Foot injuries amongst athletes may originate from a number of sources. Chiropractor, Dr. Alexander Jimenez explores the common problems, what may cause them and how it is possible to stop yours by looking further ahead.
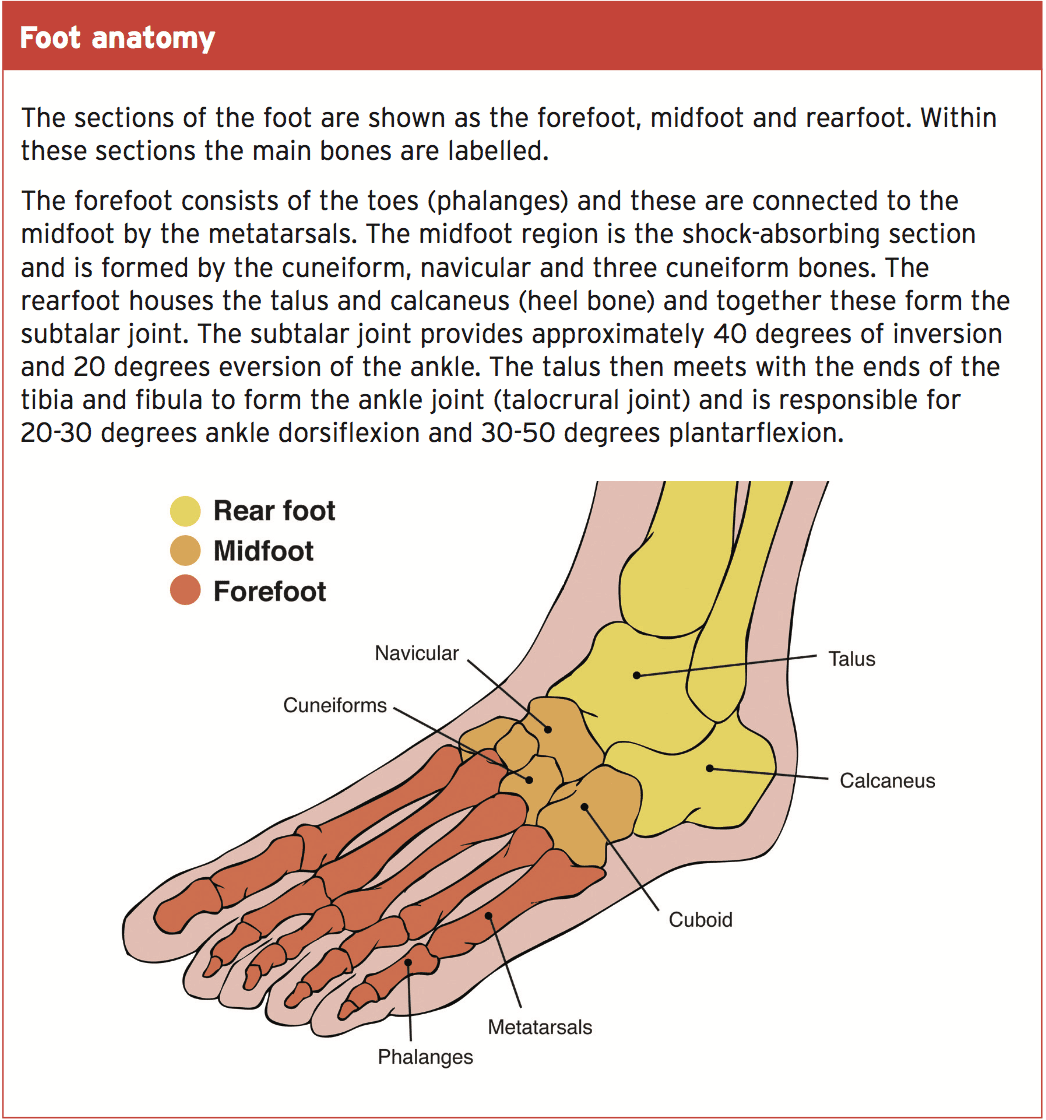
The foot is the most complicated region of this lower limb, and possibly the most intricate area within the body. It functions as a launching pad of the athlete; function as the first part to contact the floor, absorbing the ground’s forces (which could exceed more than four times the body fat running or up to 12 times with leaping and impact) and arming the athlete forwards, or in to any way they need(1). Thus it is not surprising that the foot can become overused and subject to many localized injuries. However, the difficulties can also originate from further up the kinetic chain (further up the leg) such as the pelvis/hips, knee and/or ankle. Injuries or bio-mechanical issues more proximally up the leg can have a later, indirect effect on the foot mechanics(2). Directly or indirectly, foot problems can consequently be a huge burden on the athlete. Here we present the topics to consider and how to address them.
