hip rotators, adductor magnus, gluteals and hip flexors like rectus femoris TFL and iliacus.2. Proprioception training.
3. Core stability.
4. Hip muscle activation work. No weight bearing exercises will also be needed in the hip muscles to guarantee a balance between hip rotators and hip adductors/abductors.
a. Hip extension. With the patient prone, and the knee kept flexed to 90 degrees (eliminates hamstrings), have the patient extend the hip and hold the gluteal contraction. This may be done in sets of holds and repeated until fatigue.
b. Hip abduction. Simple side lying chain hip abduction and clams exercises.
c. Hip adduction. Supine ball that is lying squeezes.
Strength Progressions
Recent research into the efficacy of hamstring repair on muscle strength has shown that even if the patient returns to full athletic function, a strength return of only 78% can be expected while the hamstring strength is objectively using isokinetic testing equipment (3). This is an important consideration to bear in mind as the patients self reported strength gain was felt to be closer to 91-92% improvement (3). Using isokinetic testing may not be as predicting return to 16, overly reliable. The use of isokinetic testing will be excluded from this rehabilitation protocol.At this stage the athlete may have started jogging with the emphasis on running mechanics such as Mach drills’ utilization such as marching ‘A’ drills, ‘ skipping ‘A’drills, triple extension exercises. However, the athlete won’t have ventured running at this stage.
Neuromobilisation
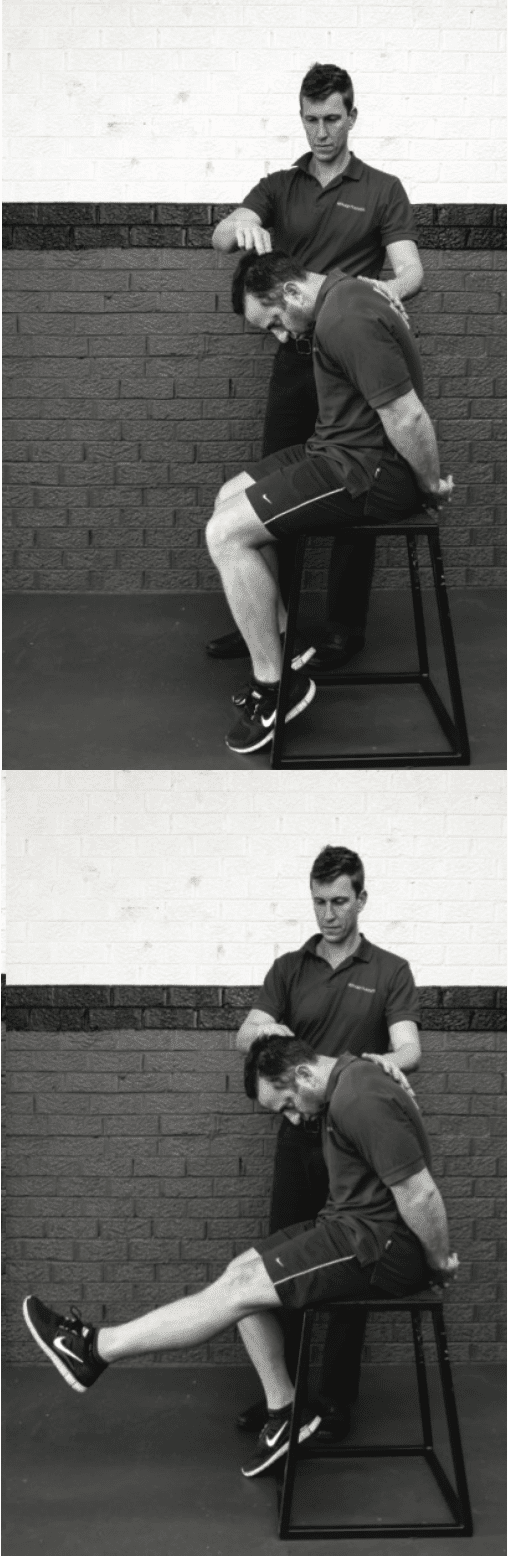
Due to the unique anatomy of the nerve and the upper hamstring, it is common for fibrosis and the scarring in and around the healing tendon to create adhesions around the nerve. This is termed ‘tension’. As the hamstring has to stretch, the athlete might affect and the bands that are fibrotic irritate the sciatic nerve. The perceived symptoms might be referred pain down the sensation and the hamstring they are ‘pulling’ the hamstring. This may be accompanied by signs such as numbness and paraesthesia.This may be readily managed clinically by starting some ‘nerve-stretching’ exercises or ‘nerve-flossing’ exercises. The most easy way to do that is using a recession position.
