In part 1 of his article, Dr. Alexander Jimenez examined the relevant anatomical features and biomechanical factors of the patellofemoral joint and subsequent dislocation of the patella. In part 2, he looks at the arguments for and against surgical repair following first-time primary dislocation, and also provides a comprehensive post-operative rehabilitation program.
The contentious issue regarding primary patella dislocation is whether or not the patient will need immediate surgery or if a period of conservative management is warranted. Even in the presence of a cartilage lesion, surgical intervention is not always needed. It may be necessary to only fixate a large displaced osteochondral fragment (if they are big enough) and have enough bone to be suitable for surgical fixation. Smaller fragments that are not suitable for fixation may only require conservative treatment.
Although recurrent patella dislocation is the exception and not the rule, many patients continue to be symptomatic following their dislocation episodes. It has been noted that at six months post-injury, 58% of patients continue to have limitations with strenuous activity(1). Failure to return to sport is found in as many as 55% of patients. For these reasons, surgical intervention has been advocated in an attempt to reduce the recurrence rate, which has led to confusion and controversy regarding surgical indications in the acute setting(2).
Conservative Vs. Surgical
There have been a few studies comparing conservative versus surgical treatment after first-time patellar dislocation. These studies often report inconsistent results, and usually, the limited number of the patients in these studies reduces the validity of the studies. On the overall balance of data in these studies, it has been shown that in first time dislocations surgical intervention does not reduce the rate of subsequent dislocation(3), and in the few studies showing that it does, it is only a small improvement(2,4-6).
Furthermore, functional outcome scores between surgically repaired patella dislocations versus conservative management may be slightly better(7), more or less the same(8,9) or in some studies actually worse(4,10)! Regarding surgery versus conservative treatment in recurrent patellar dislocation and chronic patellofemoral instability, there are no randomized clinical trials at all.
To summarize, non-operative treatment is indicated after a first-time patellar dislocation in a vast majority of patients. Surgical treatment is indicated primarily in case of relevant concomitant injuries such as large displaced osteochondral fractures, and secondarily for recurrent dislocations. After a second dislocation event, a much higher risk of re-dislocation exists (49%), and surgical intervention may be considered(11).
Conservative Management
If the decision to manage the primary patella dislocation is non-surgical, then usually a period of brace immobilisation will be required in the early post-injury period.However,littleevidenceexiststo guide the period of immobilisation, and whether the brace needs to be fixed in extension or has some range allowed.Immobilisation in an extension brace for an extended period will allow time for the medial patella structures (primarily the MPFL) and a better environment to scar up and heal. This will however lead to more atrophy in the quadriceps, scar tissue formation, joint stiffness and at times patient frustration and poor compliance. Therefore, many clinicians prefer a short period of immobilisation followed by early rehabilitation wearing a patella stability brace.
Current evidence suggests that a short period of immobilisation in extension is advisable after the first dislocation event by placing the patient in an extension brace for 6 weeks(12). This can be immediately followed by physiotherapy or patient- directed home therapy focusing on range of motion and quadriceps strengthening. In a patient who finds six weeks of immobilization unacceptable, a 3-week period of immobilisation may be performed with the understanding that a higher re-dislocation rate may result.
Other researchers have advocated the use of patella braces instead of immobilisation in the early management of acute patella dislocation – in order to allow early weight bearing and range of movement(13,15). The goal of bracing is to restore proper alignment and protect against re-dislocation and subluxation, while at the same time allowing for quadriceps strengthening during the rehabilitation programme.
Other methods of stabilising the patella include patellar taping (McConnell method)(16,17). Taping the patella has been found to activate the VMO earlier than vastus lateralis, and such timing changes have beneficial effect on patellofemoral mechanics, promoting movement of the patella into the trochlea groove early in flexion(16).
Conservative management seems to be the treatment of choice in patients with acute patellar dislocation, provided that the generally accepted indications for surgery, such as evidence of osteochondral fragments and major defects of the parapatellar ligament complex are excluded. However, the lack of bony restraint in some cases makes conservative muscle rehabilitation very difficult. Therefore surgical assistance to improve the passive stability of the joint may be required. The exact rehabilitation protocol following the period of brace immobilisation would be similar to the post-operative schedule mentioned below.
