Chiropractor, Dr. Alexander Jimenez takes a look at the anatomy and biomechanics of the adductor magnus, its role in musculoskeletal syndromes and how clinicians can manage tightness and high tone in this muscle.
The adductor magnus (AM) is a posteromedial thigh muscle, with a complex anatomical arrangement. It has a number of primary roles, including functioning as a major hip extensor, hip adductor and pelvic stabiliser. The role AM has in producing movement at the hip and pelvis is often misunderstood and underrated. It plays a fundamental role in producing hip extension force when the hip is already in hip flexion. As a result it is commonly found to be tight and overactive in many athletes potentially leading to a host of musculoskeletal issues.
Anatomy
The AM is located on the medial side and posterior side of the thigh. It has been suggested that it should be considered as having three separate anatomical and functional components (figure 1 shows the relative origins of the three heads along with the hamstring muscle group):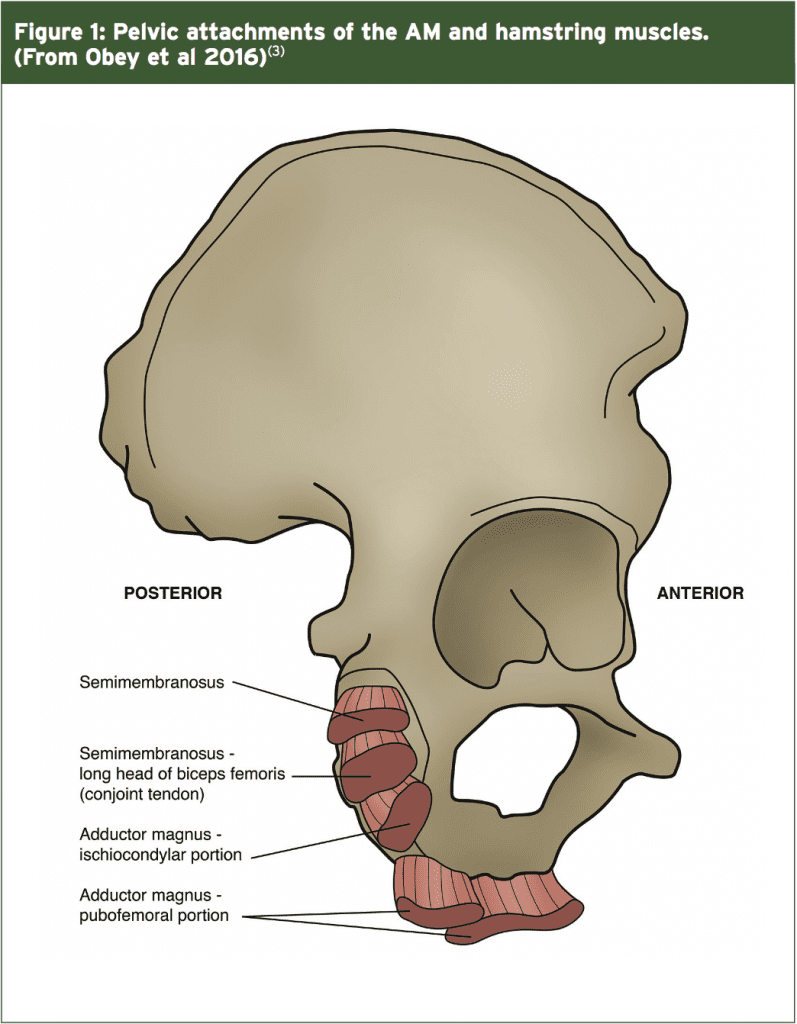
1. Pubofemoral portion or ‘adductor minimus’
a. The front or anterior part of the muscle, arising from the ischiopubic ramus (where the ramus of both pubic bone and ischium meet).
b. Fibres from the pubic ramus are short and horizontal, and insert along the linea aspera just medial to the gluteus maximus.
c. This is the hip flexing and adducting part of the AM.
2. Middle part
a. The fibres from the ischial ramus are more vertical and lateral, and these insert via an aponeurosis into the linea aspera, being innervated by the posterior branch of the obturator nerve(1).
b. This is the adducting component of the AM.
3. Ischiocondylar portion or ‘hamstring portion’
a. This is the posterior part of the muscle.
b. Due to the common nerve supply (sciatic nerve) between this portion and the hamstrings, it is often grouped together with the hamstrings as a hip extensor (sometimes called the ‘4th hamstring’(1)).
c. It arises out of the ischial tuberosity, from a well-defined osseous origin located medial to the semimembranosus and conjoint tendons(2).
d. Fibres run vertically downwards as a thick and fleshy mass of coarse bundles, and insert onto the adductor tubercle via a rounded tendon.
e. This is the hip extending part of the AM.
