The lower trapezius is an important periscapula muscle that plays a vital role in dynamic scapula movement. Chiropractor, Dr. Alexander Jimenez takes a look at the anatomy and biomechanics, and explains the implications for rehab when trying to activate the lower trapezius from early stage painful shoulder stages to end stage high performance.
The lower trapezius is a muscle that is proposed to play an important role in ‘ideal’ scapula mechanics. It is agreed that poor scapula movement (scapula dyskinesis) during overhead activities may predispose the athletic shoulder to injury in the form of impingement, subacromial bursitis and instability(1-3). Due to the role it plays in scapula function and subsequent athletic shoulder pain, the lower trapezius has received a lot of interest, regarding both its activation ratios against the other trapezius as well as its timing during movement(4-7).
Anatomy
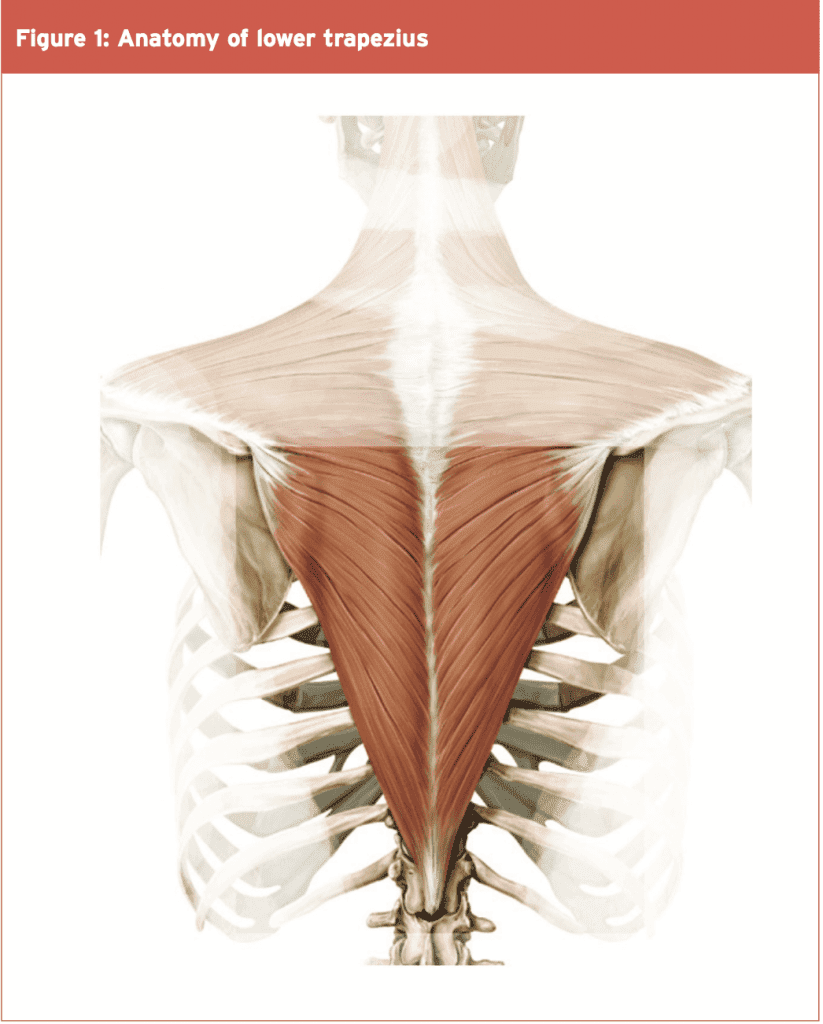
Surprisingly, very little academic research has been conducted on the exact anatomy of the lower trapezius. There is however a plethora of research regarding the role of the lower trapezius in scapula function and the association between lower trapezius dysfunction and shoulder pain. The most notable research piece on the anatomy of the lower trapezius was only conducted relatively recently in 1994 by Johnson et al(8). They found that the lower trapezius originates on the spine and extends from T2 to T12 and inserts onto the spine of the scapula from the acromian process to its root. It is closely aligned to the middle trapezius which attaches to the C7 and T1 vertebrae, and this also attaches to the spine of the scapula. It is a multi- pennate muscle that is innervated by the accessory nerve and the ventral rami of the third and fourth cervical nerves via the cervical plexus (see Figure 1).Function of the lower trapezius