The diagram below shows a slump type therapy treatment.
1. Cervical extension back to flexion
2. Knee flexion back to extension
3. Ankle plantarflexion back to dorsiflexion.
These movements can be done as slow oscillations (repeated) or they can be held for a period of time (5-10 seconds) to gain a sustained stretch.
It’s necessary that these are done to the point of not pain and discomfort.
Stage Three:
Functional Adaptation
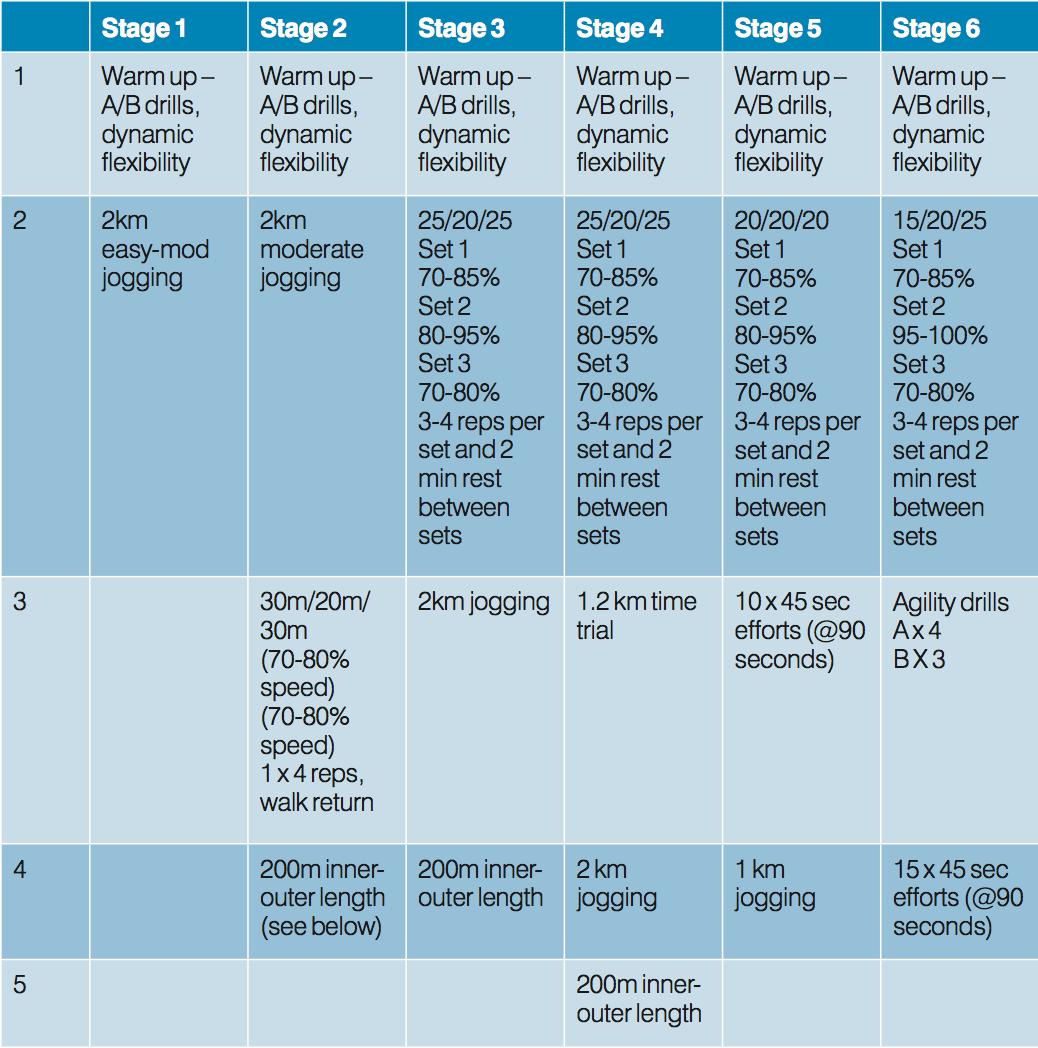
The return to running speeds highlights this phase. The patient may have started more easy low force running like jogging and running drills before this stage. Now the emphasis is on returning to high speed running. The athlete should be progressing through the strength stages.The athlete may perform 2-3 sessions of each stage (on alternate days) before progressing to the next stage. Thus the entire program that is running may take 12-18 sessions spread over a 4-5 week period. The strength work mentioned above should adhere to this running session (within 1-3 hours) and the next day ought to be a no-stress hamstring day. This should be left for recovery for soft tissue work and more easy cross training.
