In part I Chiropractor, Dr. Alexander Jimenez looked at chondral and osteochondral injuries to the patellofemoral joint, outlining the important pathophysiology and characteristic mechanisms for this injury, displaying signs and symptoms when this injury occurs. In part two, he considers the postsurgical rehabilitation of microfracture procedures.
Chondral and osteochondral defects of the patella and/or trochlear groove may be a debilitating injury for the athlete who frequently will require surgical intervention. The rehabilitation following operation can be lengthy and involved, with a firm commitment from the patient to ‘buy in’ to the post-surgical rehab.
A Substantial Quantity of work on microfracture methods and the subsequent rehabilitation post operatively was provided by Dr J Richard Steadman(1-4). Many of the ideas provided in this section are drawn from suggestions by the aforementioned author and also Tyler and Young(5).
It is difficult to prescribe an Specific time-dependant or criteria-dependant rehabilitation protocol to microfracture procedures as the recovery time is directly influenced by the size of the defect as well as the bodyweight of the patient. Big lesions (>400mm2) in heavier athletes will take considerably longer to recover than smaller lesion (200mm2) from lighter athletes. The development through phases depends on both of these variables in addition to the response of the post-surgical knee to increases loading.
What is consistent in rehab is the purpose of the initial period of recovery, in which it’s important to deliver an optimum physical environment via secure weight bearing and passive motion to permit the mesenchymal stem cells that leak into the surgically created marrow clot to distinguish and create new cells and an extracellular matrix. With time these cells and matrix will grow to form durable fix tissue in the original flaw. Any ancient loading on this tissue has the capacity to damage the healing tissue and cause a failed fix; therefore loaded movement is limited in the first post-operative interval and slowly reintroduced to permit adaptation in the newly formed fibrocartilage to happen(1).
Studies on primates with microfracture procedures revealed that at 6 months post- Operation, the fixed cartilage revealed restricted repair of chondral tissue but at 12 weeks the bone showed improved repair having a more mature hyaline cartilage(6). These findings suggest that constraints in weight bearing and protection of this defect site could be justified for greater than six weeks to allow the tissue repair to adapt to increased anxiety.
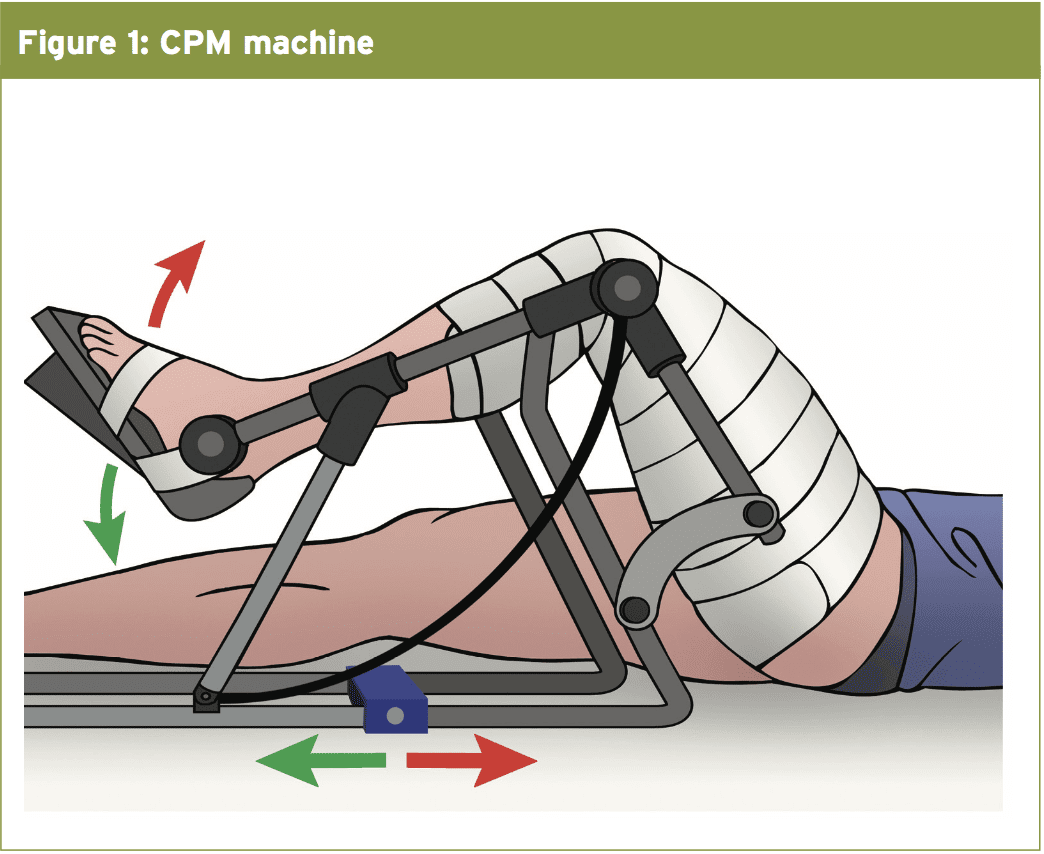
CPM
Weight Bearing