The scapula forms the basis of all upper limb kinetic chain movements. It must be mobile enough to achieve the optimal positions needed to allow the humerus to move unimpeded and without impingement. It also needs to remain solid and stable during upper limb movements, particularly overhead activities in sport to allow the proper transmission of force from the body to the hand – thus highlighting its importance in sports such as swimming, tennis and throwing sports.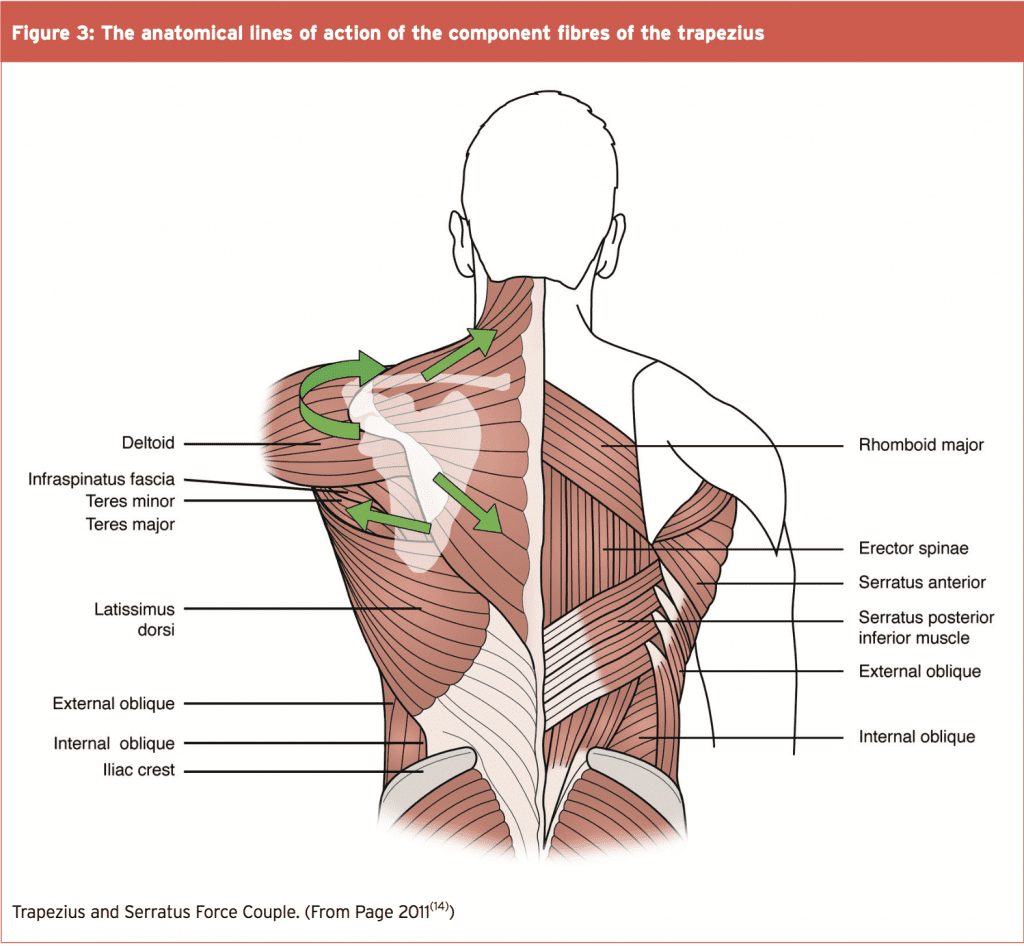
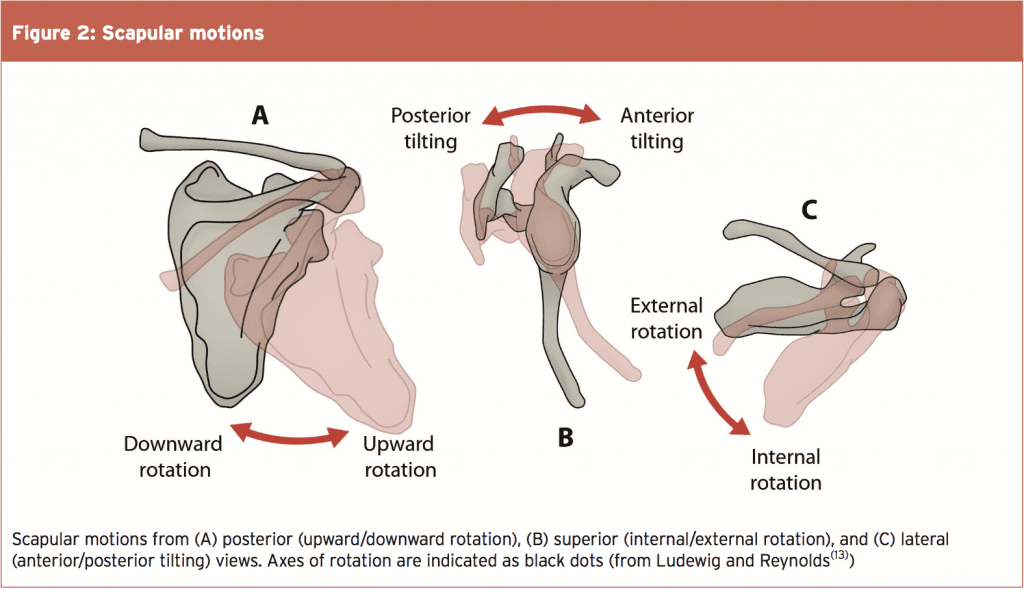
The lower trapezius is one of the many muscles that plays a role in the desired upward rotation, posterior tilt and external rotation of the scapula along with the middle trapezius and serratus anterior. It must be noted that the role the lower trapezius plays in scapula function cannot be discussed in isolation as it works with the other muscles to create a ‘force couple’ at the scapula. Furthermore, the contribution of ‘other’ competing factors in scapula dysfunction such as pectoralis minor tightness, posterior shoulder capsule tightness and thoracic spine stiffness need to also be considered(13).
The exact role of the trapezius during shoulder motion has been thoroughly researched by Johnson et al (1994)(8). Calculating the anatomical lines of action of the component fibres of the trapezius, and considering these lines of action in combination with the changing scapulothoracic axis of rotation, they