Operation Techniques
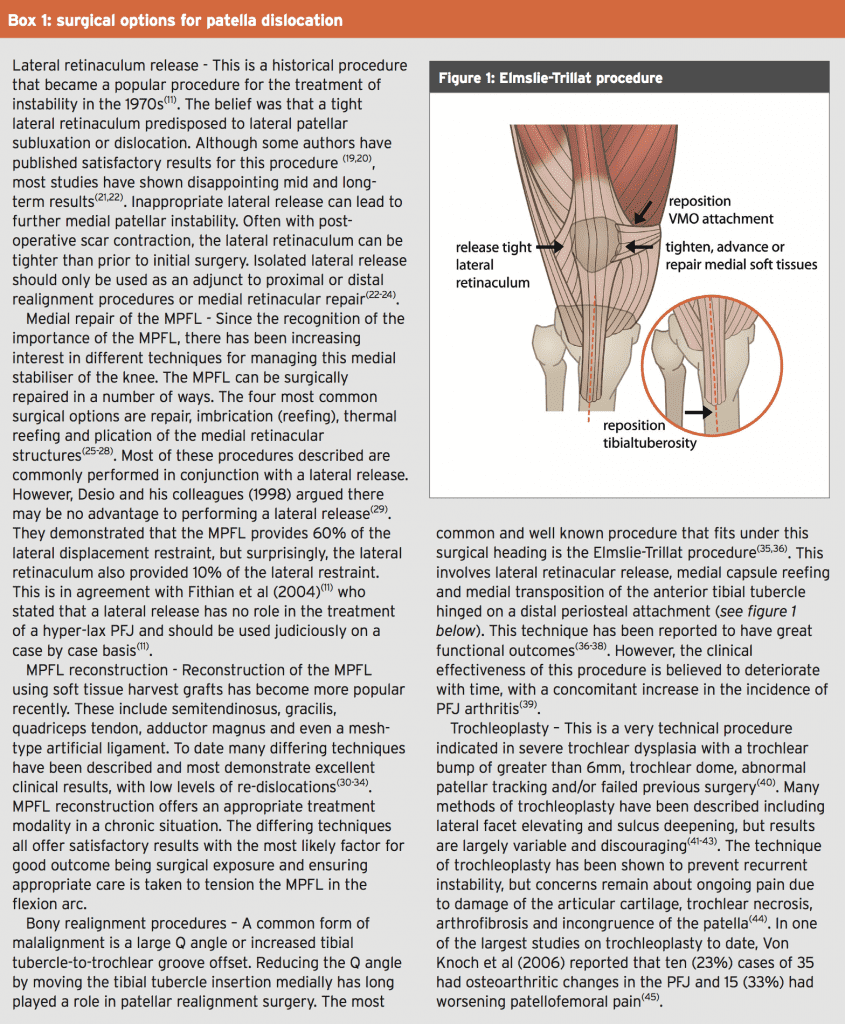
Surgical intervention is appropriate for those patients who suffer recurrent patellar subluxations or dislocations, in the acute setting for those with associated large displaced osteochondral lesions, and in those where conservative treatment has failed.The type of surgery available may vary depending on surgeon. Some surgeons address the bony elements and others the soft-tissue components, in a proximal or distal procedure. However, the gold standard of surgical treatment is yet to be clearly defined in the literature, with over one hundred surgical techniques described in the literature(18). The different types of surgical procedures are listed in Box 1.
