It has been stated that lateral ankle sprains in athletes are one of the most common injuries suffered in training and competition, accounting for a large amount of time away from competition(1,2). Also, its prevalence as a joint injury may be as high as 20% of all joint injuries suffered by athletes(3).
Most ankle sprains tend to recover well to a functional level with conservative rehabilitation. However, a number of acute ankle sprain sufferers may go on to develop later-stage chronic or recurrent ankle instability, with a feeling of ‘vulnerable ankles’, episodes of catching and ongoing pain – and further episodes of repeat ankle sprains(4). Of further significance is that ankle sprains have a high rate of recurrence (as high as 80% in high-risk sports)(5,6). This suggests that many ankle sprain sufferers will most likely sprain their ankles again, and this may then cascade to late stage chronic ankle instability (CAI).
Part one of this series discussed the pathological progression from acute ankle sprain to chronic and recurrent instability, the relevant anatomy and biomechanics that are involved in this syndrome, how it may be identified in the athlete and options for management. Part two discussed in detail the surgical options available to stabilise an ankle with CAI. The argument for anatomic repair was discussed in detail. In the final part of this series, we will consider post-op rehab. In particular, the multi-stage protocol will be presented and particular reference will be made to how the programme differs for an anatomic repair (Brostrom, modified Brostrom or Gould repair) versus the non-anatomic repair (Chrisman- Snook, Colville or Evan repair).
Post-Operative Rehabilitation Protocol
As with any planned rehabilitation protocol, an understanding of the influence of load exposure, load attenuation and force generation is critical to provide a clear understanding of the milestones that need to be achieved in the post-surgical ankle, and the rate at which these milestones can be pursued. As always, the best way to approach the process is to stage the approach to high performance and load resilience using a ‘phased’ or ‘milestone- based’ strategy, with each stage feeding into the next. In keeping with the exit- criteria approach, we do not move between stages according to the passage of time, but the accomplishment of functional goals.