found that the middle and lower trapezius are ideally suited for scapular stabilization and external rotation of the scapula. This is because the instantaneous centre of rotation of the scapula on the thorax has been found to move from the root of the spine towards the AC joint, nearly along the line of trapezius insertion.
The middle trapezius directed medially has only a small moment arm for upward rotation and is subsequently likely most active to offset protraction from the serratus anterior. The lower trapezius is the only component of the trapezius that can significantly upwardly rotate the scapula. However its relative moment arm will change across the range of motion for arm elevation. As the scapula moves through upward rotation (a movement that shortens the lower trapezius), it also protracts and elevates somewhat (movements that elongate the lower trapezius). So in fact, the actual change in muscle fibre length can remain somewhat unchanged, making the lower trapezius contraction almost exclusively isometric.
The multiple roles of the lower trapezius can therefore be summarised as follows:
- Stabilises the scapula as the shoulder moves into abduction. The initial movement and inertia of the humerus in abduction causes a ‘drag’ effect on the scapula and pulls it into a downward rotation position. The lower trapezius works as a feedforward muscle prior to abduction to contract, and ‘hold’ the scapula steady to counteract the downward rotation ‘drag’ effect. It therefore neutralizes the scapula at the start of abduction. During the primary 30 degrees of abduction, the scapula does not move but is held stable by the lower trapezius.