Post-Operative Routine
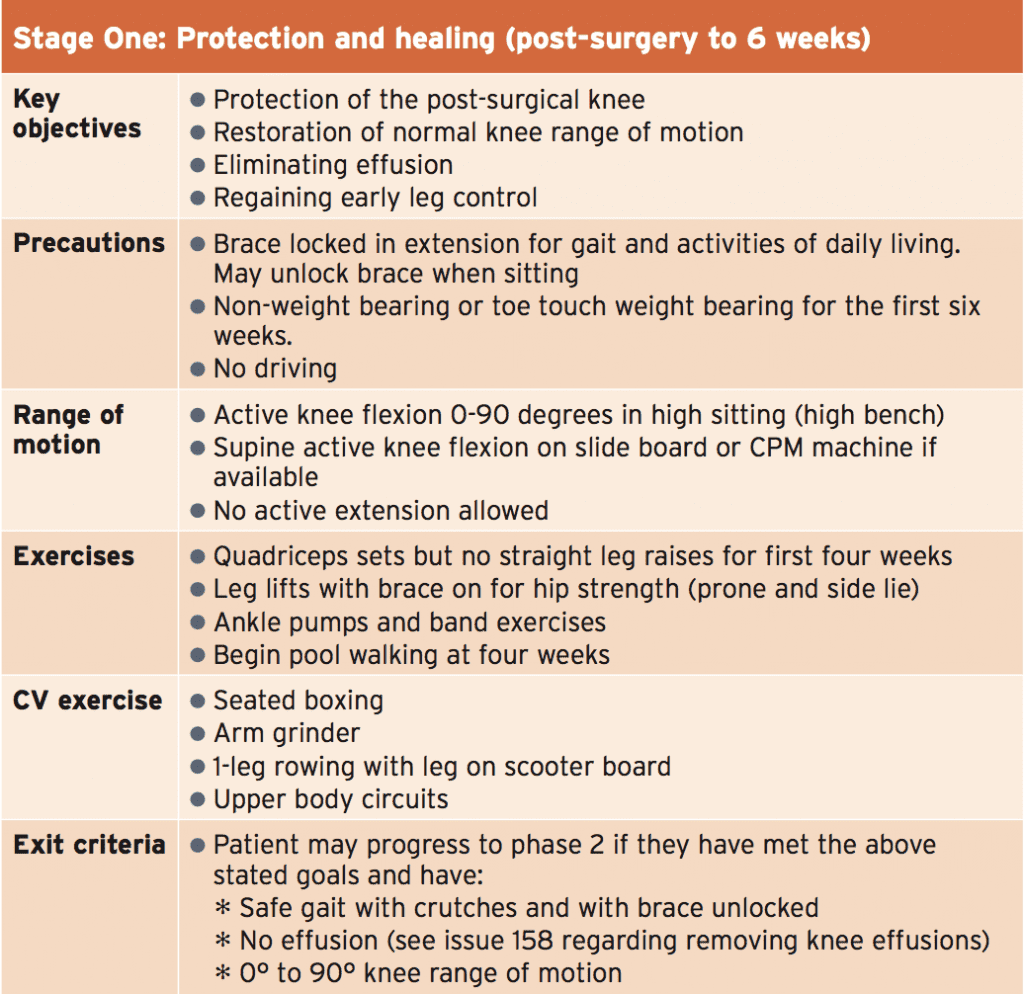
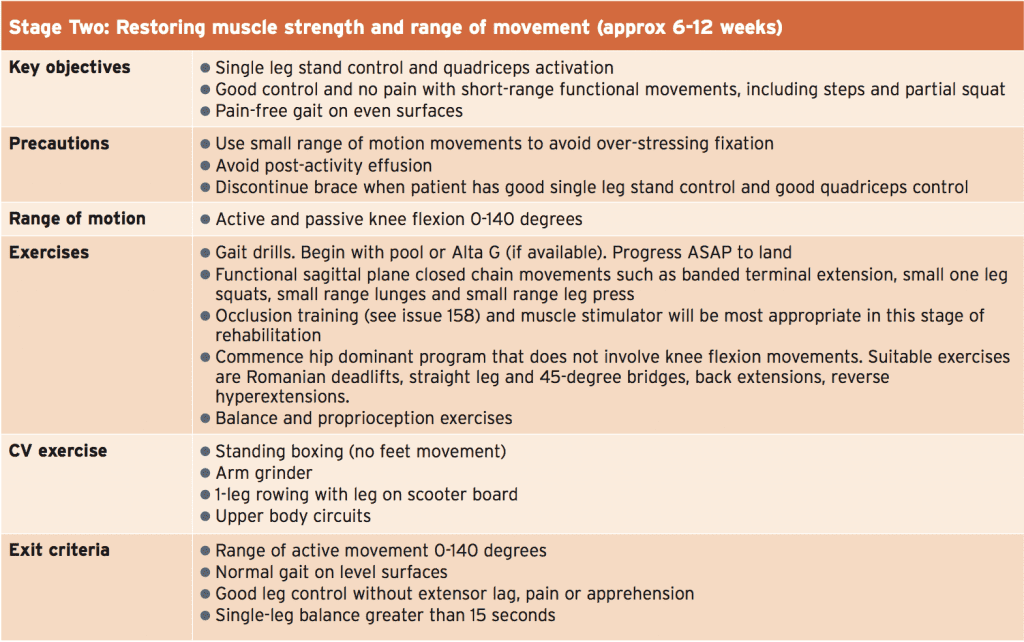
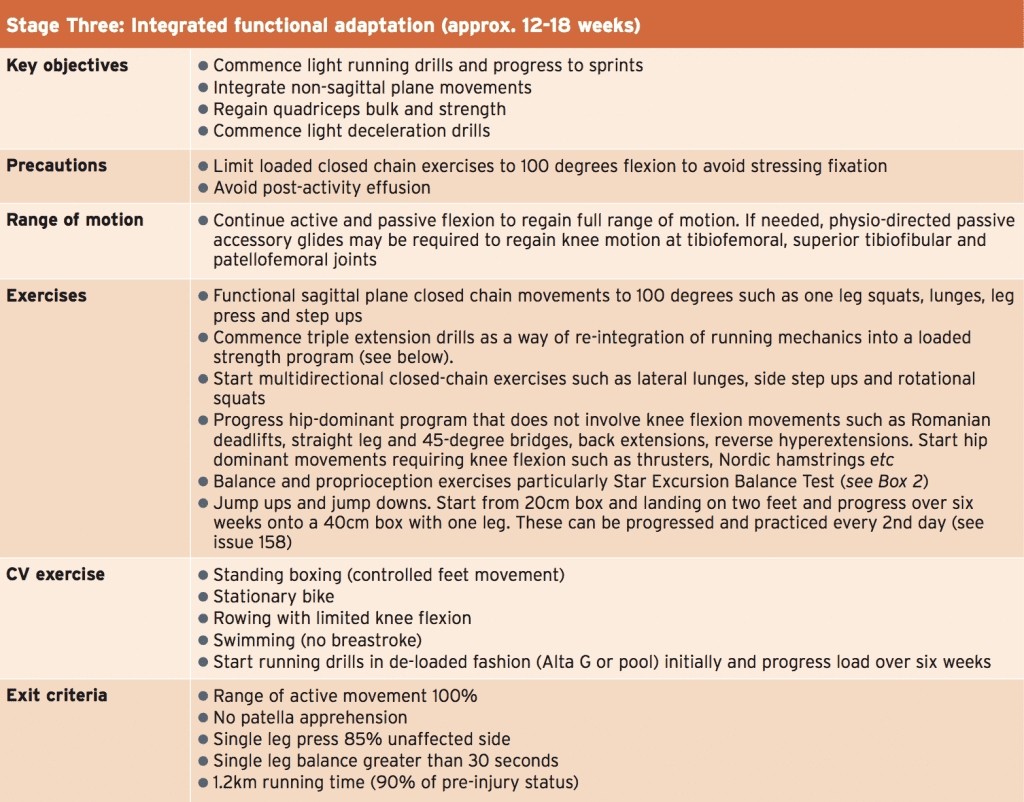
The exact time frames and procedures in the post-operative stage will depend on whether the surgical procedure chosen involves the bony elements and/or soft tissue elements, and whether the procedure was performed as an open procedure or under arthroscopy. These factors will all influence the length of time of post-operative bracing and weight bearingstatus.
What is presented below is a criteria- based progression that follows a logical and sequential order in the rehabilitation stages. For some post-operative patients, the stages can be either extended or compressed depending on the type of surgery undertaken. Furthermore, many of the key rehabilitation principles regarding time frames and key elements that are relevant in repair of an acute patella dislocation are similar to the principles outlined in the piece titled ‘Rehabilitation following LARS procedure – Part 2’, which was presented in SIB issue 158. The principles relevant to the following topics and which are covered in Issue 158 include:
In most instances, immediate repair of the acutely dislocated patella is not needed unless there is an associated large displaced osteochondral lesion. Surgical repair is also usually warranted in cases of failed conservative rehabilitation, whereby the athlete dislocates the patella on repeated occasions (‘three strikes and you are out rule’) or in failed conservative rehabilitation whereby the athlete suffers ongoing patellofemoral pain and dysfunction.