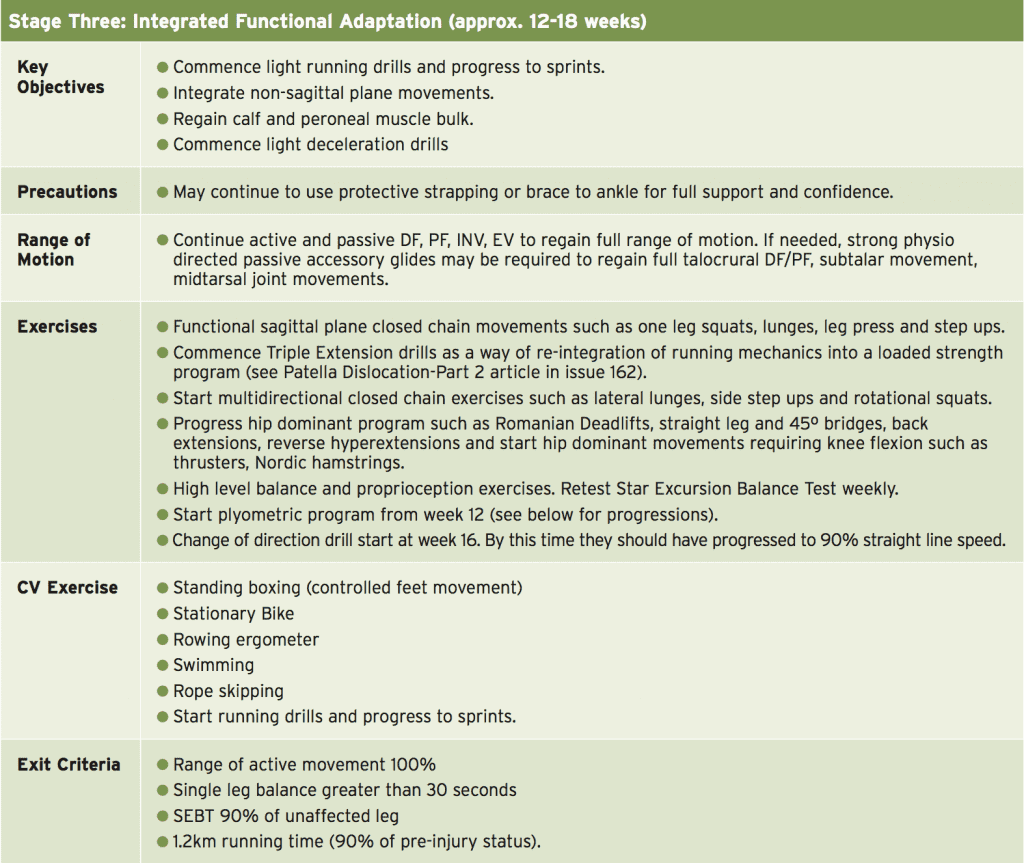
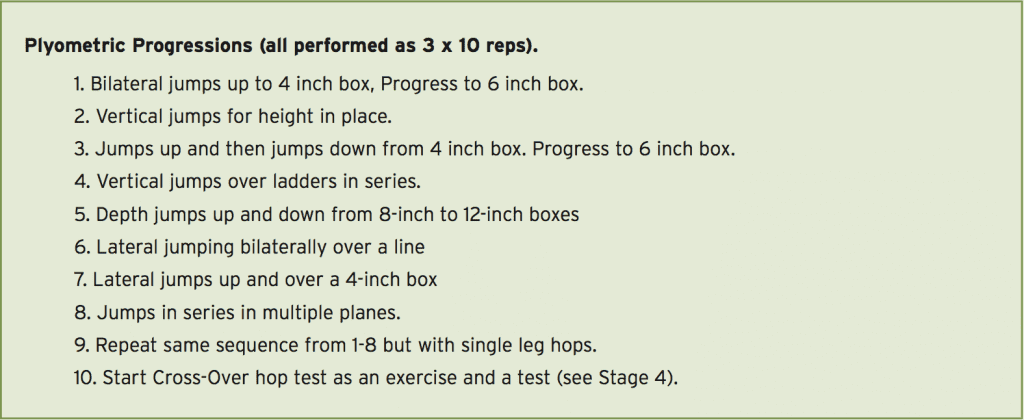
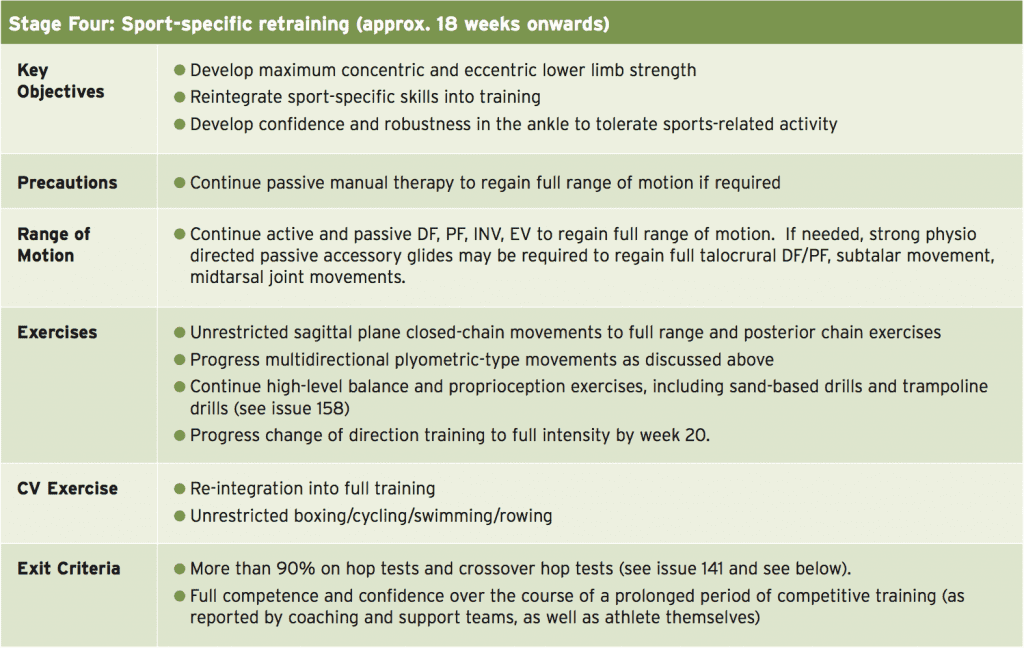
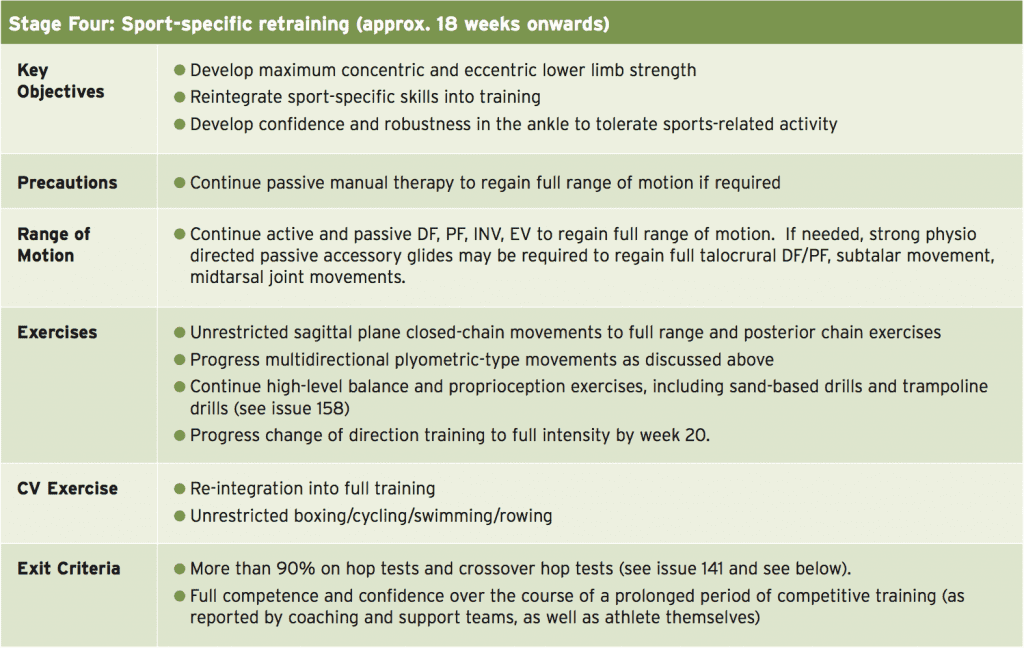
The four primary stages of ankle rehabilitation following an anatomic or non-anatomic reconstruction are:
(*) Although post-operative protocols vary with the type of repair, a standard Brostrom/Gould reconstruction is usually fully weight bearing (FWB) in Aircast Boot fixed in a neutral position for the first two weeks. During weeks 3-4 the brace is locked at 10 degrees of dorsiflexion and 20 degrees of plantar flexion. During weeks 5-6 the brace is opened to 20 degrees DF and 40 degrees of PF. At 6 weeks, the patient is FWB and allowed to mobilise without boot. However, if the patient remains tentative, it is common to maintain use of the Aircast boot when outdoors and to use an Aircast stirrup indoors.
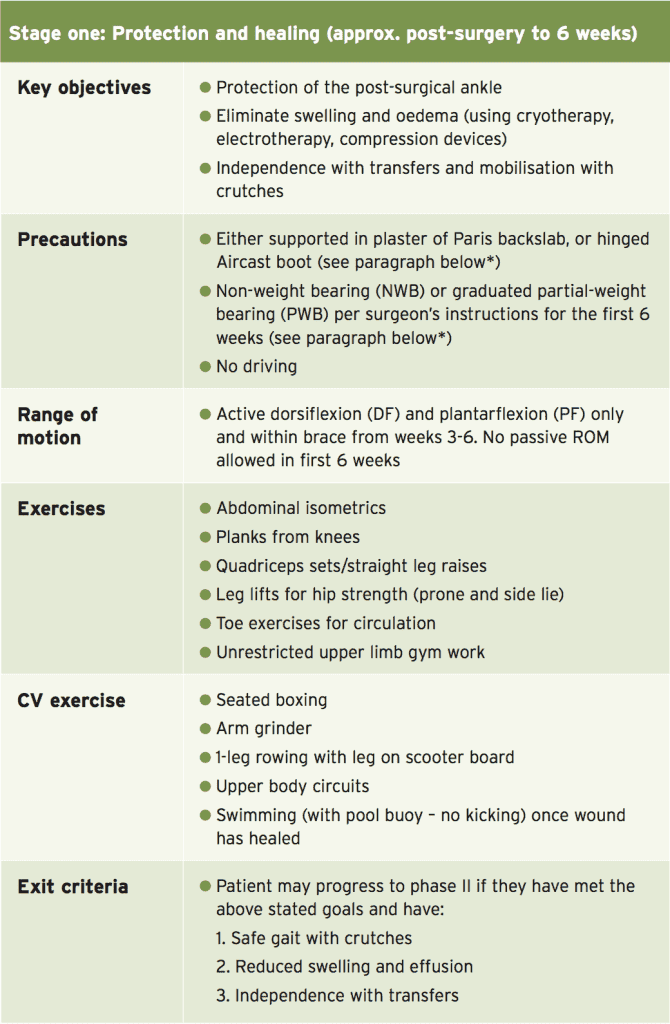
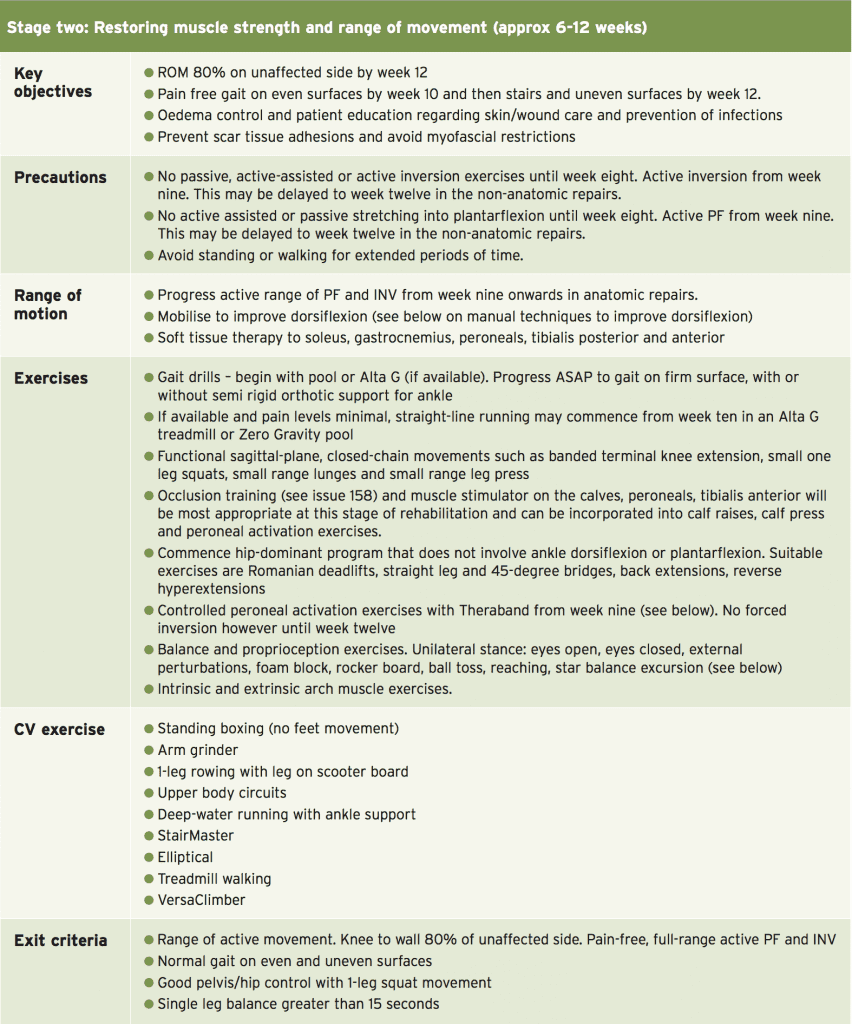
- Stage One: Protection and healing
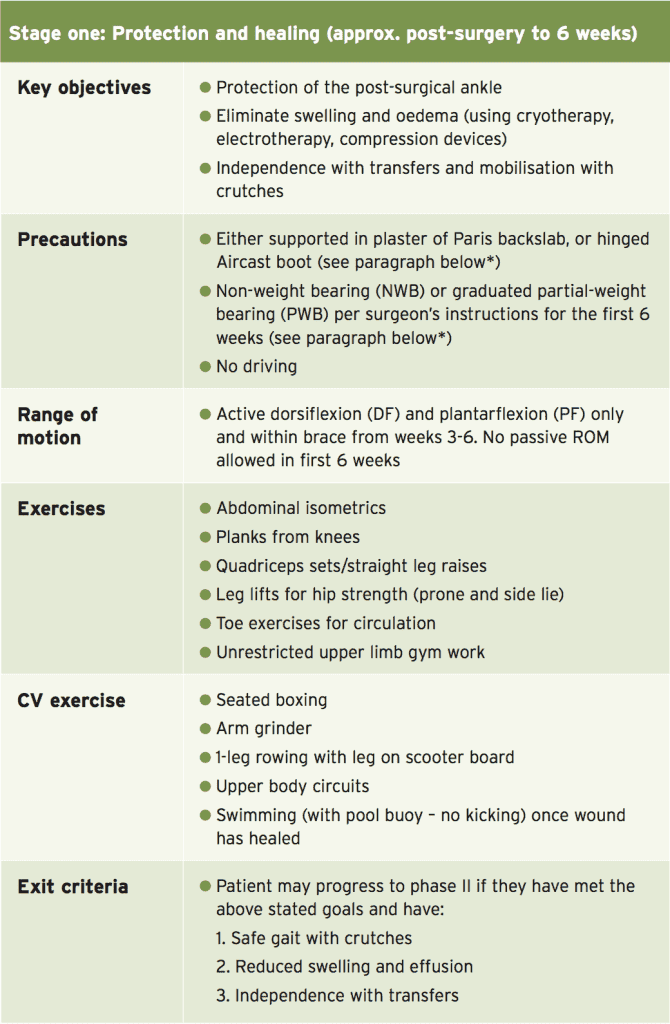
- Stage Two: Restoring muscle strength and range of movement
- Stage Three: Integrated functional adaptation
- Stage Four: Sports-specific retraining
(*) Although post-operative protocols vary with the type of repair, a standard Brostrom/Gould reconstruction is usually fully weight bearing (FWB) in Aircast Boot fixed in a neutral position for the first two weeks. During weeks 3-4 the brace is locked at 10 degrees of dorsiflexion and 20 degrees of plantar flexion. During weeks 5-6 the brace is opened to 20 degrees DF and 40 degrees of PF. At 6 weeks, the patient is FWB and allowed to mobilise without boot. However, if the patient remains tentative, it is common to maintain use of the Aircast boot when outdoors and to use an Aircast stirrup indoors.
