Concussion in sport is a phenomenon but one with potentially long-term consequences of athletes. El Paso, TX’s scientific chiropractor Dr. Alexander Jimenez looks at the issue of equilibrium and neurocognitive deficits, and approaches to rehabilitation following a concussion.
Concussion is a syndrome characterized by change in brain function, such as alteration of mental status and level leading to mechanical pressure or trauma to the head. After such an effect, a number of symptoms can occur for weeks and months later, including disturbances in reflexes, judgment, memory, speech, balance and muscle coordination.
Studies indicate shows that concussion is a common occurrence in sport, to make matters worse. For instance, data in the US has estimated that as many as 3.8 million concussions occur during competitive sports and recreational activities annually, with as many as 50 per cent of occasions going unreported(1). Moreover sport is second only to motor vehicle crashes as the leading cause of concussion being football, hockey, rugby, basketball and soccer.
Research indicates that recovery from concussion is quite rapid. As an example, a 2012 study investigated the epidemiology of concussions in high school athletes by assessing the rates and patterns of concussion one of 20 sports(2). During the study interval, 1936 concussions were reported through 7,780,064 athlete exposures (AEs) to get an overall accident rate of 2.5 per 10,000 AEs. With many athletes returning to perform 1 to 3 months, concussion symptoms resolved in over 40 per cent of the athletes studied.
From time to time recovery is not straightforward. Research proves that the larger the number, severity and length of symptoms after a concussion, the more prolonged the period of healing is very likely to function as(1). In particular, younger athletes may require a lengthier recovery and seem to be more vulnerable to a concussion accompanied with a catastrophic injury(1). To complicate things further, pre-injury mood disorders, learning disorders, attention-deficit ailments (ADD/ADHD) and migraine headaches complicate both the first diagnosis of a concussion and also the process of determining when an athlete is prepared for return to play.
Return To Play After Concussion
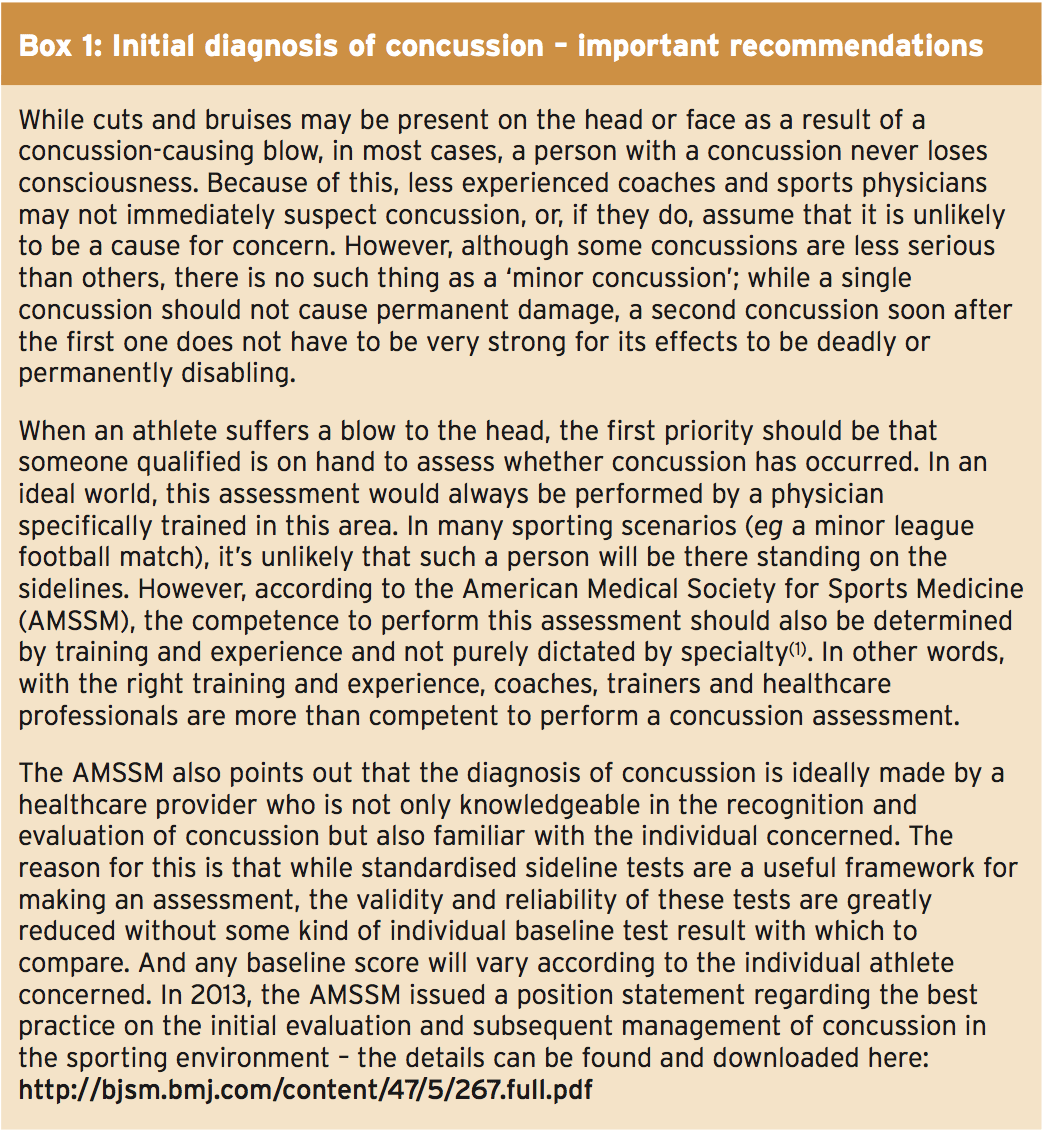
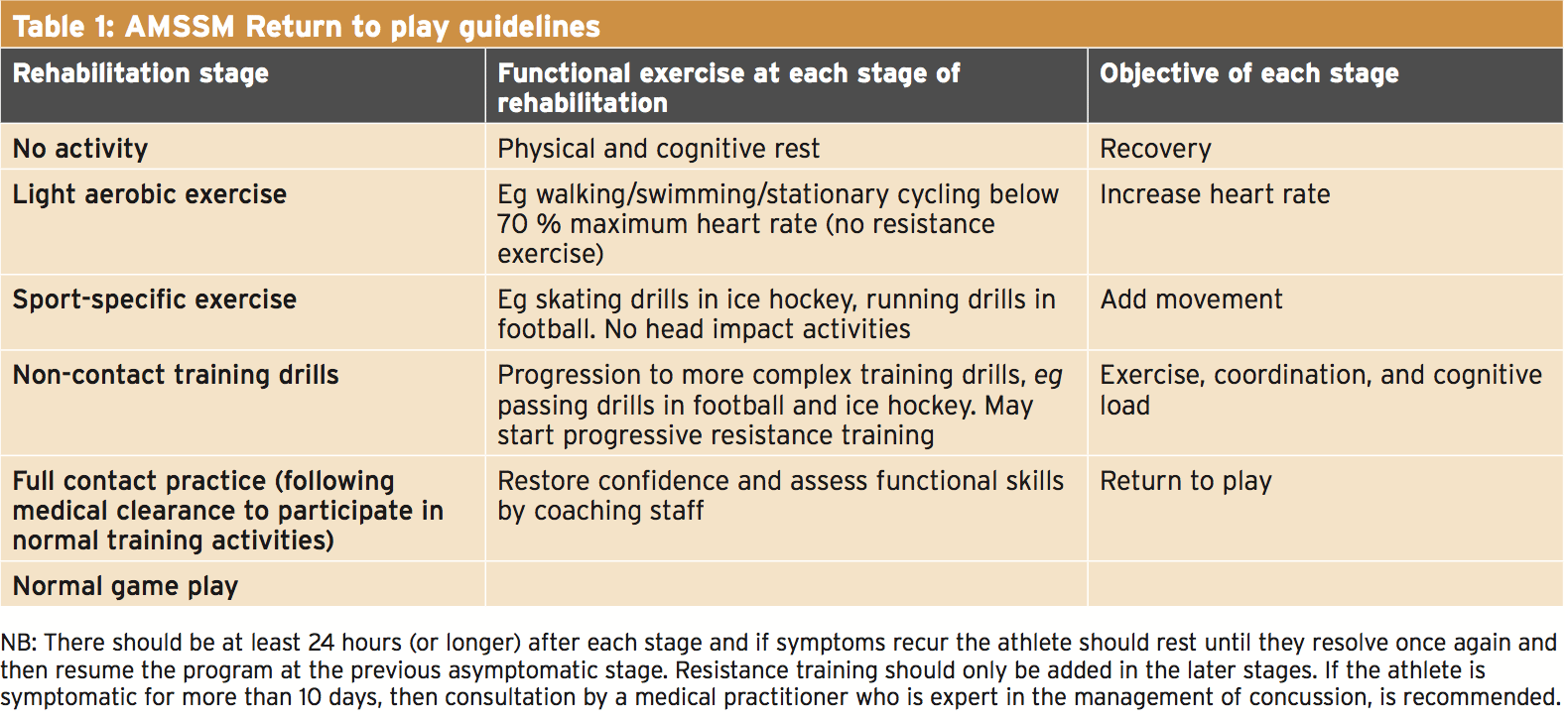
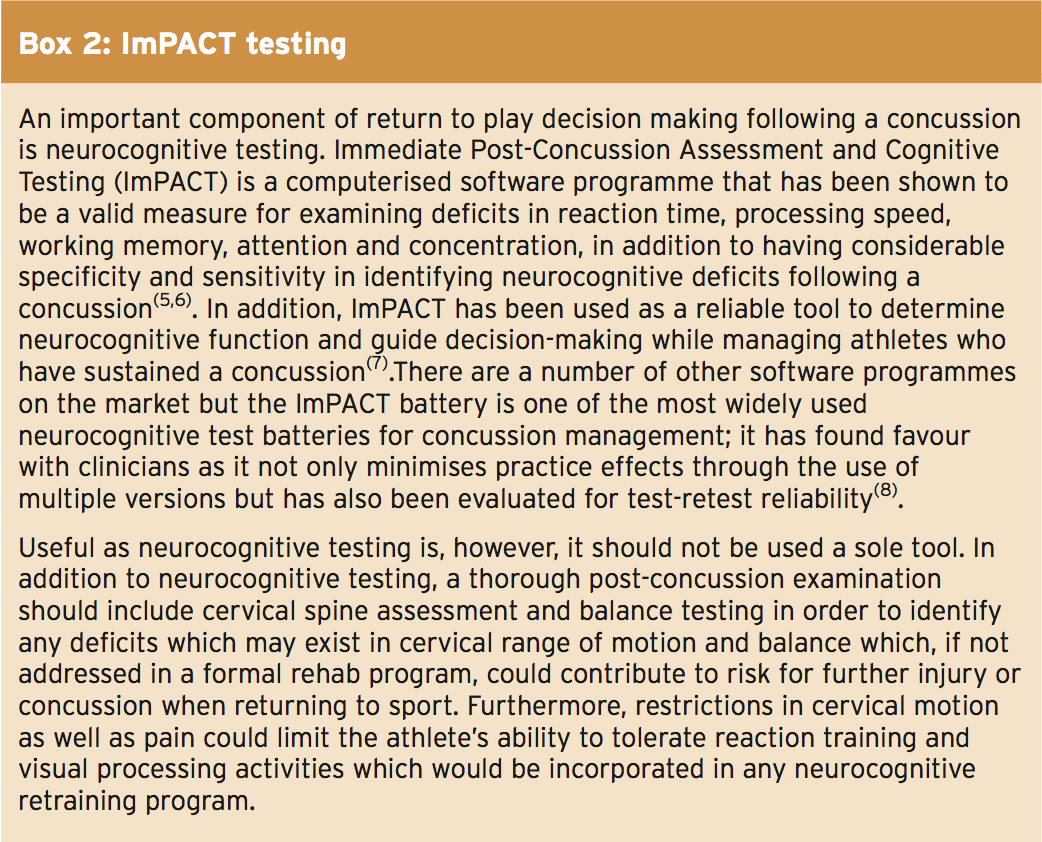
A few of the key points of initial diagnosis of a concussion are outlined in Box 1. The next thing to do is to consider a return to perform when concussion’s symptoms have escalated. Athletes returning to perform should first be medically cleared and then follow a stepwise supervised program, with defined stages of development (see Table 1). Athletes should NEVER be returned to perform on precisely the day of injury following the mildest concussion occasions.In 1 study, researchers discovered a potential link between response time and trauma(3). Employing ImPACT testing (see Box 2), they found that a composite score of higher that 0.545 seconds was connected to a two-fold threat of injury. A delayed response time is supposed to contribute to an increased injury risk because of a diminished ability for rectal control resulting from deficits in cortically driven reaction time and processing speed(4). Given the above, this suggests that analyzing, enhancing and restoring neurocognitive function must be a priority prior to returning an athlete to game following a concussion. Medical advice should incorporate concussion and orthopedic injury background in order to determine whether further evaluation is required to specifically identify risk factors for further injury.