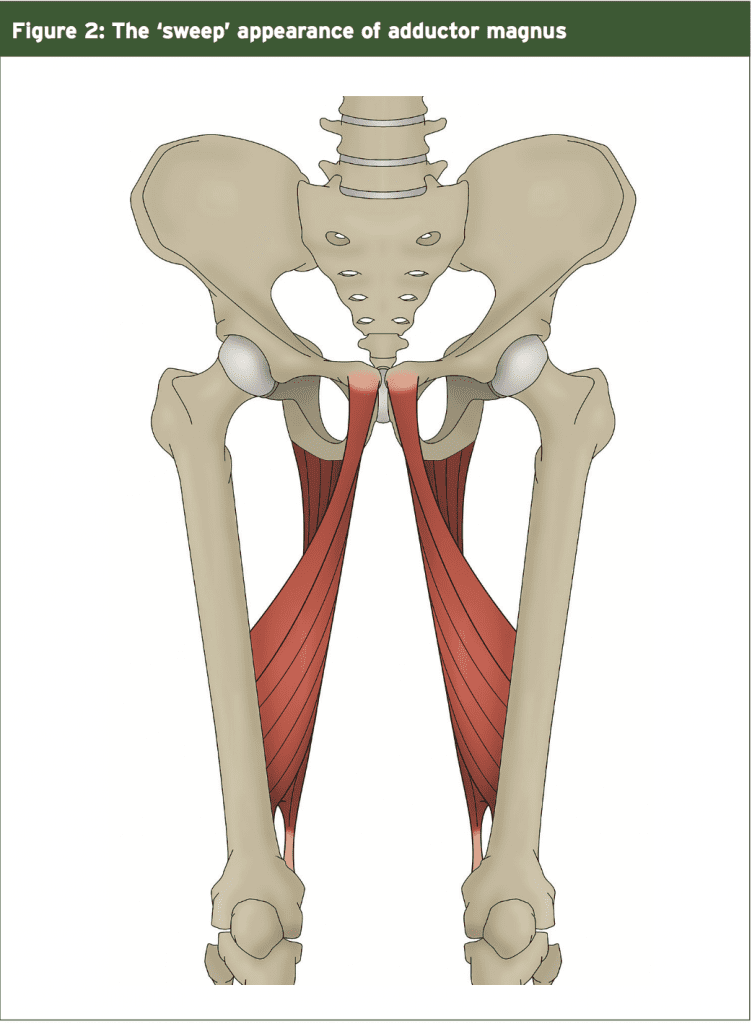
Due to the complex pelvic attachment of the AM, the variable insertion points along the femur, and the geometrical rotation through the shaft of the femur, the AM has a sweep or curved appearance as it descends down the inner thigh to insert along the linea aspera and finally the adductor tubercle. This structure allows it to act as a major stabiliser of the pelvis as we hip flex in weight bearing – eg squatting down and bending over to pick up something.
It could be postulated that due to the fact the ischiocondylar (posterior) part of the AM does not cross the knee joint, it is a muscle that can be used to not only control the hip and pelvis as we flex the hip under load (such as squatting and bending over) but which may also be used to stabilise the hip and pelvis. This is because the bi-articular hamstring muscles are influenced by the concurrent knee flexion that may occur during squatting, and can lose their ‘length tension curve’ to control and maintain hip flexion moments. The AM on the other hand is better suited to doing this (along with the gluteals). Considering the role of the AM in comparison to the other hip extensors such as gluteals and hamstrings therefore, the AM is often underrated in its influence in producing movement, and acting as a hip and pelvic stabiliser.
AM Physiology
The AM is one of the largest muscles in the body (based purely on weight and volume).
It appears to be the second heaviest muscle in the lower limb after the gluteus maximus. Ito et al. (2003) found that the gluteusmaximusandAMweighed573.4g and 452.6g respectively(4). Similarly, by reference to cross-sectional area, it is the second largest muscle after the gluteus maximus; the same researchers found that the gluteus maximus and AM were 48.4cm2 and 26.9cm2 in cross-sectional area, respectively(4). Based on muscle volume, AM is also much larger than the other adductor muscles such as adductor brevis, adductor longus, pectineus and gracilis(5).