In the non-anatomic repair, patients may be partial weight bearing (PWB) in plaster of Paris (POP) for four weeks with foot in neutral position and then full weight bearing (FWB) in POP at 4-6 weeks. Once out of POP at six weeks, they are usually transferred into an Aircast walker FWB for a 2-week period. There is no active eversion for the first six weeks. The non-anatomic repairs are typically slower to progress than anatomic repairs due to the complexity of re-routing tendons to support the lateral ankle. Note that the above protocol may be delayed and adapted if the patient has also undergone osteochondral repair (if such a defect occurs due to the nature of the CAI).
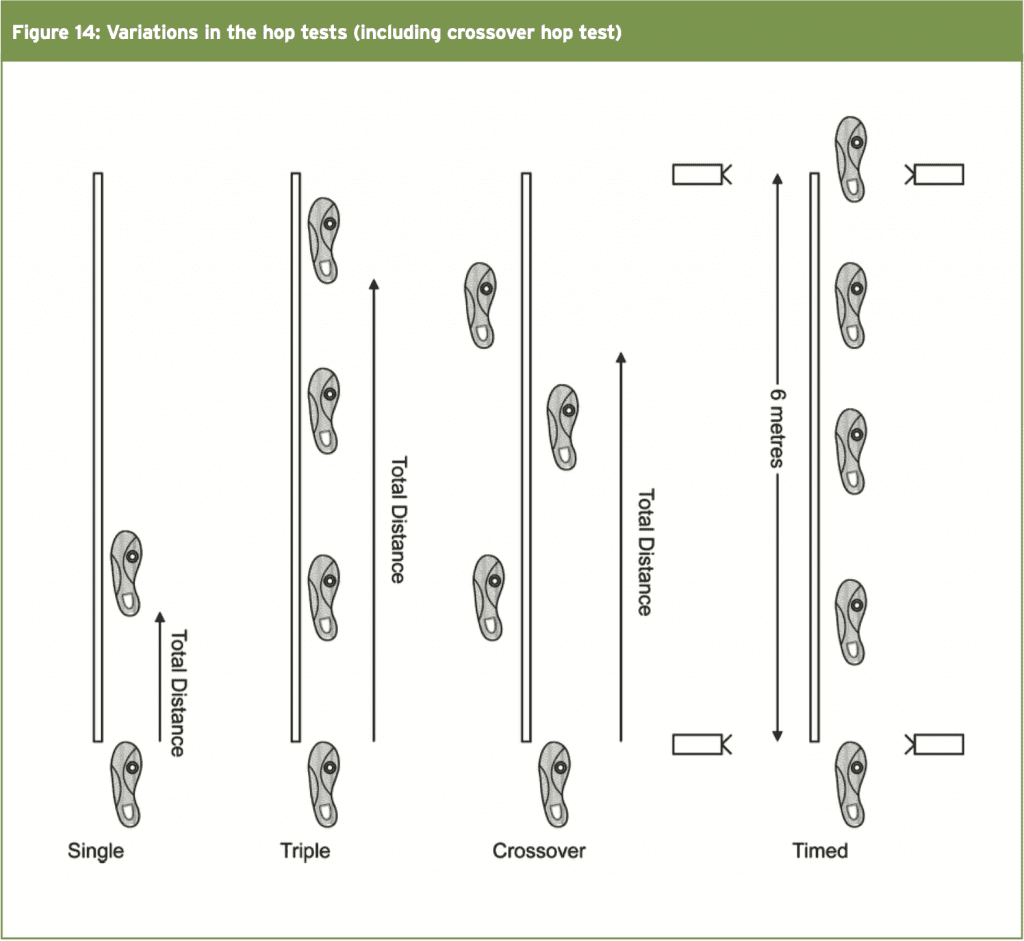
A. Distance hops: (mean involved/mean uninvolved) x 100%
B. Timed hops: (mean uninvolved/mean involved) x 100%
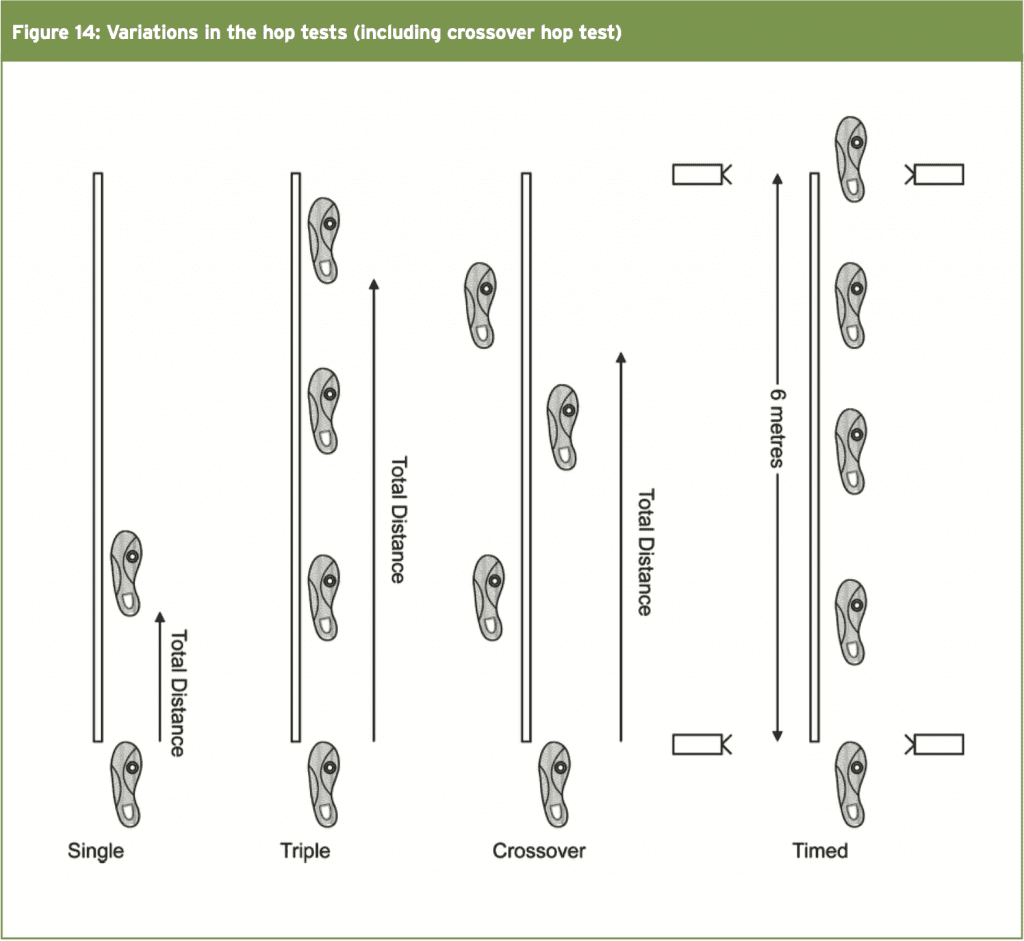
The CHT has been proven to be a reliable test for measuring the dynamic postural control in patients following knee surgery(12). It is possible to extrapolate these findings into assessment of ankle function following surgery for CAI. This test is performed by jumping over a 6-inch rectangle from a standing start followed by three impacts. The last impact needs to ‘stick’ and the athlete must not lose balance. Figure 14 shows a diagram with some variations in distance and timed hop tests. It has been accepted in post-operative knees that 87% LSI is needed to reduce risk of knee injury following surgery(12). For our purposes, the safer level of 90% LSI is used as the level the athlete needs to achieve prior to return to sport. Below is an image that shows the variations in the different hop tests including the cross over hop test.
The patho-anatomical reasons for CAI are multifactorial and relate to both anatomical deficits that lead to mechanical instability and neuromuscular changes that lead to functional instability (or perceived instability). As a result recurrent sprains may be present. Although most of these are initially managed conservatively, a percentage will fail and require subsequent ankle surgery to stabilise the lateral ankle.
Crossover Hop Test (CHT)