Notes on the table
1. Warm-up drills. These are well-used sprint drills known as ‘Mach drills’.
2. 25/20/25. This highlights the acceleration/hold speed/deceleration distance. Notice the acceleration and deceleration distance is shortened as the athlete progresses.
3. 1.2km time trial. This would most likely be a test an whole team has conducted in a pre-season so the rehabilitation coach knows the expected normal for this athlete. This can be done as a time trial or for team sports it is best done as a shuttle test. For example,
a. Run 20m and return.
B. return and Run 40m
C. Run 60m and return
D. Repeat
e. This equals 1.2km.
4. Inner/Outer Length
This area of the program’s purpose is to expose the hamstring to contraction types that are inner range, mid selection and outer selection.o-5m Bum flicks. Running drill with maximum knee flexion. Hit on the bum.
5-10m High knee skips
10-20m Jogging
20-30m A drills — heels under bum
30-40m Lunges
40-50m Jogging
Repeat and walk return for 4 sets.
5. Agility drills. In this example for a player:
a. A drill. 6-7 random cones set out over a 10 x 10m square. The athlete is instructed to run and touch the cone they are directed to at full speed. The cones are selected at random by the coach. Work and have 90 seconds recovery.b. B drill. As above the difference being that this time the athlete touches the cone, then jumps onto their front (push-up position) and then bounces up again to go to the next cone.
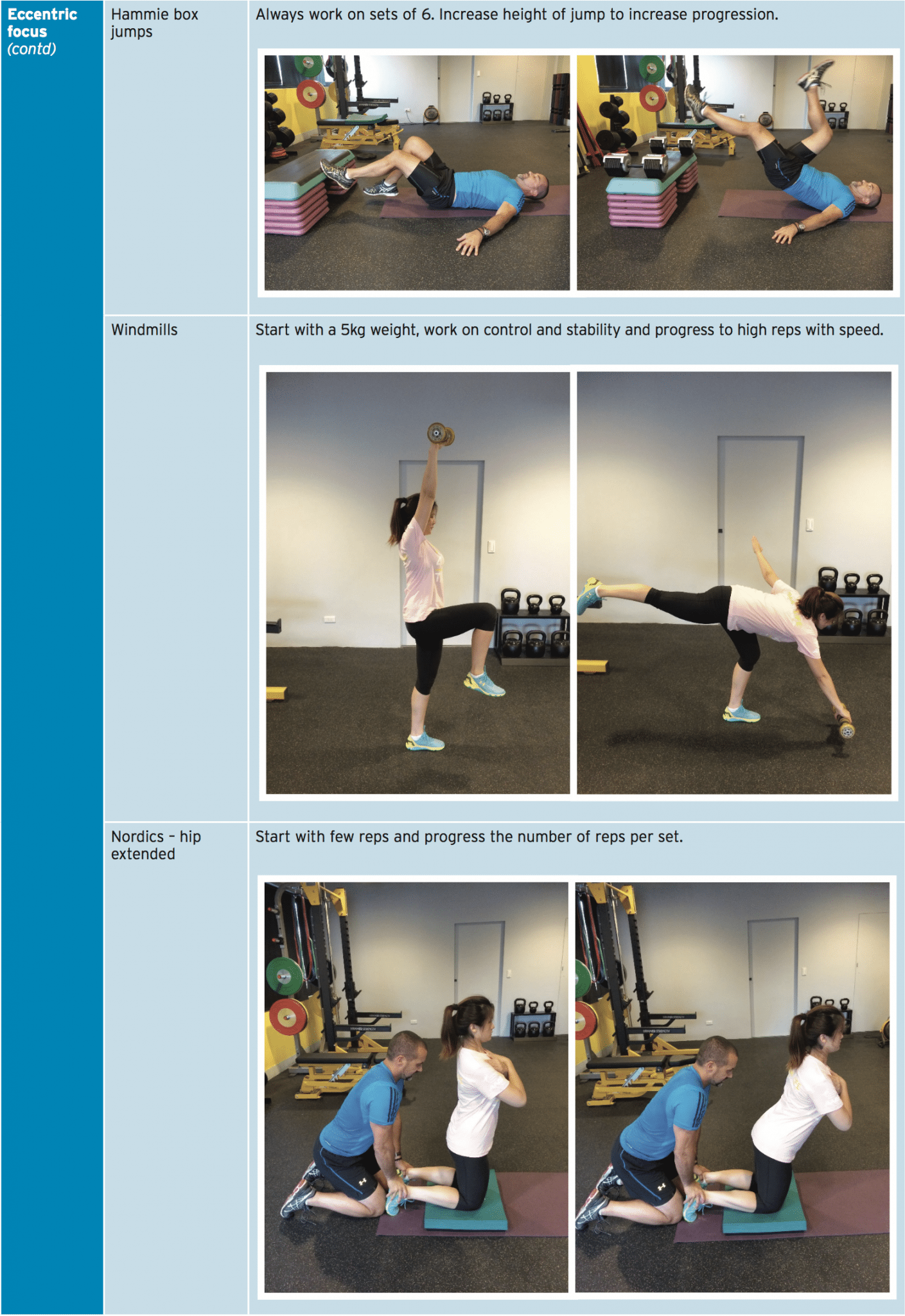
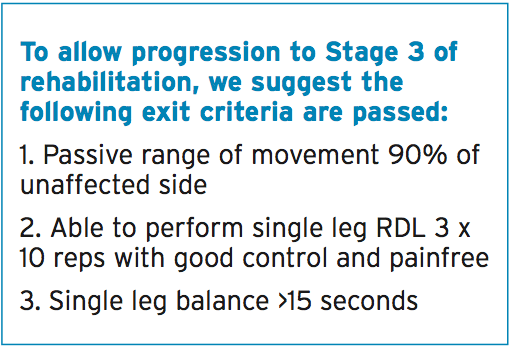
We suggest the following exit criteria are passed to allow progression to Stage 4 of rehabilitation:
1. Full speed running
2. Able to perform hip flexed Nordics 3 x 6 reps
3. No pain 48 hours post-running/weights
4. Able to change direction comfortably with no pain.
It’s expected that this stage will take surgery.
Stage Four:
Sports-Specific Retraining