The AM, adductor longus, adductor brevis, gracilis all have substantial hip-adduction muscle-moment arms. The ischiocondylar AM has a large hip extensor muscle-moment arm, making it an unappreciated hip extensor, while the other adductors are hip flexors. The hip-extension moment arm length of the AM changes with hip angle; it is a more effective hip extensor than either the hamstrings or gluteus maximus when the hip is flexed. This means that exercises that have peak contractions in positions of hip flexion (like full squats) can train the AM very effectively.
The AM, adductor longus, adductor brevis, gracilis all have substantial hip-adduction muscle-moment arms. The ischiocondylar AM has a large hip extensor muscle-moment arm, making it an unappreciated hip extensor, while the other adductors are hip flexors. The hip-extension moment arm length of the AM changes with hip angle; it is a more effective hip extensor than either the hamstrings or gluteus maximus when the hip is flexed. This means that exercises that have peak contractions in positions of hip flexion (like full squats) can train the AM very effectively.
It has been reported that the AM muscle moment arm length for hip extension was 5.7 – 6.1cm at 90 degrees of hip flexion, compared to 4.0 – 4.8cm for the hamstrings, and 3.1 – 3.3cm for the gluteus maximus(6). This makes the AM the most effective hip extensor in hip flexion, which corresponds to the bottom of the squat movement. In strength and conditioning circles, this deep position is known as ‘getting out of the hole’. The AM produces a large part of the hip extension torque in this deep position. Anecdotally, many deep squatters appreciate this the day after a heavy squat session as the most ‘sore’ muscle the next day due to delayed onset muscle soreness (DOMS) is the AM!
In contrast, the AM is only a moderate hip extensor when the hip is already extended. Németh and Ohlsén reported that the AM muscle-moment arm length for hip extension was just 1.5 – 2.4cm in the anatomical position, compared to 6.1 – 6.8cm for the hamstrings, and 7.5 – 8.1cm for the gluteus maximus(6) Meanwhile Dostal et al. reported muscle-moment arm lengths of 3.9cm and 5.8cm for the middle and posterior portions, respectively(7). This makes the hamstrings and gluteus maximus much more effective hip extensors than the AM when the hip is extended, as in the upright position.
These above findings have implications for the athlete – and also the therapist managing injuries – related to the balance of the hip extensor muscles. The ischiocondylar AM would be an extremely strong and possibly dominant muscle is the following examples:
- Sprint starts out of the blocks. They become less important as the sprinter approaches a vertical position.
- Sprint cyclists who assume a curled position of extreme hip flexion.
- Powerlifters, weightlifters or any strength athlete at the start of a deadlift/ clean and jerk movement, or getting ‘out of the hole’ in squatting.
- Hockey players spend a long time in hip flexion positions.
- American football and rugby players. Drive in contact starting from a position of hip flexion.
- Cross fit athletes who perform many movements from deep hip flexion.
- Uphill running and stepping up.
The muscle moment arms for the AM in adduction exceed those of hip extension, showing that this muscle is still definitively a hip adductor as well as a hip extensor(7). The AM does not display a large muscle-moment arm length in the transverse plane, and therefore does not contribute a lot to hip internal or external rotation(7-10).
In terms of muscle fibre characteristics, the AM is composed of mixed type 1 and type 2 muscle fibres. This compares with the other hip extensors such as the hamstrings that have higher numbers of type 2 fibres(11,12). The clinical consequence is that the AM is great at producing slow- strength based movements such as heavy deep squats, whereas in faster hip extension movements such as sprinting, the hamstrings have a favourable fibre type for this type of activity. Therefore to summarise the functional roles of the AM:
1. It is a powerful hip extensor at full hip flexion positions.
2. Its role in hip extension reduces as the hip approaches neutral positions.
3. It is an adductor of the hip.
4. It stabilises the hip and pelvis in hip flexion positions such as squatting down and bending forward.
AM In Musculoskeletal Dysfunction
Compared to other muscles such as the vastus medialis obliquus (VMO), lower and upper trapezius, gluteus medius and transversus abdominus, the research available on the role the AM plays in musculoskeletal dysfunction is sparse and almost non-existent. This may be due to the fact that is a thick and very deep muscle, has a complex anatomical arrangement, and EMG studies may be difficult due to cross talk from neighbour muscles such as the hamstrings and other adductors.Clinically and anecdotally however, it can be postulated that the AM is muscle that is often over-used and develops myofascial restrictions, trigger points and tightness – especially in athletes. Due to the heavy use of the ischiocondylar part of the AM in producing hip extension force from hip flexion positions, it could be argued that athletes may develop imbalances in these muscle groups due to the over reliance on AM to produce movement.