Ankle sprains are damage to the ligaments, and are allegedly the most common trauma ankle/foot injury in athletes (4). Roughly 30 percent of foot sprains then go on to develop chronic ankle instability, giving a less stable base in the base of the leg to affect the ground. This then affects the whole lower limb because the alignment of the leg will be imbalanced and pressure the muscles and joints erroneously. Achilles tendonitis and plantar fasciitis are the two most frequent overuse injuries, resulting in inflammation of the Achilles tendon and plantar fascia (ligament over the sole of the foot) respectively (5, 6).
Stress fractures may happen to any of the all these are likely found at which the athlete is thicker weight bearing and will depend on how they hit the ground. Ultimately, tendon strains can happen to the anterior or posterior tibialis muscles, or into some of those tendons connected with the foot and ankle. These structures become impaired can be the end result of the athlete’s biomechanics. This is simply how they proceed; just how their foot strikes the floor and how all the muscles and joints respond to this further up the limb.
Biomechanics
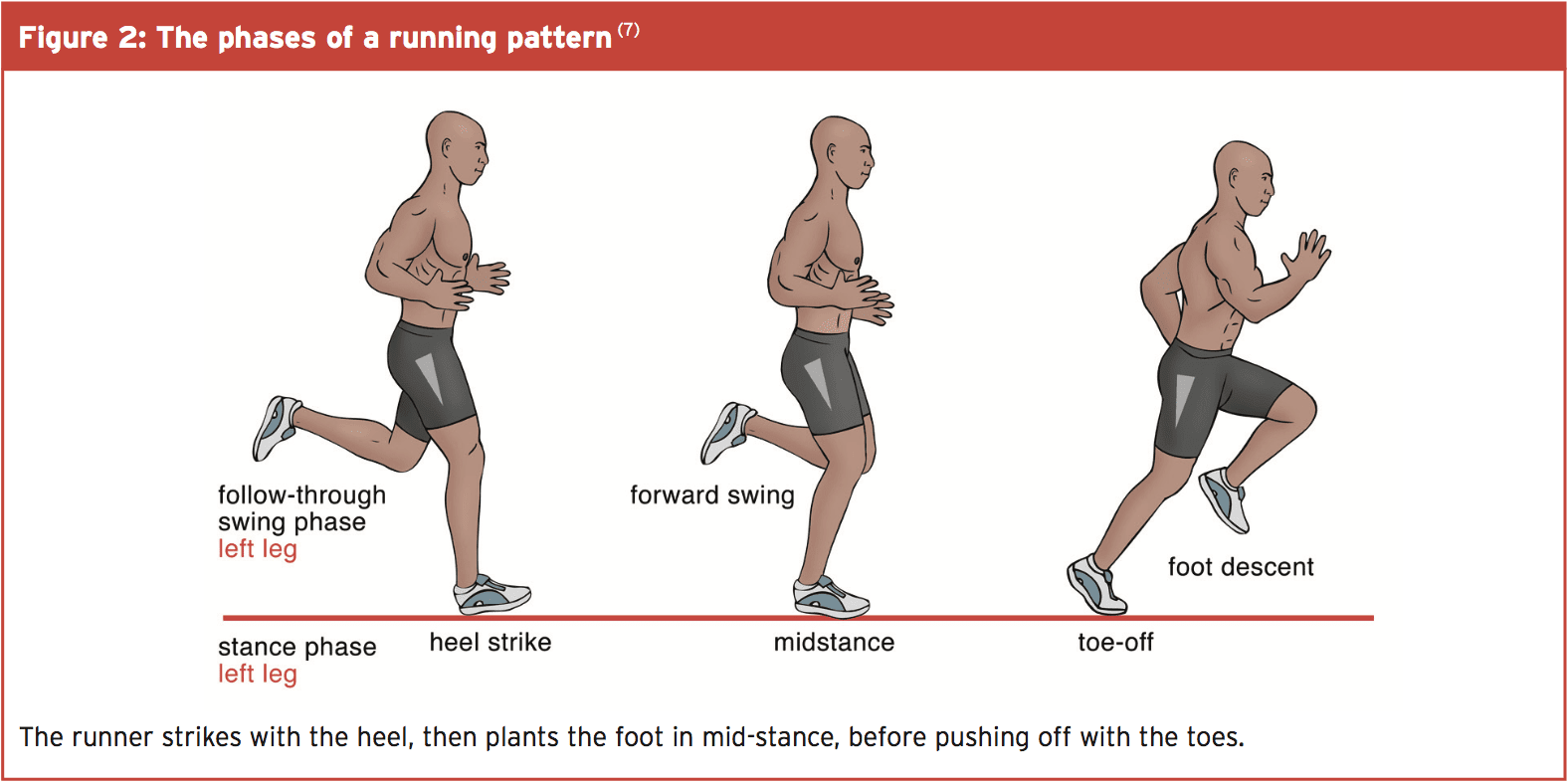
Running pattern is Hard to analyze for every sport and every person within this 1 discussion, as how the athlete sees the ground will depend on what they intend to do next. Distance runners will impact the floor usually with their heels first (see Figure 2); nonetheless, individuals who are sprinting or rapidly changing direction can utilize the forefoot initially. How the foot plants that the earth can have significant consequences afterwards.If the foot strikes in an surplus routine of Increased pronation or supination, studies have indicated that the athlete is subject to greater ground reaction forces and speed of loading; this really is actually the force returned in the floor, and the speed at which the load exerts throughout the foot(1). If the foot introduces more into pronation, there’s excessive internal rotation of the lower limb. This causes increased pressure into the lateral structures, such as the large toe and plantar fascia. The calf muscles and peroneal muscles then work harder to control the foot angle and also prevent additional rotation. This creates an imbalance of forces in the patella (knee cap) and can highlight the quadriceps and iliotibial band. Conversely, a more supinated foot strike has less freedom at the foot and ankle because they cannot roll in their natural movement pattern(two). Ankle sprains are somewhat more prevalent with supination and inversion, as this places the lateral ankle ligaments on full strain and stretch.
