Chiropractor, Dr. Alexander Jimenez reviews the possible approaches to deal with these hamstring issues — and the evidence offered.
Tendon injuries account for 30-50% of accidents reported to physiotherapy clinics and also 30% of all running injuries relating to tendon overuse (1). If handled tendinopathies are complicated to control and might cause a from long-term and sport harm. High heeled tendinopathies (HHT) are less commonly recognized than other tendons of the thoracic and might present as either deep buttock pain and or as anterior thigh pain(2).
The Objective of this review is to provide an insight into the direction for HHT and when to explore injection therapy. High hamstring tendinopathies may also be referred to as proximal hamstring tendinopathy (PHT) or hamstring origin tendinopathy (HOT). The research pertaining to conservative therapy for HHT is restricted(two) and therefore some of the research provided in this review is connected to tendinopathies of additional major joints of the lower limb.
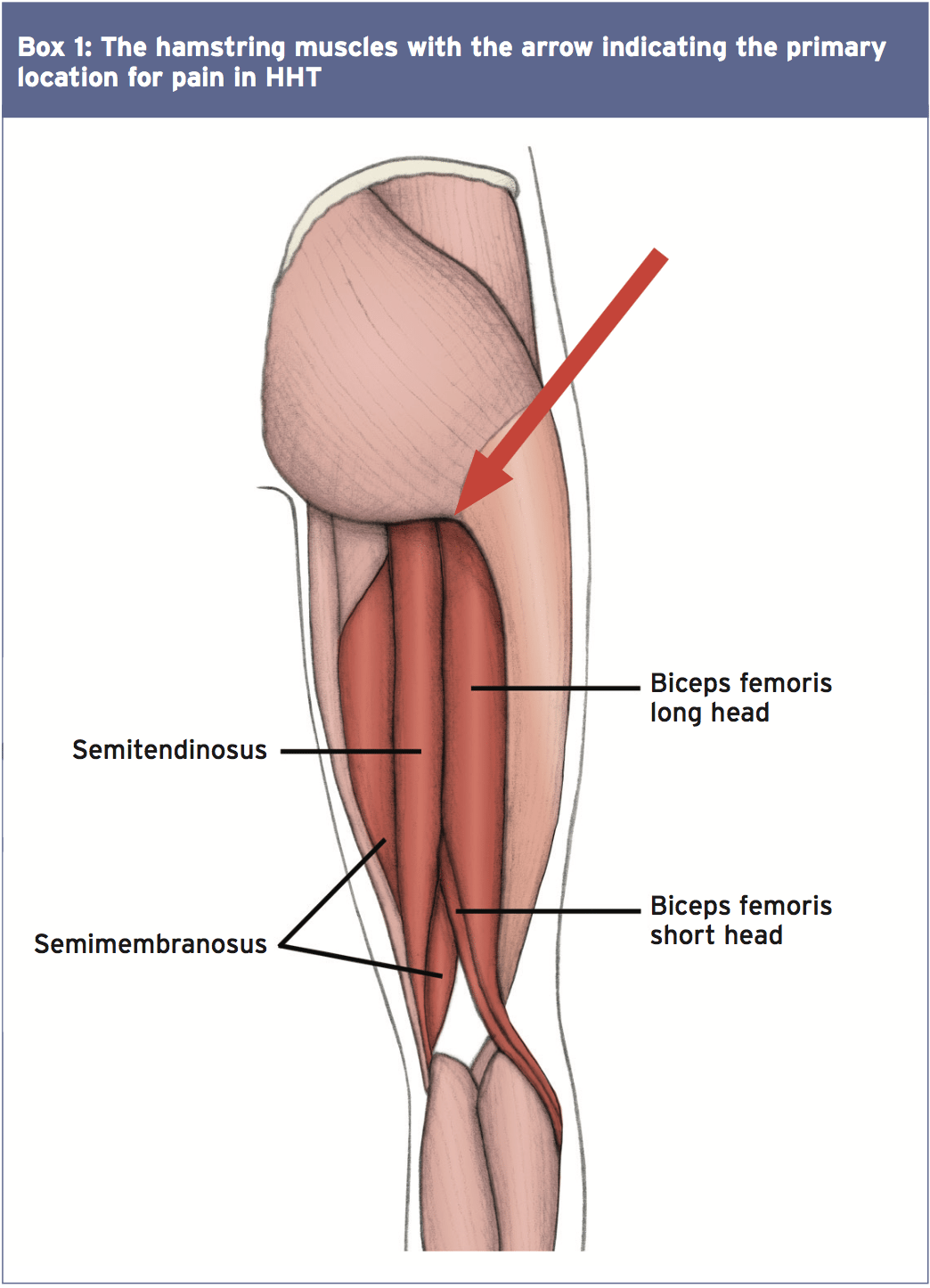
Anatomy Hamstring Muscle
Pathophysiology
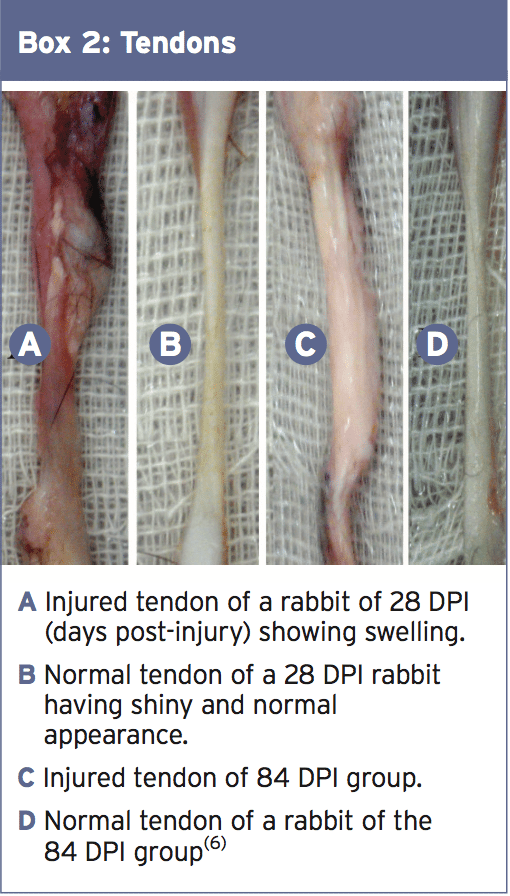
The expression tendinosis is used to describe the process of degeneration from tendinopathy, although many still use the age old term of tendinitis. The ‘itis’ suggests an inflammatory reaction is present but intratendinous degeneration is defined as being hypoxic and calcific from factors like reduced blood flow, aging and microtrauma rather than posing as an inflammatory response(4). A hypothesis explaining the pain undergone at a tendinopathy is from the ingrowth of the vessels and nerves termed as ‘neovascularisation’ which causes a pain response from the swelling of an irrititable limb(5).The part of a tendon appears as grey and of dull look as it loses its glistening white look as seen in Box 2(6). The illustration of an injured tendon in Box 2 has been a limb removal combined with repair of the superficial digital flexor tendon in