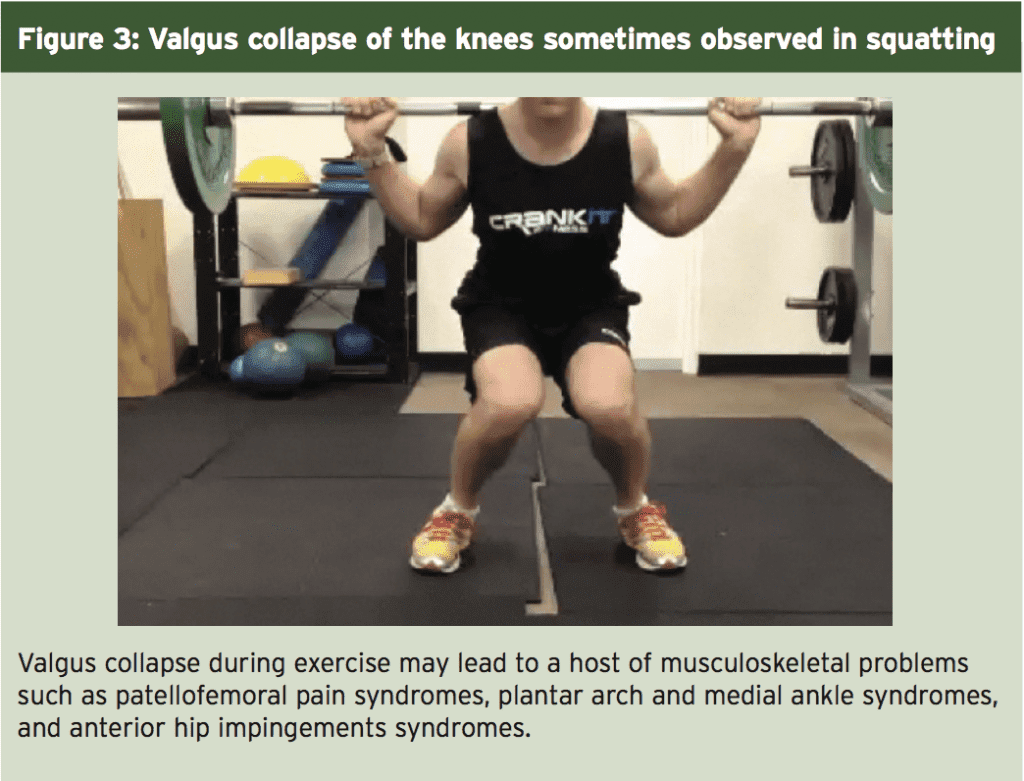
The use of the AM to produce hip extension torque would have a significant effect on the lower limb kinematics during such movements. This can sometimes be seen in heavy lifting movements with powerlifters and weightlifters, where the knees medially deviate on the initial part of the ascent during the deep squat. This is often referred to as a ‘valgus collapse’ of the knees.
It is thought that this movement is produced by the adduction component of the AM, and is not balanced by the abducting component of the gluteus maximus during the hip drive/extension phase in deep squatting movements. This can be seen in Figure 3. It must be mentioned here that this appearance of valgus collapse is also caused by other factors such as reduced ankle dorsiflexion and other hip muscle imbalances. However, if the knees appear to be aligned over the third toe during the descent of the squat, and then on the change over from eccentric to concentric muscle action a valgus collapse occurs, it may well be likely that the valgus collapse has been initiated by a hip extension muscle with an additional adduction role – ie the AM.