Problems Not To Miss
Along with the common local foot and ankle injuries mentioned earlier on, there are other sources of foot pain, not arising out of the foot, that should not be overlooked: ankle impingement, gluteal weakness, and core disturbance.1) Ankle impingement
Ankle impingement can happen anteriorly or posteriorly. Both types involve the pinching of structures which restrict the foot and ankle movements and can be severely disabling. Dance, sports and football are the most commonly reported affected sports(8). Ankle impingement may be the result of ankle instability. Lax ankle ligaments allows increased translation of their joints and small bones, allowing gliding of their bones and can impinge on the surrounding soft tissues and tendons(8). This debilitating condition can refer pain throughout the ankle and foot. This is a complex problem to diagnose and must be considered if additional harms are ruled out.2) Gluteal Weakness
Gluteal weakness is frequently because of an asymmetry at the pelvis. This may occur naturally as we burden endure more favorably through our leg and make it be stronger and more secure. In addition, the gluteals often are not attracted to full activation during everyday activities, as this necessitates proper squatting or deadlift motion, and therefore too little activation means they’ll gradually inhibit their work. Any harm that causes pain will also cause a pain inhibition influence on the gluteals. This is because of the powerful and propulsive function the gluteal muscles have, that in the event that you have injured any lower limb structure, your system inhibits the gluteals to slow you down. This will reduce the capacity of the athlete to push tougher(9). That is why regular gluteal training is essential to all athletes whether they are injured, or even.The core muscles are included within your maintain posture and keep the body in correct alignment. This ensures the forces are distributed correctly throughout the Body and that one limb, joint or construction Is not overloaded. The heart muscles Change position they transfer the weight as required, and bridge the distance, and load Between the top and lower limbs (10).