Hop tests are purported to more accurately test for post-operative dysfunction than double-leg jump tests as the tests are performed unilaterally and the good leg acts as a natural control leg for measurement comparison. With two-legged jump tests, the uninvolved limb may mask deficits of the involved limb (Myer et al 2011)(12). The values on hop tests are measured as the limb symmetry index (LSI), which is found by:A. Distance hops: (mean involved/mean uninvolved) x 100%
B. Timed hops: (mean uninvolved/mean involved) x 100%
The CHT has been proven to be a reliable test for measuring the dynamic postural control in patients following knee surgery(12). It is possible to extrapolate these findings into assessment of ankle function following surgery for CAI. This test is performed by jumping over a 6-inch rectangle from a standing start followed by three impacts. The last impact needs to ‘stick’ and the athlete must not lose balance. Figure 14 shows a diagram with some variations in distance and timed hop tests. It has been accepted in post-operative knees that 87% LSI is needed to reduce risk of knee injury following surgery(12). For our purposes, the safer level of 90% LSI is used as the level the athlete needs to achieve prior to return to sport. Below is an image that shows the variations in the different hop tests including the cross over hop test.
Conclusion
Ankle sprains and the possible late-stage outcome of CAI continues to be an area of interest in sports medicine. Ankle sprains are common among physically active individuals, particularly those who participate in court and team sports. Re-injury is also problematic in those engaging in high-risk sports, and this may lead to CAI.The patho-anatomical reasons for CAI are multifactorial and relate to both anatomical deficits that lead to mechanical instability and neuromuscular changes that lead to functional instability (or perceived instability). As a result recurrent sprains may be present. Although most of these are initially managed conservatively, a percentage will fail and require subsequent ankle surgery to stabilise the lateral ankle.