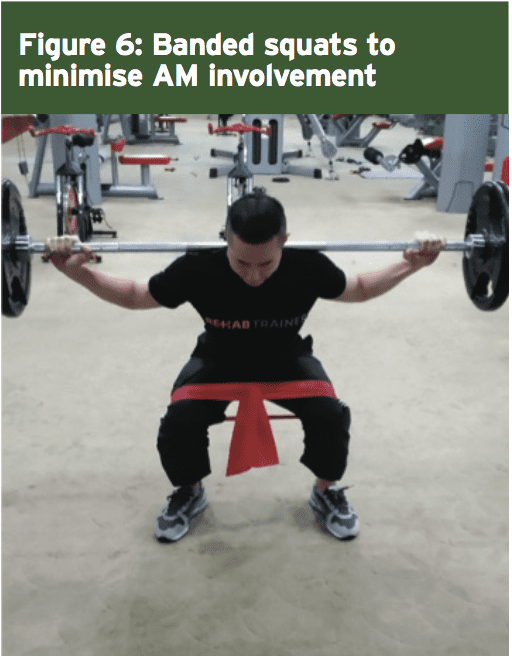
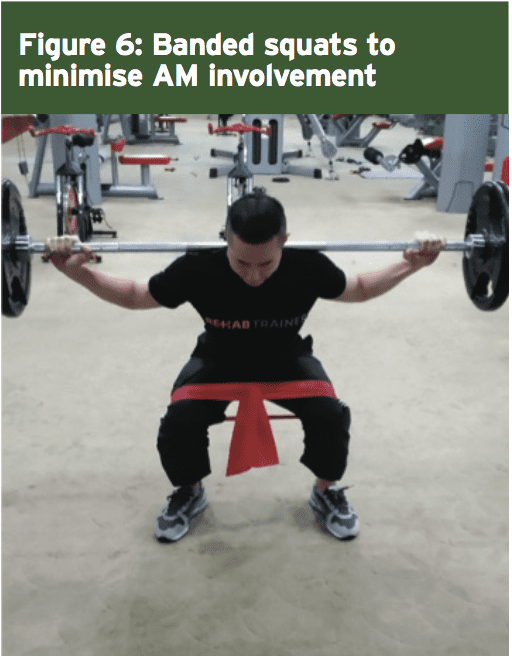
By using an elastic band or strap around the knees during squatting and asking the lifter to actively push out against the strap would in effect require the hip abducting gluteals to perform this action. This may reduce the tendency for the AM to over dominate during the squat movement and create unwanted hip adduction and valgus knee collapse. This exercise can be done in a periodised training cycle (such as in the early general preparation phases) or it may be done as warm up before performing heavy squat movements.
References
1. Martini F, Timmons M, Tallitsch R. Human Anatomy. Boston, MA: Pearson Benjamin Cummings; 2012.
2. Skeletal Radiol. [published online November 10, 2015]. doi:10.1007/ s00256-015-2291-5
Managing AM Tightness
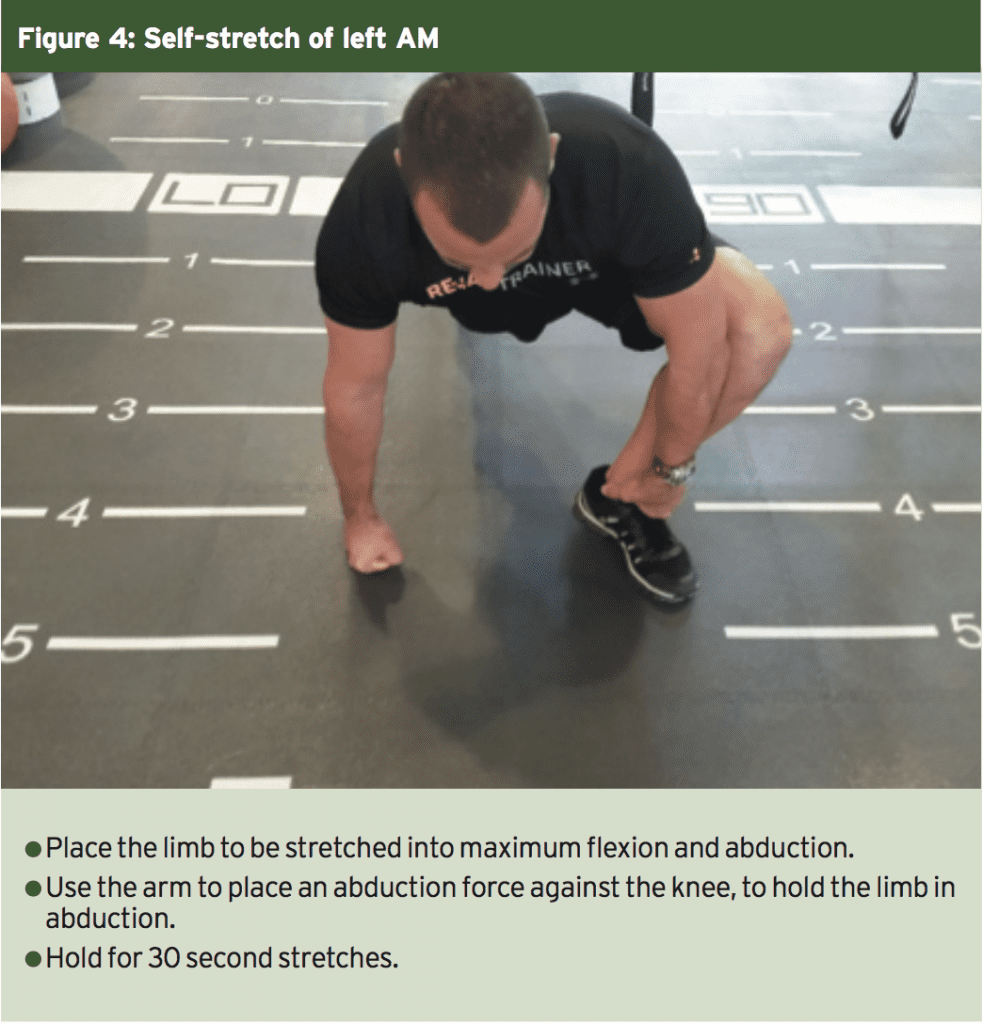
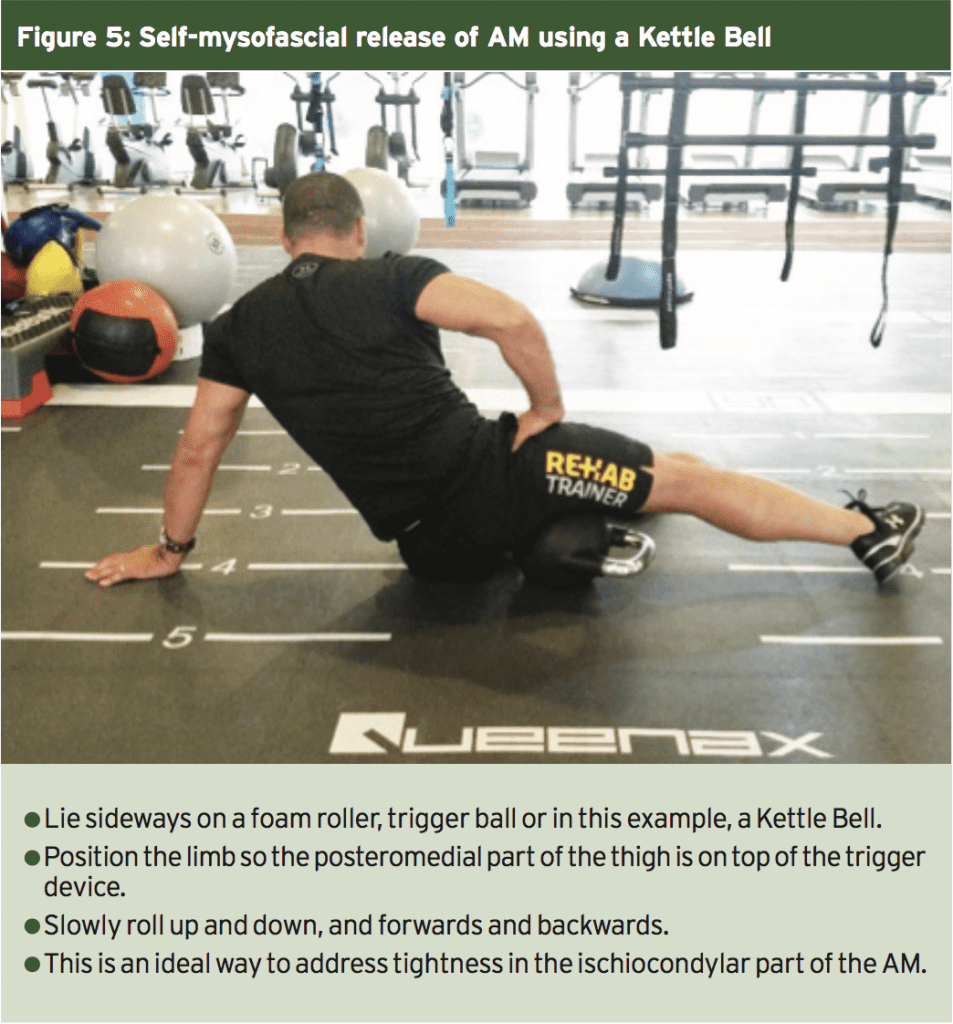
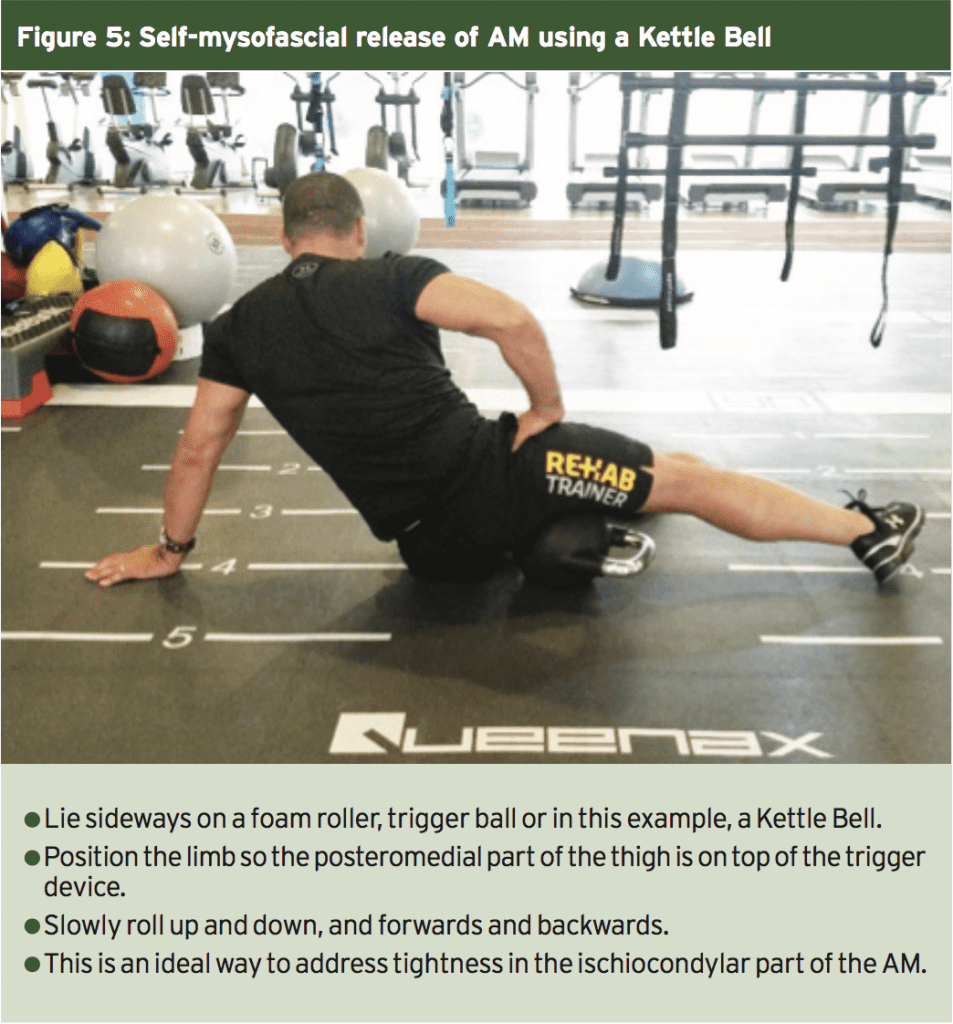