- During progressive shoulder abduction (from 30 degrees to 120 degrees), the lower trapezius works to create upward rotation of the scapula (along with the serratus anterior). The lower trapezius muscle stabilises the scapula against the protraction effect produced by the serratus anterior.
- At the uppermost levels of abduction (120+ degrees) it works to also create posterior tilt of the scapula. It counteracts the elevation effect of the upper trapezius and levator scapulae during end of range abduction.
- Whereas the upper trapezius does not appear to have a line of action for being a substantive upward rotator in healthy persons, the lower trapezius assists in producing scapulothoracic upward rotation. Furthermore, evidence indicates that the lower trapezius is the primary upward rotator of the scapula (along with serratus anterior).
- Lower trapezius also retracts and depresses the scapula during horizontal pulling movements such as rowing and works with other scapular retractors in postural positions to counteract the effect of scapular protraction whilst sitting.
- Lower trapezius activity has been found to be relatively low at angles less than 90 degrees of scapular abduction and flexion, with exponential increases from 90 to 180 degrees(15). This would highlight the increasing role it plays in upward rotation and posterior tilt as the shoulder abducts above 90 degrees.
Dysfunction & Shoulder Pain Syndromes
As with any research study that demonstrates a relationship between a muscle dysfunction and associated joint pain, care must be taken to assume a cause and effect relationship between lower trapezius dysfunction and subsequent shoulder pain. Is it that the muscle is dysfunctional and this leads to poor scapula movement and hence pain syndromes? Or is it that pathology in the joint develops first and this then inhibits the lower trapezius? Whether it is cause or effect, the presence of a dysfunctional lower trapezius leads the clinician to rationalize that the muscle needs some direct intervention to improve its function.Numerous studies have been conducted on the role that the periscapular muscles play in scapula function/dysfunction and associated pain syndromes. It has been recognised that the scapula muscles (lower trapezius included) play a vital role in the ability of the rotator cuff to function properly. They create a stable scapula that allows the rotator cuff to function more efficiently by allowing the maintenance of the optimal length to tension ratios in the rotator cuff(16-19). Below is a summary of the findings of a select few (of the many) studies relating to lower trapezius dysfunction and pain syndromes:
1. A lack of activity in the lower trapezius has been observed with overhead movements that cause impingement, often in combination with an excessive upper trapezius activation(20).
2. Mechanisms often associated with secondary subacromial impingement are low levels of serratus anterior and lower trapezius muscle activation, which cause prominence of the medial border and inferior angle of the scapula, combined with its excessive internal rotation(21-23).
3. Lower trapezius strength is decreased in individuals with unilateral neck pain(24,25).
4. Significantly delayed middle and lower trapezius activation has been demonstrated in overhead athletes with shoulder impingement, in response to an unexpected drop of the arm from an abducted position(26). The lower trapezius appears to react too slowly when compared to the upper trapezius, which may become overactive, leading to scapular elevation rather than upward rotation.
5. Cools et al (2004) found a decrease in lower trapezius activity during isokinetic scapula protraction in 19 overhead athletes with subacromial impingement(27).
6. Cools et al (2007) reported that athletes with impingement have a significantly higher upper trapezius activation compared to normal subjects, a significant decrease in lower and middle trapezius activation, and altered trapezius muscle balance(28).