rabbits and wasn’t a tendinopathy. The authors,(6)) however, drew comparisons to the therapeutic stages in tendinopathies in humans in exactly the same timelines of 28 and 84 days (four and 12 months). The picture illustrated in section C box 2 reveals the biomechanical properties of the immature collagen fibers and significantly lesser to the normal tendon in sections B and D.
Clinical Assessment
The hamstring tendon is placed under load when the knee is extended and the hip is completely flexed. Running, or running-related sports, induce an individual to tendinopathy due to the extended length the thoracic is stored within this eccentrically loaded position(7). Additional factors exposing somebody to HHT might consist of low hamstring to quadriceps muscle ratio, inadequate warm-up protocols, preceding hamstring injury and reduced hamstring flexibility(2). Other factors could include pelvic dysfunction and diminished activity of the core stability muscles and therefore a wide evaluation should be undertaken with the onset of deep buttock pain (3).Pain may be included by symptoms of HHT during repetitive eccentric loading, acceleration during jogging and in extreme instances sitting on hard surfaces. The taking the shoe off test, resisted by the uninvolved foot, was proven to have a High sensitivity and specificity of 100% for hamstring-related injuries and ought to be considered to be used with a suspected HHT(8). Normally pain is felt on active and passive stretching of the hamstring muscles at the origin attachment with pain too experienced on palpation of the ischial tuberosity(two). Moreover, there is minimal decrease in power of the hamstring muscles with knee flexion or cool extension in isolation without a neurological deficit is current unless additional lumbosacral spine pathology is included(two). Pain is often detected with the hip completely flexed placing the best load on the muscles like phase of the swing period in gait’s terminal when the knee is extended.