Neurocognitive & Balance Deficits After Concussion
The treatment and management of balance and neurocognitive dysfunction in athletes requires a multidisciplinary approach and is based on constant reassessment of the presenting symptoms. The challenge for the clinician when handling persistent symptoms of the athlete that is post-concussive is currently ascertaining if is essential and if testing is matched by a set of symptoms.How common are long-term neurocognitive and balance shortages following concussion? A study completed in 2013 looked at the incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college athletes(9).
Researchers investigated the prevalence of recovery in 18,531 athlete- seasons over a period. A total of athletes with concussion and 166 controls who underwent pre-injury baseline assessments of neurocognitive functioning symptoms and balance were re-assessed immediately, three hours, and 1, 2, 2, 5, 3, 7, and 45 or 90 days after concussion. The concussed athletes have been stratified into typical (within seven days) or prolonged (more than seven days) healing groups based on symptom retrieval period.
Ten per cent (57) of the athletes experienced a prolonged symptom recovery, which was significantly associated with lengthier recovery on neurocognitive testing. In 45-90 days post- injury, symptoms were reported by the healing group, but minus shortages on equilibrium or cognitive testing. Recovery has been associated with unconsciousness following severe symptoms that were more severe amnesia and the blow. The researchers reasoned that a small fraction of athletes can experience impairments beyond the window of recovery and that prolonged recovery is associated with acute indicators of acute injury.
Another very recent research suggests that in certain athletes, balance shortages may still exist, even after medical clearance to return to play was granted(10). Researchers used centre of pressure (COP) dimensions on footballers to find out if stationary balance deficits had regained when concussed athletes had been cleared to return to play. Nine soccer players were matched. Equilibrium in the anterior-posterior and medial-lateral instructions was assessed through stance with eyes open and eyes closed. The results demonstrated that the football players exhibited anterior-posterior COP displacements that were greater with. However, the COP speed in the direction remained elevated compared to controls at return to play. The balance control deficit in the anterior-posterior direction suggested vestibular impairment due. The study’s authors pointed out that detected persistence of balance control deficits in football players that were concussed to play are very likely to be unnoticed by traditional assessments, which don’t incorporate higher-order steps of balance.
Further evidence for the importance of evaluation and treatment of balance and neurocognitive deficits comes from a review study published a year(11). Researchers gathered together original research studies, literature reviews, and clinical guidelines released between 1997 and 2012 about the treatment and management of vestibular and balance dysfunction in concussed athletes (the vast majority of articles dating post-2004).
They reasoned that in post-concussive athletes, impairments in balance may exist as a result of pressure. Their findings suggested that clinical evaluation information, neuropsychological testing, and reassessment are helpful method to determine severity of disorder and monitor course and resolution of symptoms. In terms of treatment and direction for balance and vestibular impairments, the evidence indicates that athletes should be assessed from initial impact to resolution of symptoms, in a stepwise manner. It is likewise recommended that neurocognitive and resolution of signs must be resolved prior to returning to play or game and, therefore, the athlete should be reassessed and treated until symptoms.