Considering that the AM is often ‘overactive’ in most athletes, it may be argued that it is a muscle that does not need a lot of direct strengthening. It may be more appropriate to stretch and perform myofascial release techniques to the muscle. Below are two examples of how this can be performed.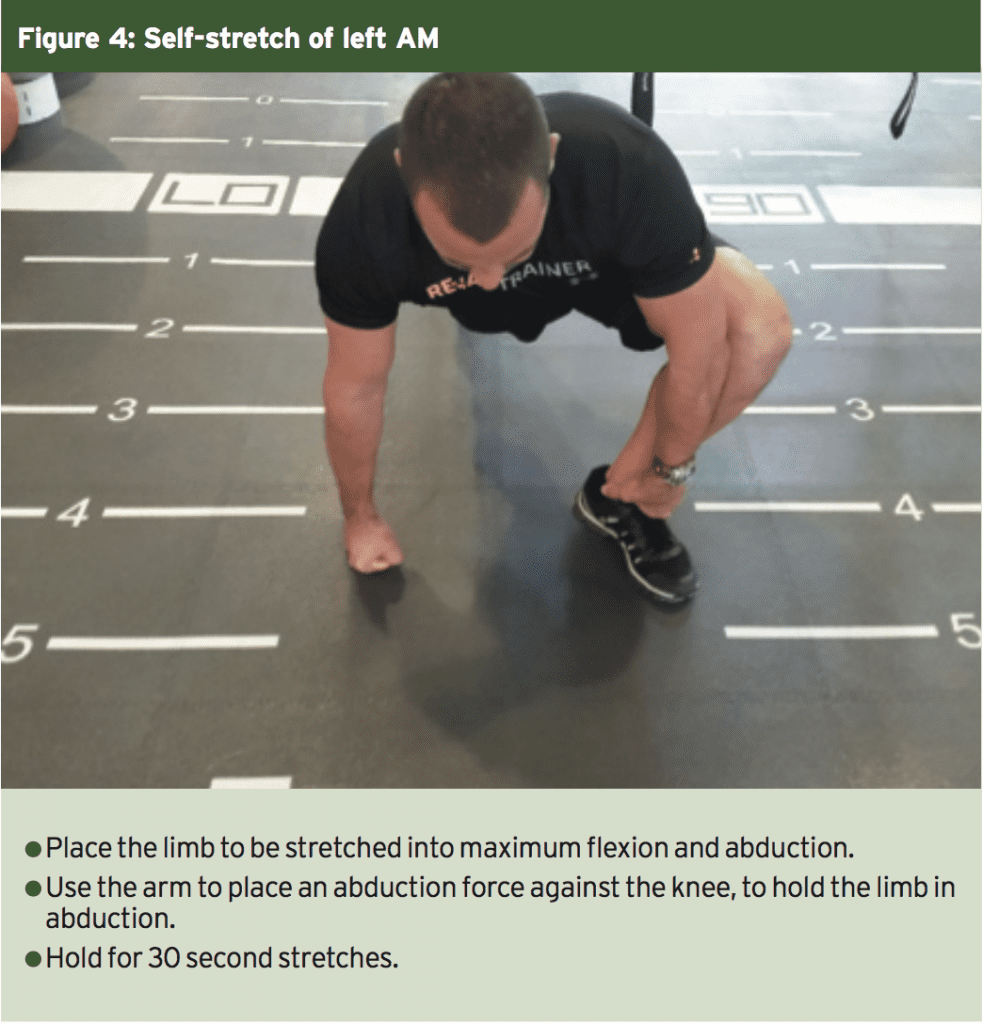
Minimising AM Involvement In Squatting
To minimise involvement, it may be necessary to integrate more gluteus maximus into the squat movement via the use of bands and straps around the knees when squatting. This is a technique made popular by a wide variety of strength and conditioning coaches around the world such as Louie Simmonds and the Westside Barbell Company in the USA.By using an elastic band or strap around the knees during squatting and asking the lifter to actively push out against the strap would in effect require the hip abducting gluteals to perform this action. This may reduce the tendency for the AM to