Conservative Therapy
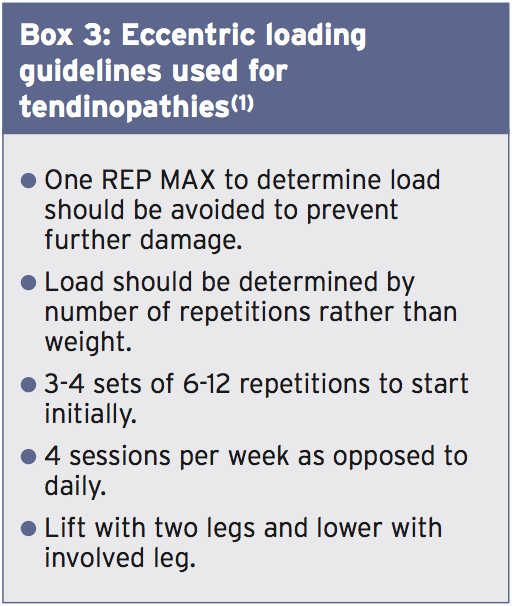
An eccentric contraction, which refers to higher tension of a muscle-tendon unit through lengthening, has been widely employed as a treatment tool for tendon pathologies(7). Tendons need seven and half times less oxygen compared to skeletal muscle does and throughout the eccentric phase oxygen consumption rarely rises to more than double its resting value(9). Research compiled through the 1970s indicated that faster concentric contractions demand a greater oxygen supply and consequently an increase in heat generation and cellular metabolism happen(10). Consequently a greater quantity of waste products are transported into the active site possibly causing a chemical reaction of nerve endings and an increase in pain(10). Thus the justification for bizarre exercise in the management of tendinopathies is supplied as opposed to concentric contractions.Research has suggested that eccentric exercise boosts collagen fibre cross-linkage inside the thoracic that eases remodelling of the injured tissue(7). This was supported by Langaard and colleagues who found that 12 weeks of eccentric loading of the Achilles tendon improved the collagen synthesis rate of type one fibres(5). It’s been said that pain and neovascularisation are reduced following a different 12-week bizarre training program for an Achilles tendinopathy(11). A period of 12 months is considered sufficient for tendon regeneration to occur, although positive outcomes might be observed.
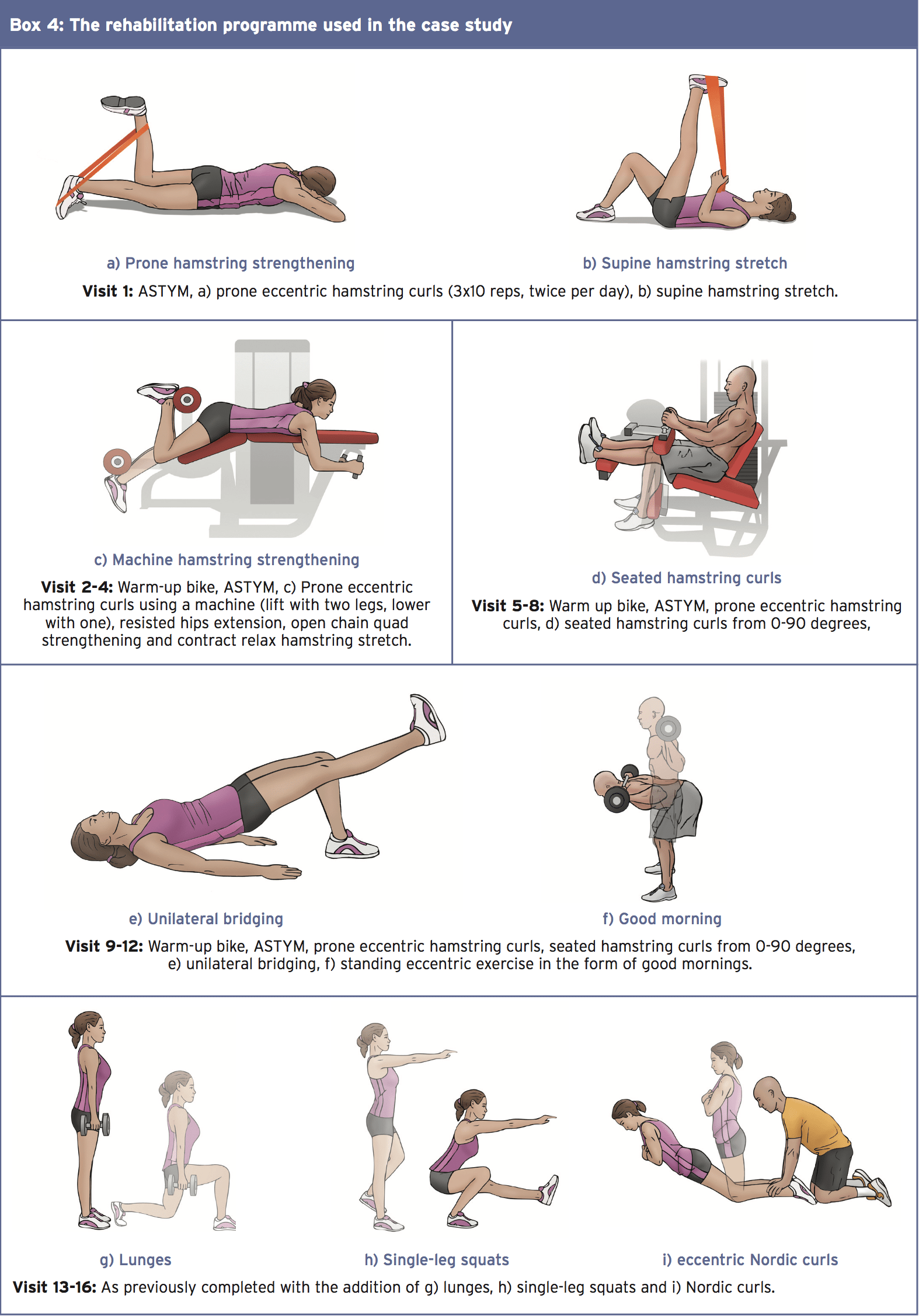