- Importance of removing knee joint effusions
- Occlusion training
- Developing the capacity to decelerate Sand-based training
- Trampoline drills
- Functional testing – eg crossover hop tests
In Summary
Acute patella dislocation is an uncommon but potentially debilitating condition for the athlete, particularly the young female athlete. Thorough investigative work up is required to differentiate this injury from other acute traumatic knee injuries such as ACL rupture, osteochondral defects, and to also view the integrity of the primary medial stabiliser – the medial patella femoral ligament (MPFL).In most instances, immediate repair of the acutely dislocated patella is not needed unless there is an associated large displaced osteochondral lesion. Surgical repair is also usually warranted in cases of failed conservative rehabilitation, whereby the athlete dislocates the patella on repeated occasions (‘three strikes and you are out rule’) or in failed conservative rehabilitation whereby the athlete suffers ongoing patellofemoral pain and dysfunction.
Many surgical options exist. However the more common variations involve repair of the MPFL with or without an alignment procedure, such as an Elmslie-Trillat procedure. The time frames involved in post-surgical rehabilitation can be lengthy and are similar in progressions as an anterior cruciate ligament reconstruction.
References
1. Am J Sports Med. 2000; 28:472-479
2. J Bone Joint Surg Am. 2009;91:263-273
3. Clin J Sport Med. 2005; 15:62-66.
4. Acta Orthop. 2005; 76:699-704.
5. Arthroscopy. 2008;24(8):881-887.
6. Arthroscopy. 2015;31(6):1207–15.27.
7. Am J Sports Med. 2008;36:2301-2309.
8. Acta Orthop Scand. 1997;68:419-423.
9. Cochrane Database Syst Rev.
2011;(11):CD008106.26.
10. J Bone Joint Surg Am. 2008;90:463-470.
11. Am J Sports Med. 2004;32:1114-1121.
12. Am J Sports Med. 1997;25:213-217.
13. Am J Sports Med. 1999; 27:350–353
14. Am J Knee Surg. 2000; 13:137–142
15. J Magn Reson Imaging. 1994 4:590–594
16. Phys Ther. 1998; 78. 25–32
17. Sports Med Arthrosc Rev. 2007; 15:95–104
18. International Orthopaedics (SICOT) (2012)
36:2447–2456
19. Clin Orthop. 1993; 179:183–188
20. Arthroscopy. 1987; 3:269–272
21. Ital J Orthop Traumatol. 1992; 18:25–36
22. Sports Med Arthrosc Rev. 2007; 12:57–60
23. Arthroscopy. 2007; 23:463–468
24. Clinical Sports Med. 2003; 21(3); 499-519.
25. Arthroscopy. 2002; 18(1):E2
26. Am J Sports Med. 2005; 33:220–230
27. Arthroscopy. 1993; 9:63–67
28. Arthroscopy. 2006; 22:166–171
29. Am J Sports Med. 1998; 26:59–65
30. Am J Sports Med. 2007; 35(11):1851–1858
31. Knee. 2000; 7:121–127
32. Arthroscopy. 2006; 22:787– 79
33. Am J Sport Med. 2011; 39(1):140–145
34. Knee Surg Sports Traumatol Arthroscopy.
2005; 13:522–528
35. Rev Chir Orthop. 1964; 50:813–824
36. Arthroscopy. 2008; 24(1):77–81 8
37. Am J Sport Med. 2005; 33:1220–1223
38. Am J Sports Med. 1982; 10:303–310
39. J Bone J Surg Br. 2002; 84:861–864
40. Sports Med Arthosc Rev. 2007; 15:61–6
41. Rev Chir Orthop Reparatrice Appar Mot.
2002; 88(7):678–685
42. Rev Chir Orthop Reparatrice Appar Mot.
1990;76:45-54
43. Knee Surg Sports Traumatol Arthrosc.
2005; 13:529–533
44. J Am Ac Orthop Surg. 2011; 19(1):8–16
45. J Bone J Surg Br. 2006; 88(10):1331–1335