over dominate during the squat movement and create unwanted hip adduction and valgus knee collapse. This exercise can be done in a periodised training cycle (such as in the early general preparation phases) or it may be done as warm up before performing heavy squat movements.
Summary
The AM is a complex muscle that has wide anatomical attachments onto both the pelvis and femur. It has a major role in producing hip extension force from positions of deep flexion, and also adduction in all hip angle positions. AM is often overactive on athletes and thus is a muscle that needs a lot of direct stretching and myofascial release techniques to avoid possible knee and hip joint issues.References
1. Martini F, Timmons M, Tallitsch R. Human Anatomy. Boston, MA: Pearson Benjamin Cummings; 2012.
2. Skeletal Radiol. [published online November 10, 2015]. doi:10.1007/ s00256-015-2291-5
3. The Orthopaedic Journal of Sports Medicine. 2016. 4(1)
4. Okajimas folia anatomica Japonica. 2003. 80(2-3), 47
5. Journal of Applied Physiology. 2012. 113(10), 1545-1559
6. Journal of Biomechanics. 1985. 18(2), 129-140 7. Physical Therapy. 1986. 66(3), 351-359
8. Medical Engineering & Physics. 1998. 20(1), 50-56
9. Gait & Posture. 2000. 11(3), 181-190
10. Journal of Biomechanics. 2001. 34(4), 437-44
11. The American Journal of Sports Medicine. 1984. 12(2), 98-103
12. Archives of Physical Medicine and Rehabilitation. 2004. 85(4), 593
4. Okajimas folia anatomica Japonica. 2003. 80(2-3), 47
5. Journal of Applied Physiology. 2012. 113(10), 1545-1559
6. Journal of Biomechanics. 1985. 18(2), 129-140 7. Physical Therapy. 1986. 66(3), 351-359
8. Medical Engineering & Physics. 1998. 20(1), 50-56
9. Gait & Posture. 2000. 11(3), 181-190
10. Journal of Biomechanics. 2001. 34(4), 437-44
11. The American Journal of Sports Medicine. 1984. 12(2), 98-103
12. Archives of Physical Medicine and Rehabilitation. 2004. 85(4), 593