A case study was printed in the Journal of Manual and Manipulative Treatment of a 41-year-old feminine Recreational runner who completed five Three-mile runs per week (7). The individual Had a start of buttock pain that is right however had been Able to continue training at a lesser Intensity for 12 months. The patient then developed left buttock pain with worsening Pain on Patient to cease running. The Patient’s objective was to make a return that is full to running. Pain ranged from 0-6/10 on VAS scale depending on activities. Pain Was walking In and out of automobiles and sitting on hard Surfaces and when taking off shoes (‘taking off a shoe evaluation’).
An assessment of the individual in the case analysis (7) suggested straight leg testing with ankle dorsiflexion and slump tests were negative bilaterally and pain-free thoracic spine motions with over- stress in all directions were unfavorable. Pain in buttock with lumbar flexion with her knees fully extended was, nevertheless, noted. No pain on palpation of the lumbosacral spine was detected but the individual has been tender on the ischial tuberosity and the proximal two inches of the hamstring tendon. Pain was not discovered on the hip quadrant test of either hip and no hassle has been noted on sacroiliac joint testing. Hip flexors, abductors and external rotators were all pain-free and recorded as 5/5 on the Oxford scale. Hip extension was slightly painful on both sides with a reduction in strength 4/5. Knee flexion reproduced greater pain amounts on both sides with 4-/5. Pain was replicated on both sides by extending the knee with the hip claimed in 90 degrees of flexion.
The outcome of the case published by McCormack(7) signaled a steady progression during with no hassle on taking shoes off at visit . After the treatment the patient has been able to walk two and half an hour pain-free and after 12 remedies able to jog one mile pain- free. After 16 treatment sessions that the patient reported 95% postoperative improvement and managed to operate for 2 weeks and a half miles pain-free.