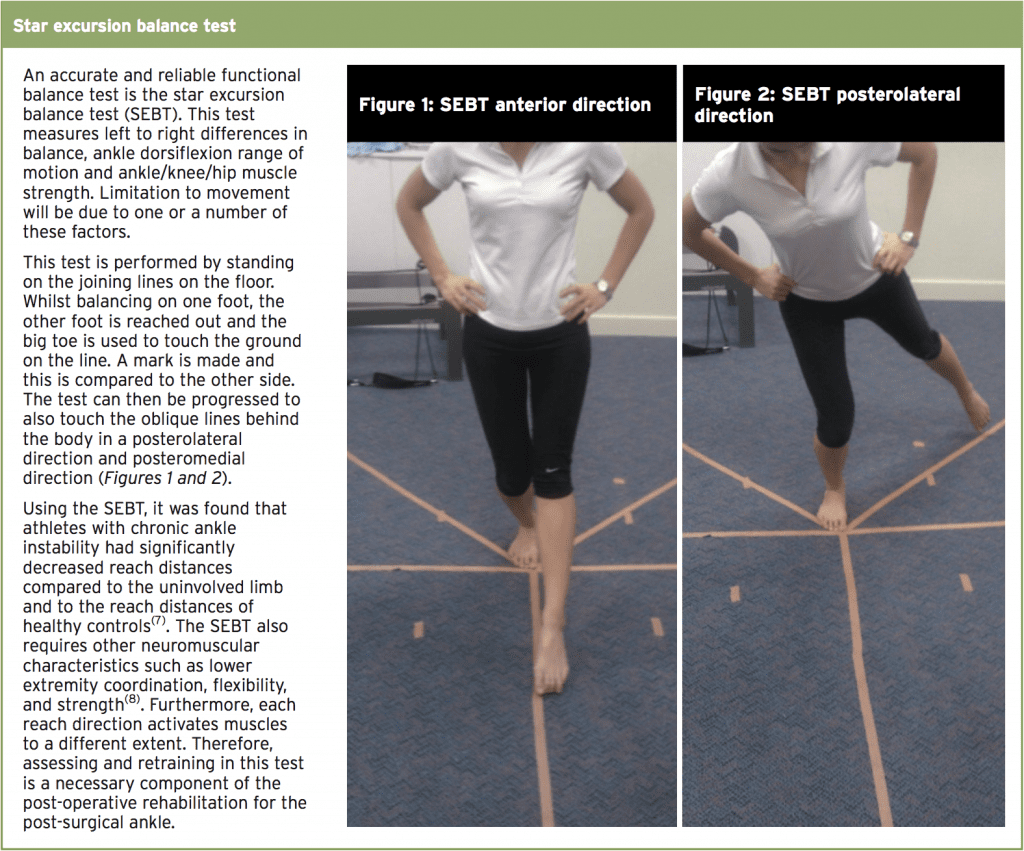
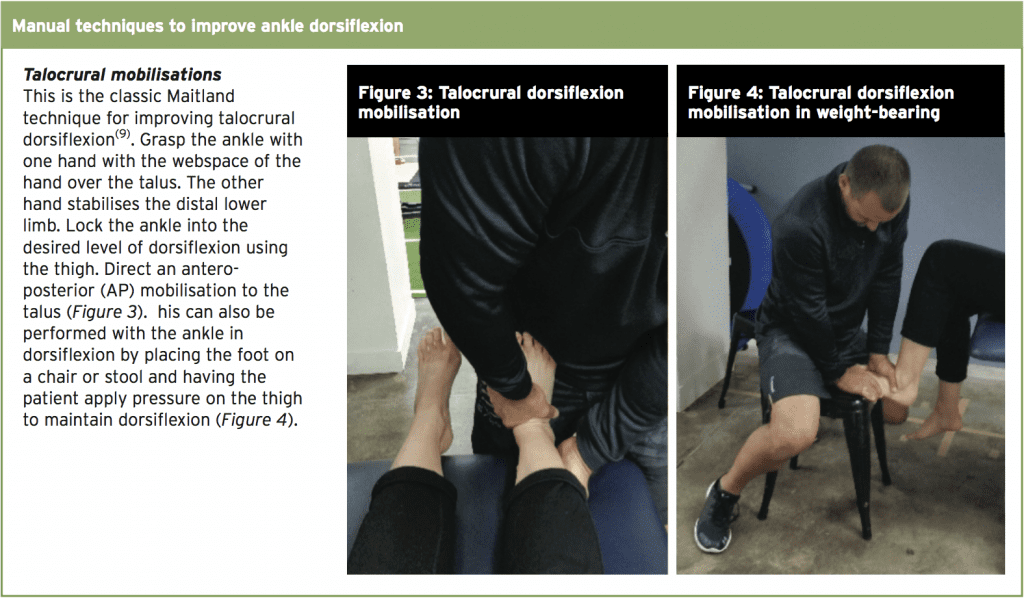
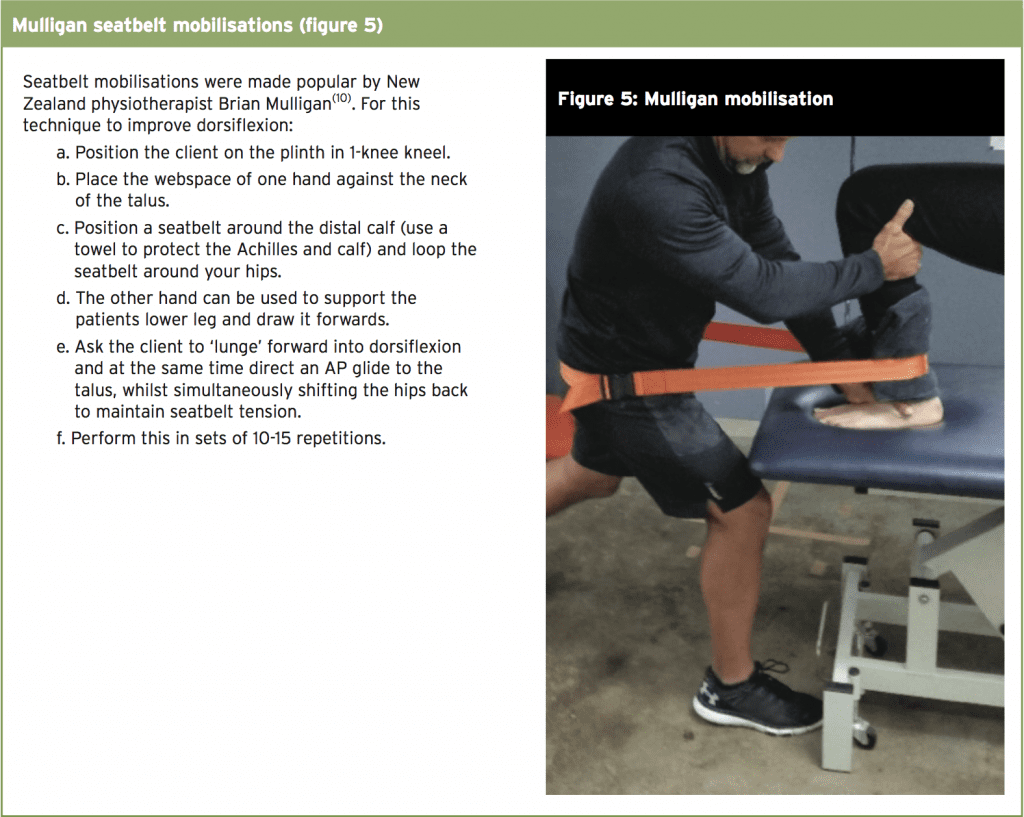
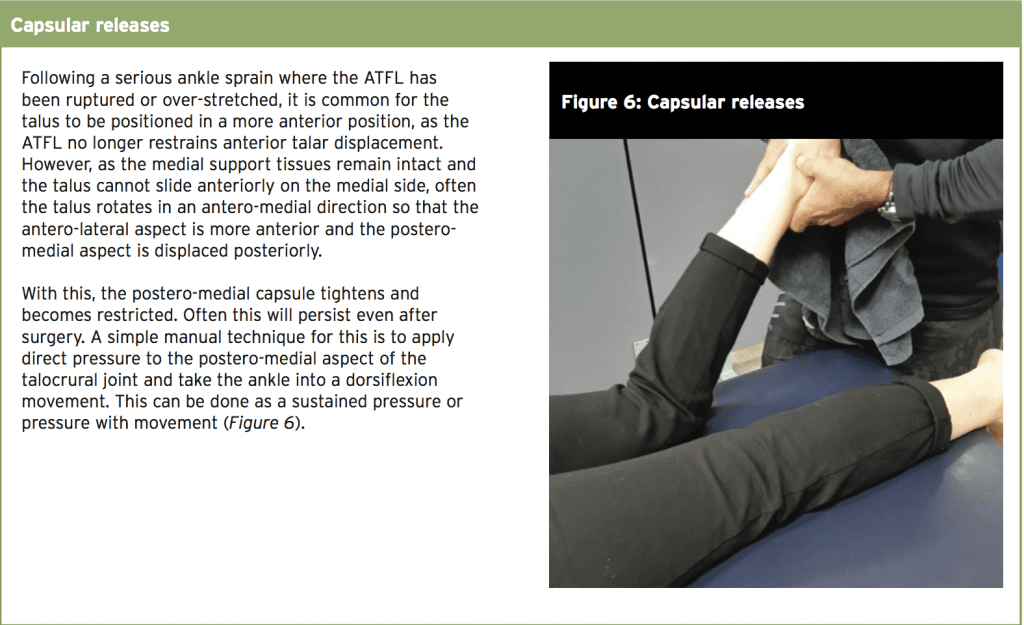
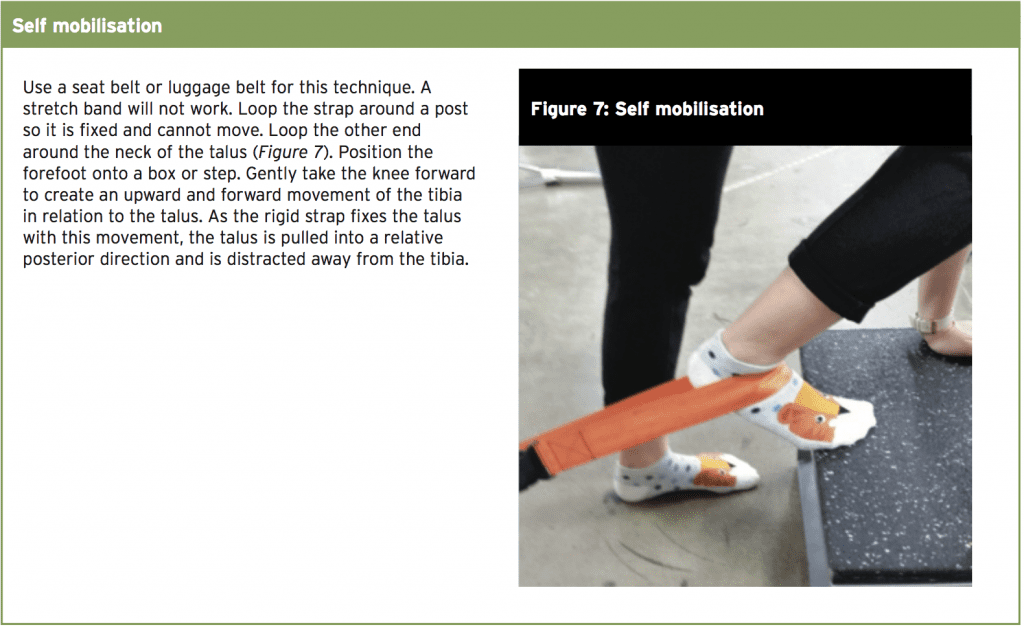
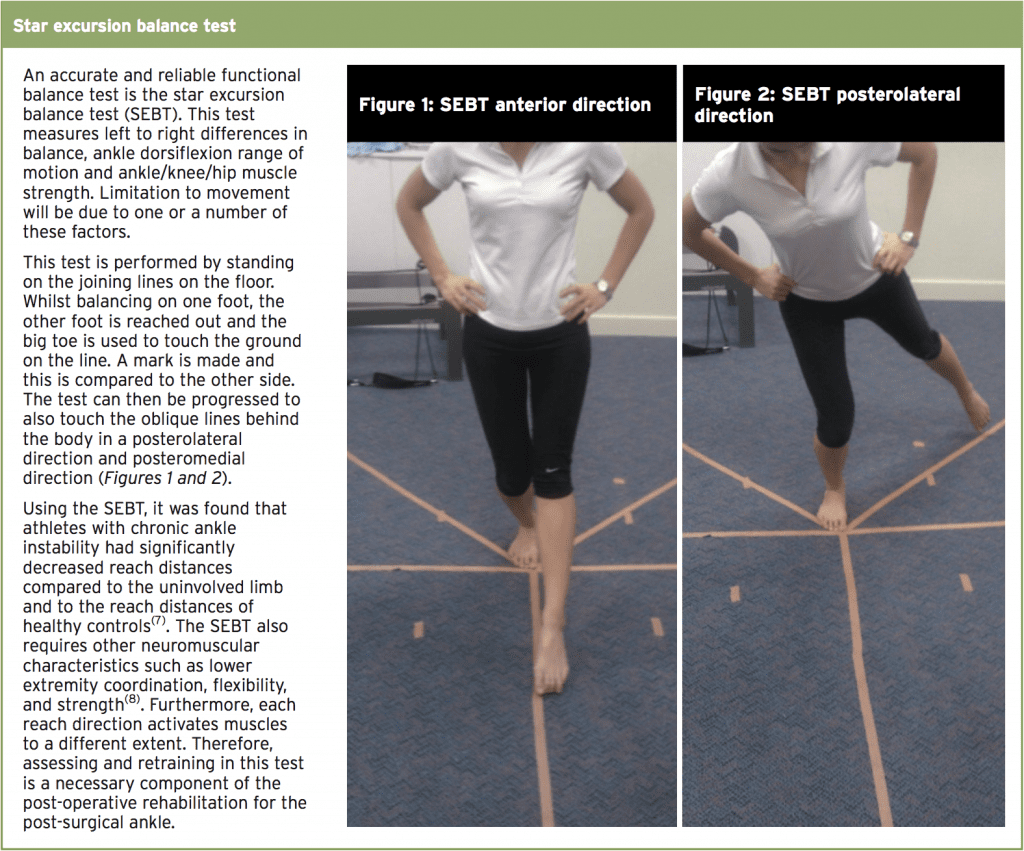
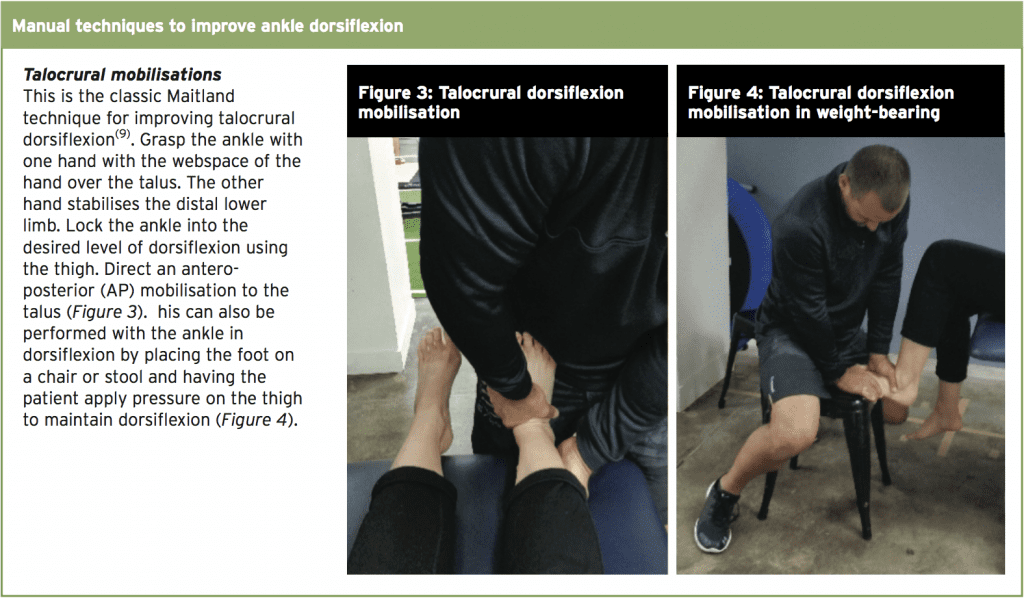
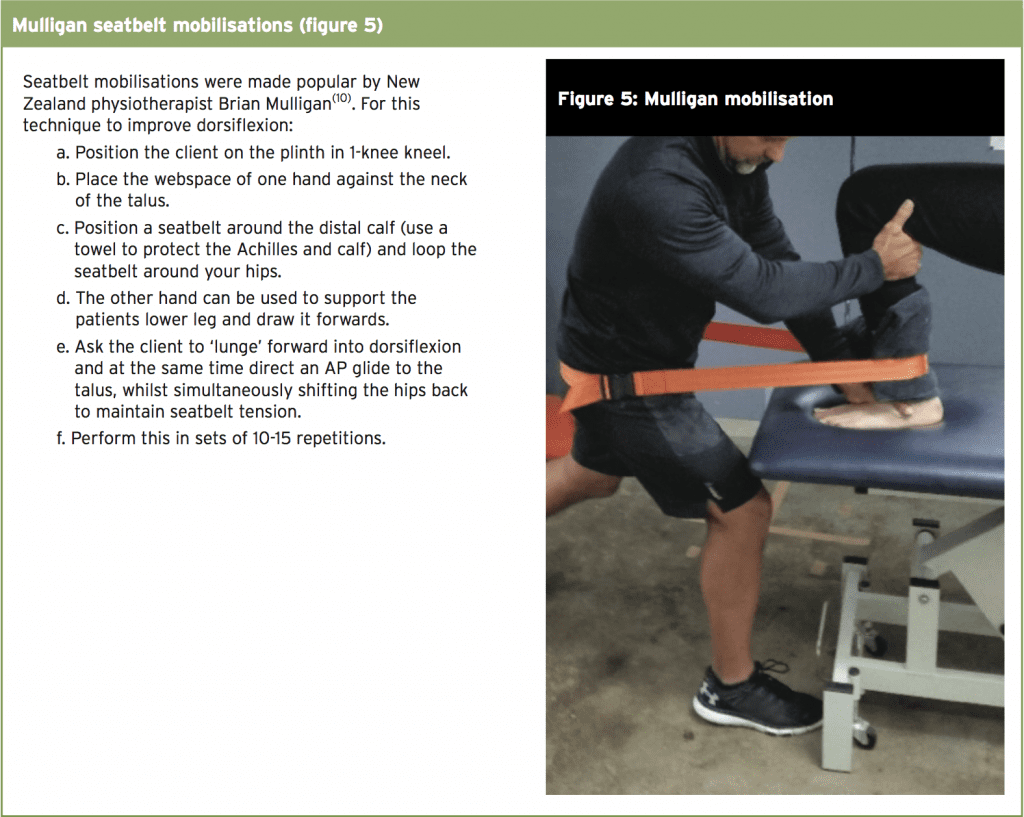
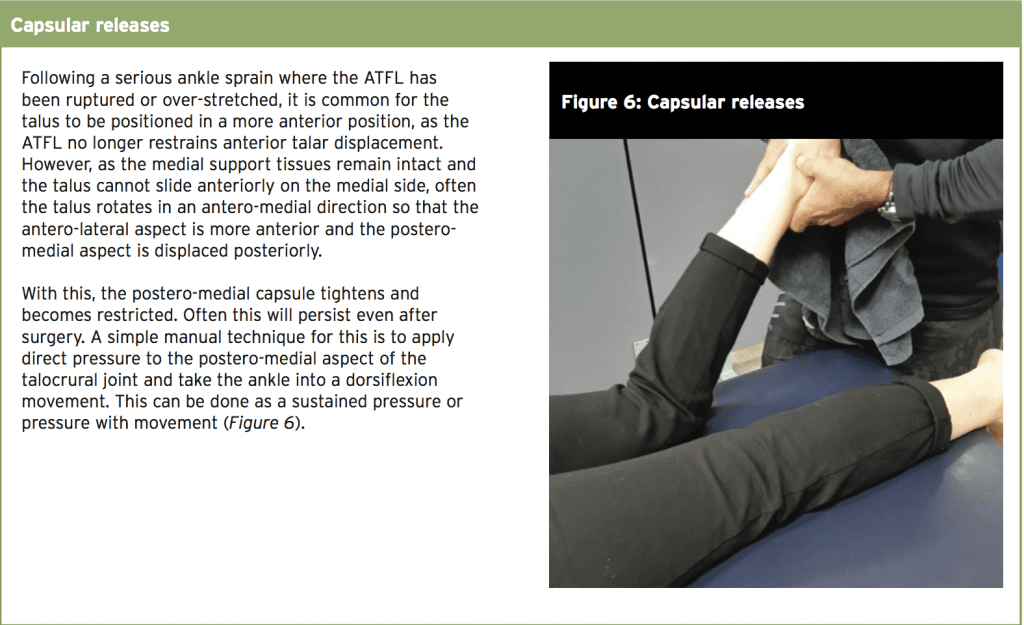
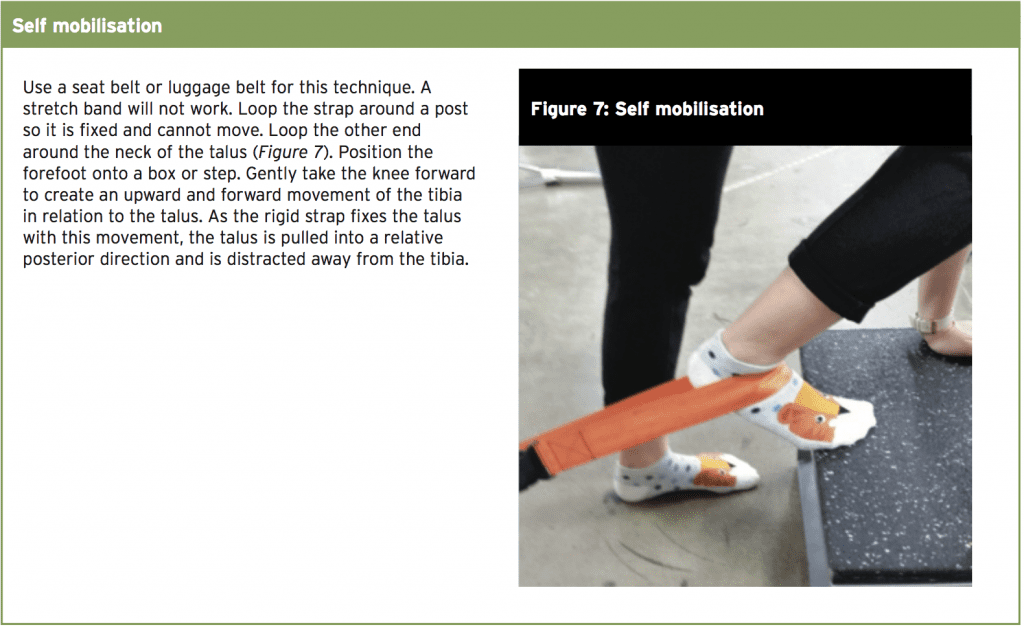
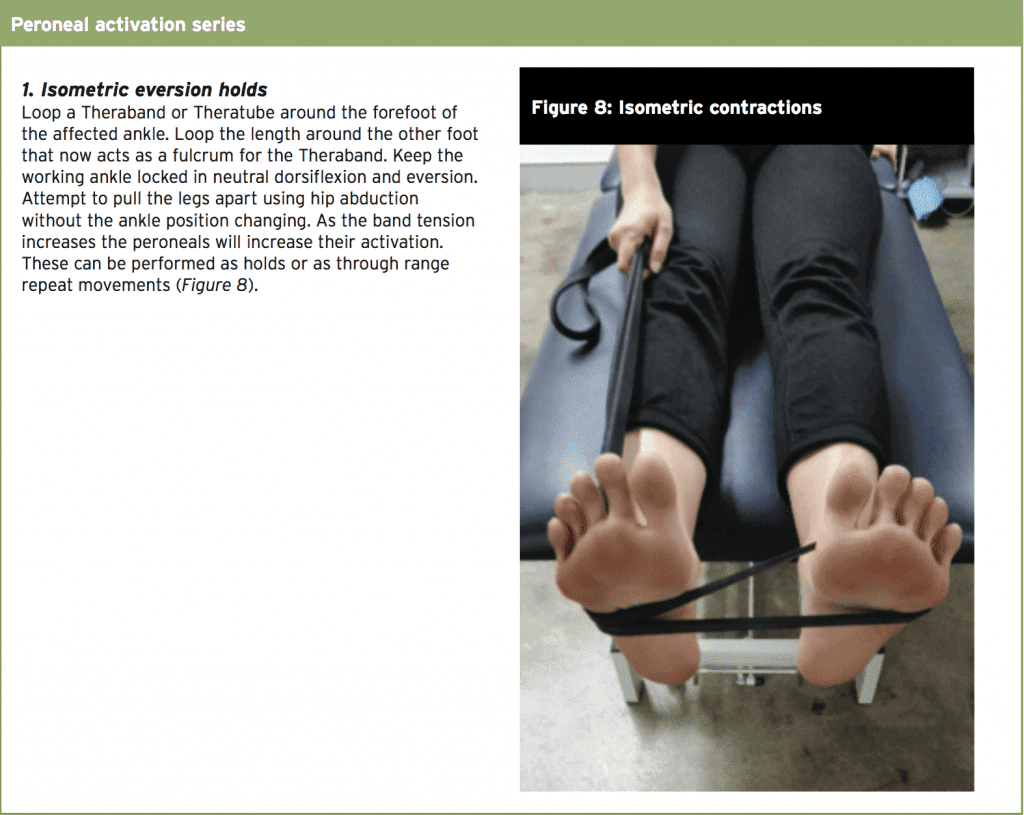
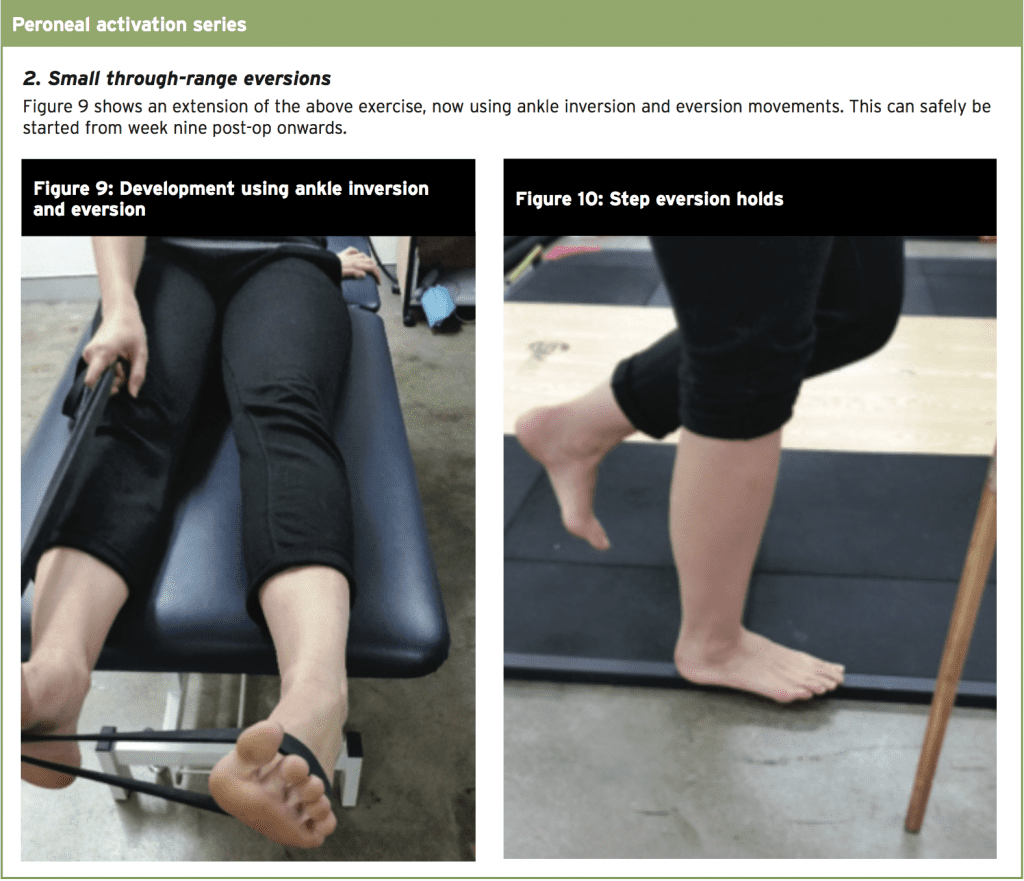
The post-operative rehabilitation following surgical repair of the ankle with CAI is quite extensive for the athlete and this incorporates direct