Heal From Above
Once the local injury has been treated right, the therapist must then explore the further intrinsic factors which might have contributed to the problem. These are the problems within the body including muscle fatigue and imbalances core stability. Balance is also a huge factor, incorporating all muscles and heart work.1) Gluteal Strengthening
These should be performed for the weak side initially to make up the discrepancy, and completed on both sides for bilateral stability and balance. Up to 3 sets of 10; however, it is more about quality of the movement and control than numerous repetitions.2) Core Stability & Balance
These should be performed for the side initially to compose the discrepancy, and thereafter finished on both sides for bilateral equilibrium and balance. In accordance with 3 sets of 10 can be educated; however, it is more about quality of their motion and control than many repetitions.These should be carried out on either side to encircle the whole core region. These exercises are all done on a mat, on the stable floor surface. Whilst that does provide an additional challenge to the athlete, a recent study showed that performing heart exercises on the unstable surfaces had no further benefit to physical fitness than the very same exercises performed over the secure ground(11). So whilst they might be more core intensive, they don’t transfer to higher fitness benefits and perhaps executing the workout with good technique is much more important here than attempting to attain the hardest version.
3) Single-Leg Balancing
Balance exercises on a leg are important to permit the whole kinetic chain to work together and coordinate, because the majority of the above exercises operate muscle groups in isolation. These may also be tailored to the athlete by mimicking positions they might encounter during play. Single-leg balancing additionally strengthens the intrinsic foot muscles (small muscles involving the foot bones) by simply inviting them to be the grip on the surface for stability.Treat Outside The Box
When the inherent factors have been addressed, the therapist should also think of the extrinsic influences.1) Footwear Selection
Footwear is a hugely personal taste, and will also come down to the sort of sport being played. When the foot attack pattern has been identified the correct footwear can be selected. People who over pronate will require a shoe with extra stability and control, and this usually consists of a medial arch support inside the shoe. Those people who have surplus supination will require a trainer that offers extra cushioning and padding to absorb more shock.Trainers gradually lose their support and shock absorption capacity and, for the amateur, after 250 miles they are going to have depleted roughly 30-50percent of their support. By 500 miles that the athlete should want to replace their coaches to maintain good support(12). For the serious athlete the mileages could be far less. Having two pairs to alternative will also accustom the foot into different supports and decrease the wearing from one coach. More common change than this is not recommended, but because fresh footwear will probably be more rigid, and research has shown that this causes an gain in the plantar pressure; this really is the pressure the athlete puts through the foot when conducting and may place additional strain throughout the foot structures(12).
2) Altered Training Plans/Grounds
The surface where an athlete performs on can be attributed to injury, even though the evidence for this isn’t outstanding. Generally, harder, drier surfaces can lead to overuse injuries like stress fractures and tendinopathy, since there is less shock absorption and much more effect through the joints. Artificial grounds normally have a greater shoe-surface friction and therefore are associated with higher injury rates(13). If an athlete is afflicted by injury, return to sport should be guided through suitable surfaces/softer grounds initially before return to normal surfaces.Overview
- The foot is responsible for all weight bearing activities, absorbing the ground’s reaction forces, and propelling the athlete in movement.
- The position that the foot strikes the floor can affect injury, particularly if the foot is over-pronated or supinated;
- The equilibrium and alignment of the hips and knees can affect the angle that the foot is placed at, and affects the floor;
- Local foot placement and patterns should be assessed initially, followed by correction of abnormal foot attack, altered arches, knee posture and pelvic place.
- Strengthening exercises should work the gluteal muscles, core stability, alignment of the lower limb, and balance function;
- Other things to consider include the kind of coach or footwear, insoles, training grounds, and training plans.
1. Annals of Biolog Research. 2011; 2(6): 102-108.
2. Clin Sports Med. 2010; January 29(1), 157-167.
3. Clinical Sports Medicine (2009). 3rd Ed. Australia: McGraw-Hill Professional. pp. 646.
4. J Athl Train. 2007; 42(2):311-319.
5. Foot ankle Int. 2008;29(7):671-676.
6. Sports Med. 2006; 36(7):585-611.
7. Clinical Sports Medicine (2009). 3rd Ed. Australia: McGraw-Hill Professional. pp.48.
8. Foot and ankle surgery. 2015;21:1-10.
9. Br J Sports Med. 2014; 48: Suppl 2: A6-A7.
10. J of Sports Rehab. 2013; 22: 264-271.
11. BMC Sports Sci, Med and Rehabil. 2014; 6:40.
12. BMC Research Notes. 2011; 4:307.
13. Scand J Med Sci Sports. 2003; 13(5): 299-304.