The patient is instructed to just ‘touchdown weight endure’ for the eight months following surgery to avoid any muscle contraction around the knee which may lead to compression of the tibiofemoral joint and/or patellofemoral joint. For accidents to the tibiofemoral joint, a motion limiting brace is not worn but to get a patellofemoral lesion the knee brace is proposed also is braced at 0°-20° expansion to avoid any flexion of the knee, which may result in the patella calling the femoral trochlear groove and make shearing at the maturing marrow clot. The brace is to be worn at all times except once the patient is in the CPM machine.Given the femoral condyles are Weight-bearing surfaces, restrictions are placed upon the amount of weight a patient is allowed to place upon the involved lower extremity. However, patellofemoral lesions are able to take more weight initially (around 30\% bodyweight) and that is progressed to weight bearing as tolerated from the brace from 2 weeks post-operation. For larger lesions of the patellofemoral joint (>400 mm2), weight-bearing is protected for the first 6 months.
After the first 8 weeks, the individual can increase the weight-bearing as tolerated. The patient using a patellofemoral lesion is invited to fully weight bear in the knee motion brace from 8 months onwards. Nevertheless the brace is gradually opened to permit more knee flexion. Patients are slowly weaned off crutches over weeks 9 and 10 and the brace removed at 10 weeks post-operation.
Mobilisations and patella/quadriceps mobilisations are initiated Immediately to prevent adhesion forming Between the patella and femur. This can also be encouraged in patellofemoral lesions. Total From early post-operative stages, except for The patellofemoral lesions, where flexion Isn’t encouraged. Manual therapy is a Defining characteristic in the first 12 weeks later Operation. Once full passive range of movement Is restored with full extension and complete flexion (without a continuing knee effusion), The emphasis moves from range of Motion and progresses to strengthening.
Strengthening
Gentle non-weight bearing quadriceps contractions are encouraged from an early stage such as inner array quadriceps setting, right leg lift and muscle stimulators (on the atrophy setting), and this is continued for the first 12 weeks after operation. At this stage, supine/side lie inclined hip exercises are invited with resistance to keep some proximal hip muscle hypertrophy.In 12 weeks post-surgery, the patient ought to have near full range of passive and active motion, and strength training could be safely progressed. In tibiofemoral lesions, the ranges of movement allowed for strengthening are initially confined to 0 degrees to 300 degrees through this 12per week phase of rehab. Full weightbearingisallowedasthepatient feels comfortable; nevertheless the range is always limited in this age.
In patellofemoral lesions, the surgeon will notice during operation where stage of knee flexion that the patella enters the trochlear groove and moves over the newly generated marrow clot. As an instance, at a small patella lesion, the surgeon may note that the patella contacts that the femur out of 20-40° of knee flexion, however before and following this range there is not any patella to femur contact. Loading the knee joint in flexion is subsequently averted in this 20-40° range for the first 4 months post- operation but loading up to 20° and out of 40° onwards is allowed.