Lower Trapezius Activity In Selected Exercises
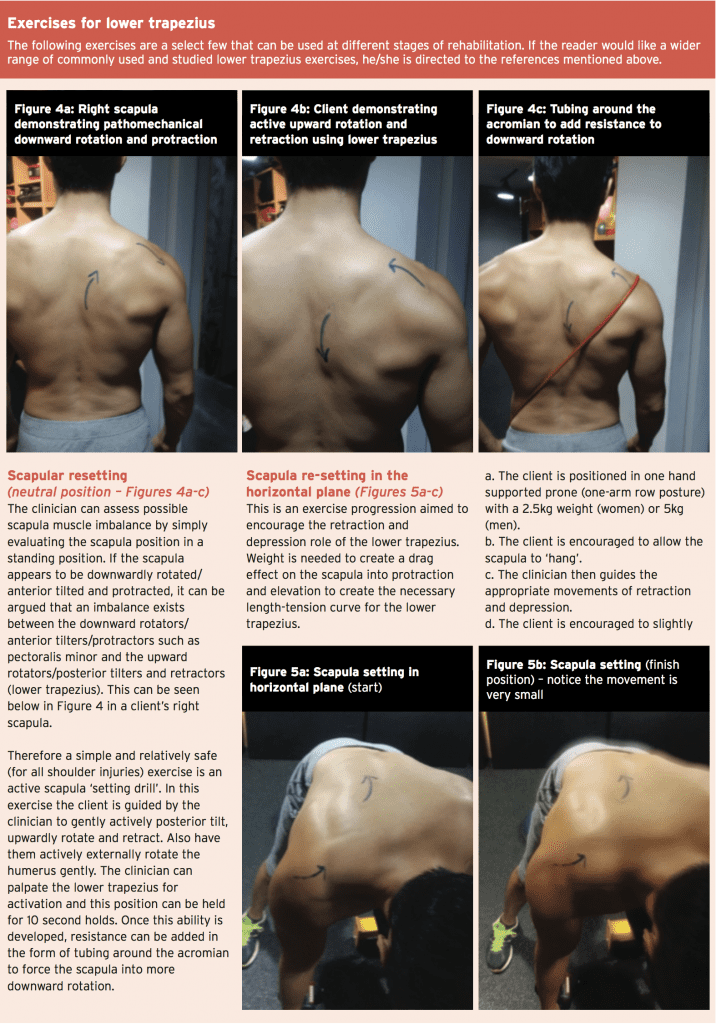
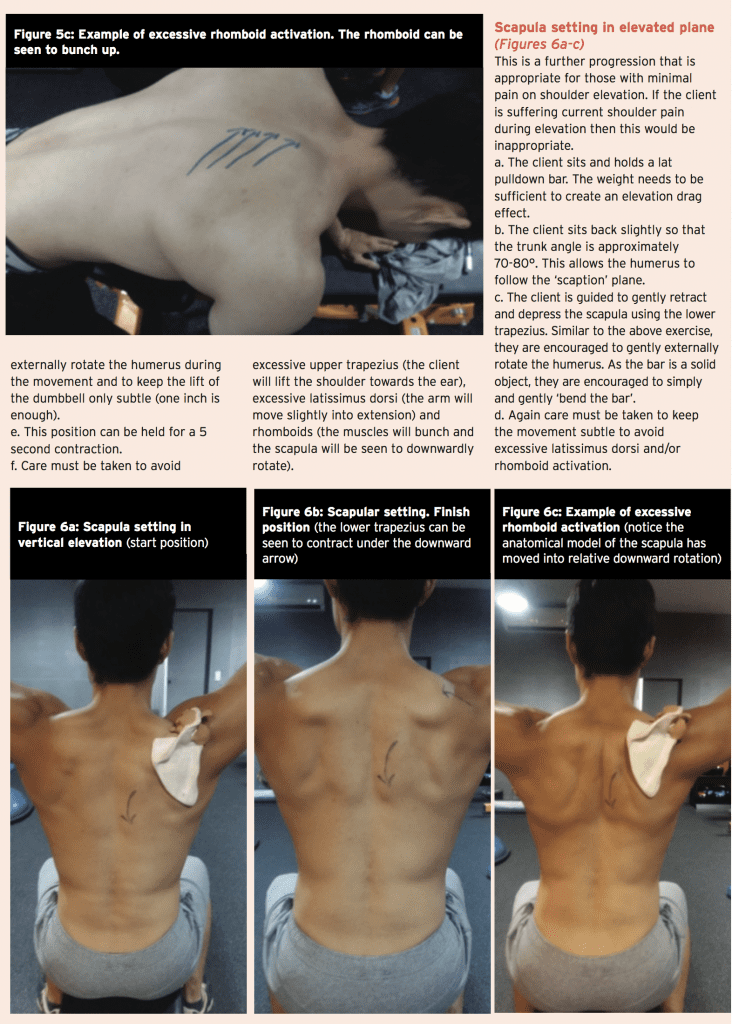
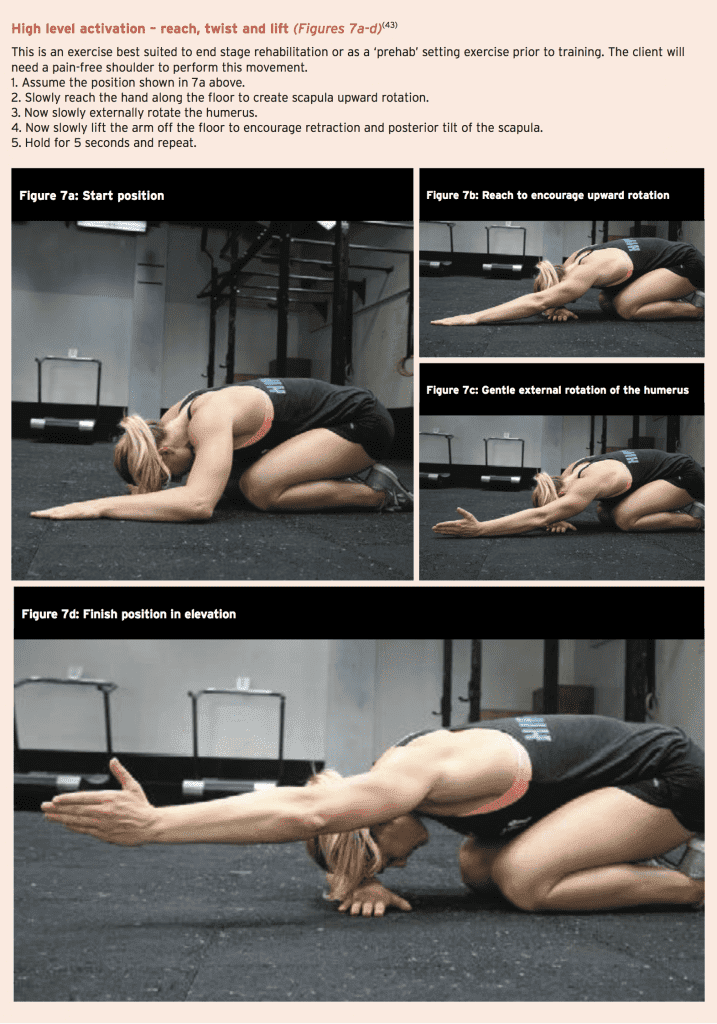
A significant amount of conflict exists in the literature regarding the choice of exercises that should be used to rehabilitate the lower trapezius. Some authors argue that the threshold for recruitment should be kept low, because high levels of muscle activity is not reflective of the role the lower trapezius plays in function(29,30), and that the exercises for functional recovery of patients with this imbalance must be performed with reduced activation to avoid fatigue (around 20% to 40% of maximum voluntary contraction)(31). Furthermore, high levels of activity may be associated with ‘overflow’ to other scapular muscles such as upper trapezius and even the latissimus dorsi.
Others argue that the exercises need to be performed in weight bearing and in kinetic chain patterns to truly imitate what the muscle does in gross kinetic chain function(32-34). They have made the point that in normal sports specific movements, early upper trapezius activity is normal, and thus rehabilitation for athletes should encourage early upper trapezius activation(35). Some of the more significant findings worth mentioning in relation to lower trapezius activation with rehabilitation exercises are as follows:
- Many studies recognise the importance of glenohumeral external rotation in activating greater lower trapezius activation(30,35-38). Exercises such as the ‘scaption’(30), ‘robbery exercise’(32,39), the lawn mower’ and the ‘shoulder horizontal with external rotation’, all elicit greater levels of lower trapezius activation. The reason for this is supported by the work of Kibler et al (2006), which states that the rotator cuff and scapular stabilisers work together to maintain optimal length- tension relationships in the rotator cuff(16). They postulated that with shoulder external rotation, as the humeral attachment of the infraspinatus and posterior deltoid approximates the scapula, the muscle would lose optimal length-tension. Therefore if the scapula was to retract as the same time as humeral external rotation, the medial scapula would move away from the humeral attachment, thus maintaining the length-tension relationship.