Neurocognitive Recovery & Aid Balance
Evidence suggests that an proper intervention strategy could improve neurocognitive function and an athlete’s equilibrium following a concussion. Not only can this improve sport performance, but as mentioned above, it may also reduce the risk of harm.As well as an ImPACT assessment for function, some kind of balance evaluation is also recommended to provide a baseline and measure of advancement over the intervention period. The Balance Error Scoring System (BESS) has found favor among clinicians as study suggests it’s both a valid and reliable measure for assessing postural equilibrium(12-14). A higher score on the BESS test suggests possible shortages in the somatosensory, visual, and vestibular components of the equilibrium system and that a number of balance errors, as evaluations are performed on surfaces.
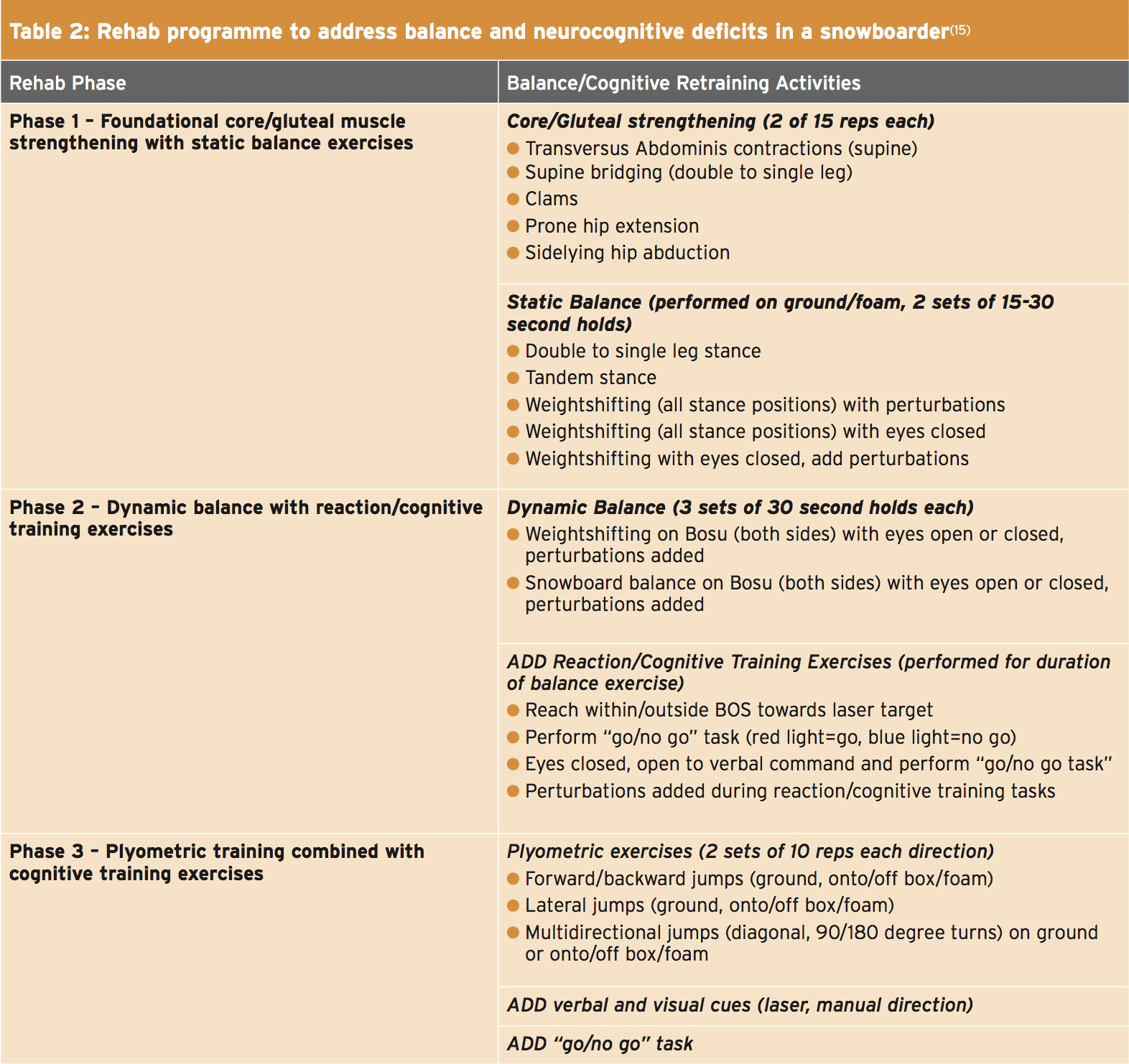
Concerning a practical intervention strategy, this will need to be tailored to the individual athlete. But a recently published case study appearing at treating equilibrium and neurocognitive deficits in a previously concussed snowboarder provides a helpful insight(15). The first stage of the rehabilitation system included instruction on proper transversus abdominis and gluteal muscle activation patterns through isometric and isotonic strengthening exercises with the goal of offering stabilization of the pelvic region during equilibrium exercises (Table 2). These activation patterns were incorporated with BESS testing exercise progressions, including:
- Standing with single leg leg and tandem stance support by performing exercises with eyes, on both the firm floor and polyurethane surfaces while challenging input;
- Performing static equilibrium positions (these were practiced before dynamic positions to allow for appropriate muscle and insertion activation sequences while challenging all components of the equilibrium system);
- Visual focus exercises, designed to strengthen muscles round the eyes that are responsible for dynamic gaze stabilization, to enhance concentration and focus when incorporating visual tracking (such exercises have been proven to enhance balance in addition to both hand and eye coordination also consisted of visual tracking activities at various rates across multiple airplanes(16)).
To aid rehabilitation retraining exercises have been united as a development. Examples included balancing on a surface that is unstable with perturbations short-term word recall and while finishing long, number sequencing, and word association tasks. Progressions included performing equilibrium exercises on unstable surfaces with eyes closed opening to do response training, which consisted of attaining within and external base of support to the laser target’s positioning.