Now that the athlete has returned to full- speed running, they may be integrated back into sport-specific and team-specific skill training. This phase is going to be characterized by the return to all skill elements done at competition intensity and speed. The athlete should have a part in this process as they are the ones that need to feel confident they can execute the skills. This phase may last 4-6 weeks before they are confident they can return to competition.Athletes in high speed running sports may take to feel confident to return to play; others in speed sports over distances may take six months post- .
We suggest the following exit criteria are passed to allow progression to return to competition:
1. Confidence in all skills
2. Perform a Bosch single leg hamstring (bodyweight) 3 x 6 reps.
It’s expected the athlete is going to be fit to resume competition post- surgery.
Conclusion
Hamstring avulsion injuries in athletes is a rare but debilitating condition that usually takes a surgical intervention. The return to competition period may take 6-9 months post- surgery and will involve high levels strength work and structured return and return to training programs.Most athletes who suffer a surgically can expect a hamstring when tested on isokinetic apparatus; nonetheless they might feel confident in returning to competition.
References
1. Domb, B.G., Linder, D., Sharp, K.G., Sadik, A., Gerhardt, M.B. Endoscopic repair of proximal hamstring avulsion.
Arthrosc Tech. 2013. 2(1); p. e35-e39.
2. Folsom, G.J., Larson, C.M. Surgical treatment of acute versus chronic complete proximal hamstring ruptures:
results of a new allograft technique for chronic reconstructions. Am Journal of Sports Med. 2008; 36(1): p.104-9.
3. Chahal, J., Bush-Joseph, C.A., Chow, A., Zelanzy, A., Mather, R.C., Lin, E.C., Gupta, D., Verma, N.N. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures. The Am Journal of
Sports Med. 2012. 40(10); p. 2325-2330.
4. Bosch, F. Klomp, R. Running. Biomechanics and Exercise Physiology Applied in Practice. 2004.