Shockwave Therapy
Shockwave therapy has been cited as being an effective tool for handling HHT. A study investigated the effects of hamstring resistance training (not specifically eccentric loading) using anti inflammatory drugs and shockwave treatment on the tendinopathy of the proximal hamstring in 40 professional athletes (12).) The shockwave implemented was 2500 impulses per session without anaesthesia of a single session per week for four weeks. The four-week study, which used a randomized controlled study design, found at three months post-study which 17 of the 20 athletes that received shockwave had a decrease in pain of 50%, whereas in the treatment group only two patients received a decrease in their pain from 50 percent. Even though the contrast between the shockwave versus therapy group should not be contrasted against bizarre training, it’s significant evidence for the use of shockwave in curing HHT.Steroid Injection Therapy
Research of tendinopathies has suggested that 20% of individuals will stay as symptomatic at three to six months after a conservative direction program was applied(13). Further interventions must be researched at this point and one of the options is in the kind of injection therapy. It needs to be noted that once injection therapy has been carried out it’s key that the conservative management program be continued to get optimum results.A fluoroscopy-guided peritendinous corticosteroid injection was provided for 18 athletes using HHT diagnosed by MRI (two). The followup, on average being 21 months, also suggested by questionnaire that pain had considerably decreased from 7.22 pre-injection into 3.94 article injection. The results also indicated that athletic involvement had significantly increased from 28.76\% to 68.82\% with 38.8percent of individuals being completely asymptomatic in a mean follow up of 24.8 months. There was no proof of a conservative programme and this is the limit of the research. Had a structured management program been supplied it would be beneficial to draw on the results obtained and draw comparisons between the classes.
Researchers from the University of Copenhagen studied the effects of corticosteroid injections, bizarre training and significant slow resistance training on patients with patellar tendinopathy(14). With a randomized controlled single blind study design, 39 male participants were assigned to one of the three intervention groups. Factors measured were work, pain, symptoms, tendon swelling and vascularisation and limb mechanical components prior to the study, in 12 weeks and at six months after the analysis.
The outcomes of the research yielded that each intervention significantly improved in pain, symptoms and function during the initial 12-week period. What’s more, pain, symptoms and function continued to improve in the eccentric and heavy slow resistance training groups at the follow-up but had considerably diminished in the corticosteroid injection group. Additionally at the six-month follow-up the heavy slow resistance training team suggested they were the very satisfied with the therapy result which coincided with increased collagen turnover. Even though the corticosteroid injection alone provided favorable first results at 12 weeks the results weren’t substantive for its long- term clinical effects.
Overview
A rehabilitation program invented for HHT should depend upon the findings in the first examination and also the load in which the hamstring muscle may withstand. What’s more, the sophistication and load of the rehab exercises should be particular to the patient’s pain tolerance. If the tendon is not responding to conservative treatment then steroid injection is an avenue to explore based on the individual’s age and present symptoms following a period of 12 weeks. To draw greater comparisons involving steroid injection therapy and a conservative management plan, research should endeavor to contrast the effects of both forms of treatment using randomized research design. The current review is unable to provide a firm conclusion at this stage as additional research is required.References
1. The Int J of Sports Phys Thera. 2011 Mar; 6 (1):27-45.
2. The Ortho J of Sports Med. 2014; 2 (3).
3. J of Chiro Med. 2011; 10: 93–99.
4. Br J Sports Med. 2002; 36: 239–249.
5. Scand J Med Sci Sports. 2007; 17: 61–66.
6. Sports Med, Arthro, Rehabili, Thera & Techno. 2012; 4: 14.
7. J Man Manip Thera. 2012 Aug; 20 (3): 142–146.
8. Clin J Sport Med. 2006 Mar; 16 (2):166-9.
9. Sports Med. 1986; 3: 114-135.
10. J Physiol. 1976; 260: 267-277.
11. Knee Surg Sports Traumatol Arthrosc. 2003 Sep; 11 (5): 327-33.
12. Am J Sports Med. 2011 Jan; 39 (1): 146-53.
13. J Bone Joint Surg Am. 1999 Feb; 81 (2): 259-278.
14. Scand J Med Sci Sports. 2009 Dec;19(6):790-802.