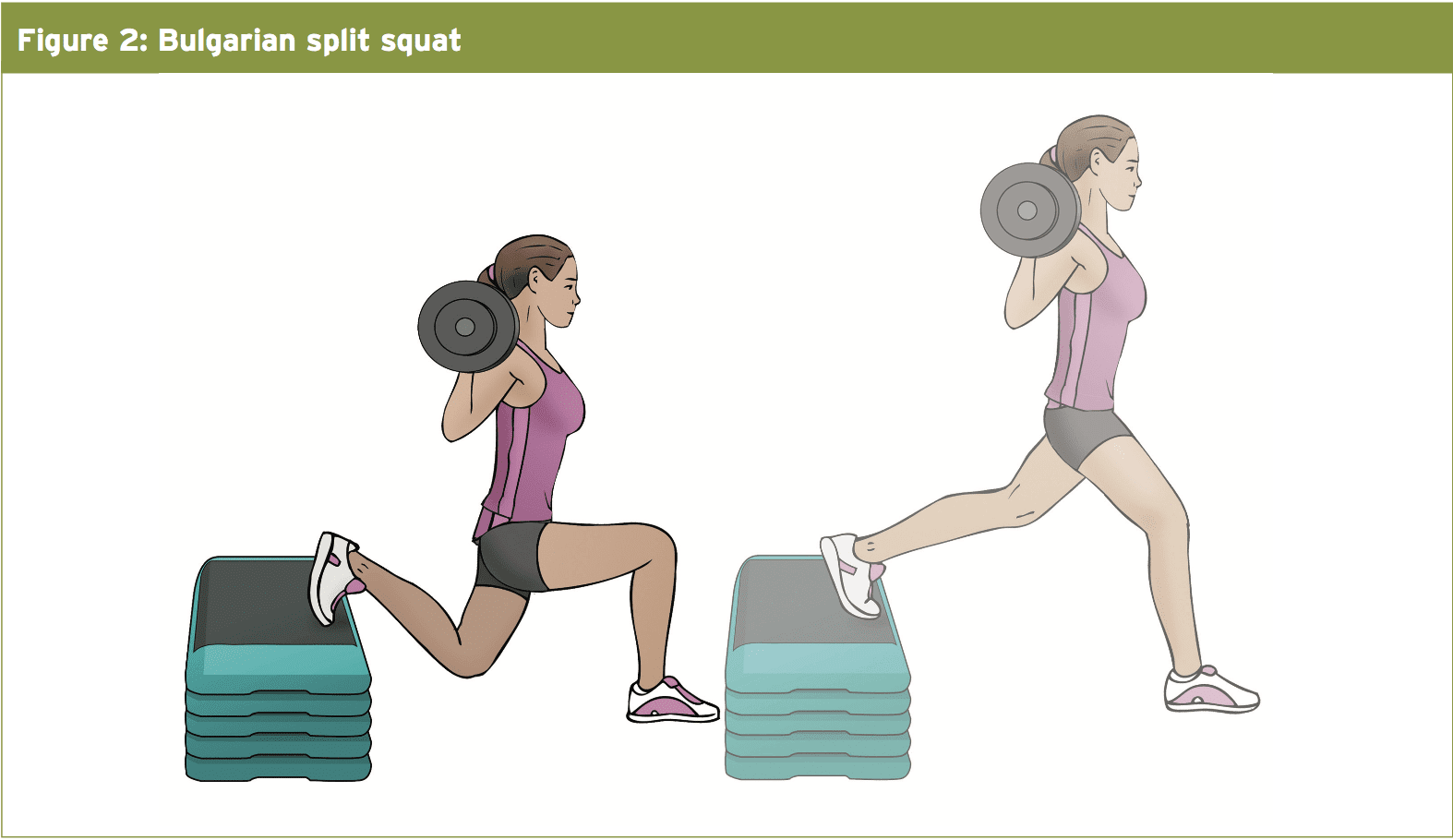
Loading may take the form of single leg squats, 1 legged leg presses and additional split squats (see Figure 2). Isometric holds can be added in the upper knee flexion angles and muscle stimulators can also be utilized along with these movements. Isometric holds can be added in the maximum knee flexion angles and muscle stimulators can also be utilized along with these motions.