interventions such as talocrural dorsiflexion techniques to improve range of motion, peroneal muscle activation to improve the function of these protective muscle units, as well as frequent functional testing such as the SEBT and hop tests, which will provide the athlete with the confidence and resilience to return to high level sport.
References
1. Sports Med. 2007;37(1):73–94
2. Am J Sports Med. 1977;5:241–242
3. United States Bone and Joint Initiative. The Bone and Joint Decade: The Burden of Musculoskeletal Diseases in the United States. http:// www.boneandjointburden.org/. Accessed November 1, 2013
4. Am J Med. 2008;121(4): 324–331, e6
5. Br J Sports Med. 2001;35:103–108
6. J Athl Train. 2002;37(4):376–380
7. J Athl Train. 2002;37:501-506
8. J Orthop Sports Phys Ther. 2006;36:131-137
9. Hengeveld E and Banks K (2013) Maitland’s Peripheral Manipulation, 5th Edition ‘Management of Neuromusculoskeletal Disorders’ – Volume 2. Churchill Livingstone
10. Hing et al (2015) The Mulligan Concept of Manual Therapy. Churchill Livingstone
11. Am J of Sports Med. 2009. 37(5); 982-988
12. J Orthop Phys Ther. 2011. 41(6); 377-387
References
1. Sports Med. 2007;37(1):73–94
2. Am J Sports Med. 1977;5:241–242
3. United States Bone and Joint Initiative. The Bone and Joint Decade: The Burden of Musculoskeletal Diseases in the United States. http:// www.boneandjointburden.org/. Accessed November 1, 2013
4. Am J Med. 2008;121(4): 324–331, e6
5. Br J Sports Med. 2001;35:103–108
6. J Athl Train. 2002;37(4):376–380
7. J Athl Train. 2002;37:501-506
8. J Orthop Sports Phys Ther. 2006;36:131-137
9. Hengeveld E and Banks K (2013) Maitland’s Peripheral Manipulation, 5th Edition ‘Management of Neuromusculoskeletal Disorders’ – Volume 2. Churchill Livingstone
10. Hing et al (2015) The Mulligan Concept of Manual Therapy. Churchill Livingstone
11. Am J of Sports Med. 2009. 37(5); 982-988
12. J Orthop Phys Ther. 2011. 41(6); 377-387