- Arm elevation position also seems to be important. Abduction angles around 130 degrees seem to elicit the greatest lower trapezius activation whilst still minimising upper trapezius(39-42). For example, Ekstrom et al (2003) used surface EMG during 10 different exercises. They demonstrated that the position in which the participants elevated the humerus above the head in line with the lower trapezius muscle fibres activated the lower trapezius up to 97% MVIC(40).
Summary
The lower trapezius is an important periscapula muscle that plays a vital role in both dynamic scapula movement as well as holding the scapula stable when required in overhead functional movements. It has been shown that a dysfunction between the lower trapezius in terms of activation exists in the presence of shoulder pain. Therefore it is a muscle that requires direct activation work for it to regain its functional role in scapula control. This article presents a number of exercises that can be utilised to activate the lower trapezius from early stage painful shoulder stages to end stage high performance.References
1. Scand J Rehabil Med (1995) 27: 243-252
2. Shoulder. J Sport Rehabil (1995) 4: 122-154
3. Orthop Clin North Am (2000) 31: 247-261
4. Scand J Med Sci Sports. 2007;17:25-33
5. Br J Sports Med. 2004;38:64-68
6. Phys Ther. 2000;80:276-291
7. Int J Sports Med. 1997;18:618-624
8. Clin Biomech 1994;9:44–50
9. Sports Med. 2008;38(1):17–36
10. Br J Sports Med. 2010;44(5):319–327
11. Clin Biomech (Bristol, Avon). 2003;18(5):369–379
12. Br J Sports Med. 2010;44(5):300–305
13. J Orthop Sports Phys Ther. 2009 February; 39(2): 90–104
14. The International Journal of Sports Physical Therapy. 2011. 6(1). 52-58
15. Journal of Orthopaedic and Sports Physical Therapy 2009;39(2):105–117
16. Am J Sports Med. 2006;34(10):1643–1647
17. Arch Phys Med Rehabil. 2002;83(1):60-9
18. Physiotherapy. 2005;91(3):159-64
19. Clin Biomech (Bristol, Avon). 2000;15:95-102
20. BMC Musculoskeletal Disorders 2010;11:45
21. J Manipulative Physiol Ther. 2007;30(1):69-75
22. Physiotherapy. 2001;87(9):458-69
23. J Bone Joint Surg AM. 1998;80(5):733-738
24. J Orthop Sports Phys Ther 2011 41: 260-265
25. J Spine 2012, 1:3
26. Am J Sports Med. 2003;31(4):542–549
27. Br J Sports Med. 2004;38:64-68
28. Am J Sports Med. 2007;35: 1744-1751
29. J Orthop Sports Phys Ther. 2011;41(7):520-5
30. ConScientiae Saúde, vol. 11, núm. 4, 2012, pp. 660-667
31. BMC Musculoskelet Disord. 2010;11(45):1-12
32. Journal of Athletic Training 2015;50(2):199–210
33. Clin Sports Med. 2008;27:821 – 831
34. J Athl Train. 2000;35:329-337
35. International Journal of Sports Medicine, 18, 618–624
36. Phys Ther. 1993;73:668-677
37. Journal of orthopaedic & sports physical therapy 2009 39(10); 743-752
38. J. Phys. Ther. Sci. 2015 27: 97–100
39. Am J Sports Med. 2008; 36(9):1789–1798
40. J Orthop Sports Phys Ther. 2003;33(5):247– 258
41. Physical Therapy in Sport 2001;2:178–185
42. Sports Med. 2009;39(8):663–685
43. Long Z and Casto B (2014) The Cross Fit Journal. The Optimal Shoulder. http://journal.crossfit.com