The last phase of the rehab program comprised plyometric exercises combined with reaction training in order to integrate the dynamic components of leaping and landing while preventing deficits necessary for snowboarding. In particular, the athlete was educated on landing mechanisms with foot contact during jumps. Jumps were conducted to either verbal or visual command. Visual commands would comprise laser pointer or hands- direction. Previously mentioned neurocognitive exercises were also integrated in this stage.
Four training sessions within a six-week period generated improvements in neurocognitive processing and balance, reaction times. The athlete reported a occurrence of enhanced self-confidence and headaches. With some deficits present, it was recommended that the athlete continued with the rehabilitation program .
Conclusion & Summary
Concussion is a very common injury in sport 7 one with consequences that are possibly long-term. In severe concussions, the period of recovery is likely to be prolonged, delaying a return. But even when an athlete is deemed fit to return to perform, they could still experience some balance and neurocognitive deficits, which are often unnoticed by traditional screening. Balance and neurocognitive examinations like ImPACT and BESS can provide a measure of recovery in addition to information about the area of any such deficits. Regarding retrieval, the limited evidence available indicates a stepwise, innovative program to address balance and neurocognitive deficits, starting with core stabilization work, progressing to dual balance-visual tasks and to similar jobs involving cognitive processing, may be of significant value to the recovering athlete.References
1. Br J Sports Med. 2013 Jan;47(1):15-26. doi: 10.1136/bjsports-2012-091941
2. Am J Sports Med. 2012 Apr;40(4):747-55
3. Int J Athl Ther Train 2012;17:4-9
4. Am J Sports Med 2007;35:943-948
5. J Int Neuropsych Soc 2004;10:904-906.
6. Arch Clin Neuropsych 2006;21:91-99.
7. J Neurosurg 2003;98:296-301
8. Am J Sports Med. 2007;35:1284-1288
9. J Int Neuropsychol Soc. 2013 Jan;19(1):22-33
10. Gait Posture. 2014 Jan;39(1):611-4
11. NeuroRehabilitation. 2013;32(3):543-53
12. J Athl Train 2001;36:263-273
13. J Athl Train 2004;39:280-297
14. J Sport Rehabil 1999;8:71-62
15. Int J Sports Phys Ther; 2014, 9 (2) 232-241
16. Perceptual and Motor Skills 1991;72:863-866