Hip dominant movements that don’t involve knee flexion under load can also be improved in this stage. By the week 24 onwards, it is expected that the individual will then be comfortable enough and have sufficient strength to advance to more traditional weight training applications, incorporate more volatile Olympic lifts and also have begun simple plyometrics-type moves. These are all gradually improved throughout the last stages of rehabilitation.
Cardiovascular Training
In tibiofemoral lesions, gentle turning on the bicycle and deep water running (no touching the pool bottom) could be started when 1 week post-operation if the lesion is small. But, in larger lesions (>400mm2), this really is postponed to 4 weeks post surgery. At 12 weeks post-surgery, many non-impact cardio function is allowed for example spinning, water jogging, running, and treadmill walking.Spinning on the bike is completed initially without resistance until the patient can attain a comfortable 45 minutes pain free, and without post-exercise effusion. Then the load is slowly inserted and the time reduced to 20 minutes. This is built up to 45 minutes before another increase in load is allowed. This is gradually increased 5 minutes each session-assuming the knee suffers no pain and no post exercise effusion.
Straightforward running mechanics drills could be started in 16 months post-operation, with a focus on drills to enhance hip/ knee/ankle mobility. The running time is increased 1 minute each week and walking period reduced each week so that after 5 months the patient should be able to run 20 minutes continuously.
Bodyweight is increased 10\% per week so that by 5 weeks they’re up to 100\% body weight. Speed and endurance drill are actively commenced at around 21 weeks post-operation and slowly improved over a 4-5 week period.
By 26 months post-operation, the athlete must currently be able to perform the majority of the mobility, speed, agility kind drills prior to being reintegrated into group training. Generally athletes in high impact sports that involve cutting, landing, pivoting and abrupt deceleration can take 9 weeks to completely recover their physical abilities and also the confidence needed prior to return to competition.
Long-Term Impairment
The long-term outcomes after having a microfracture procedure demonstrate some handicap to athletic purpose can be expected. After the microfracture procedure was performed in several athletes, improvements in role were initially seen. Lysholm knee scores increased by 56.8 to 87.2 after surgery while Tegner scores increased from 3.2 to 6 in the two-year follow up. The athletic population revealed an 80\% increase in sports activities during the initial 2 years, but this gradually declined to 55\% at 5 decades. This is sometimes attributed this decrease to the organic decline in your ability to perform at a high level with age in addition to the chance that the fibrocartilaginous repair tissue gets less resilience and might deteriorate over time(8).But, those athletes that have experienced a microfracture procedure will have the expectation that they’ll return in competition in a span of 6-9 months after surgery. Once they’ve progressed through the phases of rehab, particular outcome measures may be used to determine the key exit criteria for complete return to sport. These are:
- Minimum knee effusion article training
- Return to maximum jogging velocities
- Confidence in changing and landing direction
Conclusion
Knee micro-fracture procedures involve a lengthy rehabilitation process which involves controlled passive movement with protected weight bearing. Because of the debilitating effects of protracted non invasive and lack of competitive quadriceps exercises in the early post- operative period, the patient may expect significant quadriceps wasting and functional limitation at the ten to twelve week stage following surgery. Therefore regaining full range of movement and redeveloping quadriceps muscle power is going to have a lengthy lengthy rehabilitation period. When the athlete has attained adequate weight bearing power, then return to functional capacities like running and changing direction will also be lengthy time dependant endeavour. Patience and consistency are required by both therapist and patient to slowly recover function, having the expected time to return to sport confidently often being greater than two weeks in duration.References
1. Clin Sports Med. 2010; 29; 257-265
2. J Knee Surg. 1980; 15:170-176
3. J Arthroscopic and Related Surgery. 2003; 19(5): pp 477-484
4. J Knee Surg. 2003; 16(2), pp. 83–86
5. Curr Rev Musculoskelet Med. 2012; 5:72–81
6. Am J Sports Med. 2005;33(5):680–5
7. Am J Knee Surgery. 1994; 7: pp 109-116
8. Knee Surg Sports TraumatolArthrosc. 2005;13:213–21