Science has been described as the ‘systematic classification of experience’. With that in mind, chiropractor Dr. Alexander Jimenez looks at the up-to-date knowledge surrounding muscle injuries and their classification. As he explains, by being armed with this information, clinicians can be better equipped to move more rapidly along the road of evidence-based prevention and rehabilitation programming.
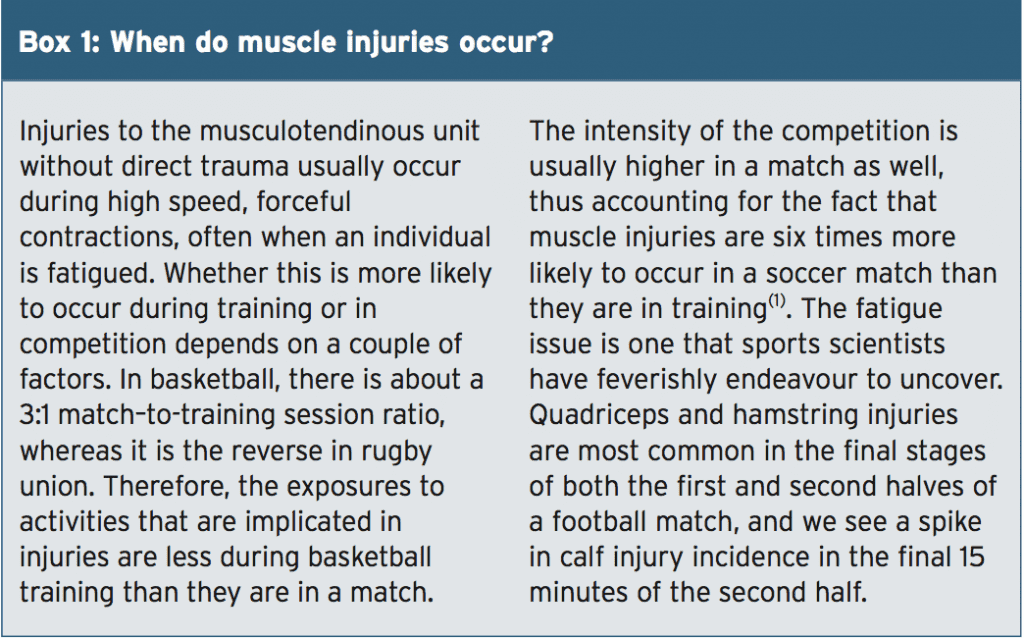
Performance support teams working with athletes the world over often agonize over injury lists. Of course, people go into sport knowing that the risk of injury is an ever- present, but particularly galling are the so-called ‘preventable’ injuries. In most cases, the injury that springs most readily to mind as ‘preventable’ is that of the soft tissue (musculotendinous unit) variety. Whether fair or not, it’s a fact that the efficacy of many sports medicine departments around the world is measured by the incidence of muscle strains in their athletes. What is undeniable however is the fact that we need to understand our ‘foe’, if we are to reduce the risks of it defeating us.
The Extent Of The Problem
In most team-based running sports, muscle injuries consistently rank among the chief causes for playing and training time missed, accounting for anywhere between a fifth and a half of all time loss injuries in the various football sports around the world. Broadly speaking, a football manager can expect a player to sustain a muscle injury every two years, with around a fortnight missed for every injury(1).Of course, not every player on the squad will sustain a muscle injury, so, let’s just ask for a license to extrapolate here. What we can say is that approximately half a squad will sustain a muscle injury in a season. A football squad usually comprises somewhere between 24-30 players, meaning that 12-15 players will sustain a muscle injury, with an average time out of two weeks. A simple calculation shows that this totals 24-30 weeks out which, given the tight fixture scheduling, may mean 30-45 games missed, And when you consider that most successful teams in world sport need to have consistent team selections that are not hampered by injury, muscle injuries are clearly a problem worth understanding!
 |
| Guidelines for chiropractic care low back pain treatment |
In sports such as Australian Rules football, the formalized central epidemiology reporting system does not reflect pre-season injuries (an injury is only counted if it results in a missed match). This means muscle injuries are going to be underreported. Any reporting study, therefore needs to clearly define what constitutes an injury.
According to the UEFA Champions League study by Hagglund and his co-workers, an injury is said to have occurred when an incident takes place during a scheduled training session or a match that results in an absence from the next scheduled training session or match(2). Whilst this may give us an indication of injury prevalence (how often something happens), we are really interested in injury severity (how long someone is out for). This is easily calculable by determining the number of days missed. The same UEFA study defined the following:
- Minimal injury (1-3 days missed)
- Mild injury (4-7 days missed)
- Moderate injury (8-28 days missed)
- Severe injury (>28 days missed).
The MLG-R Classification System
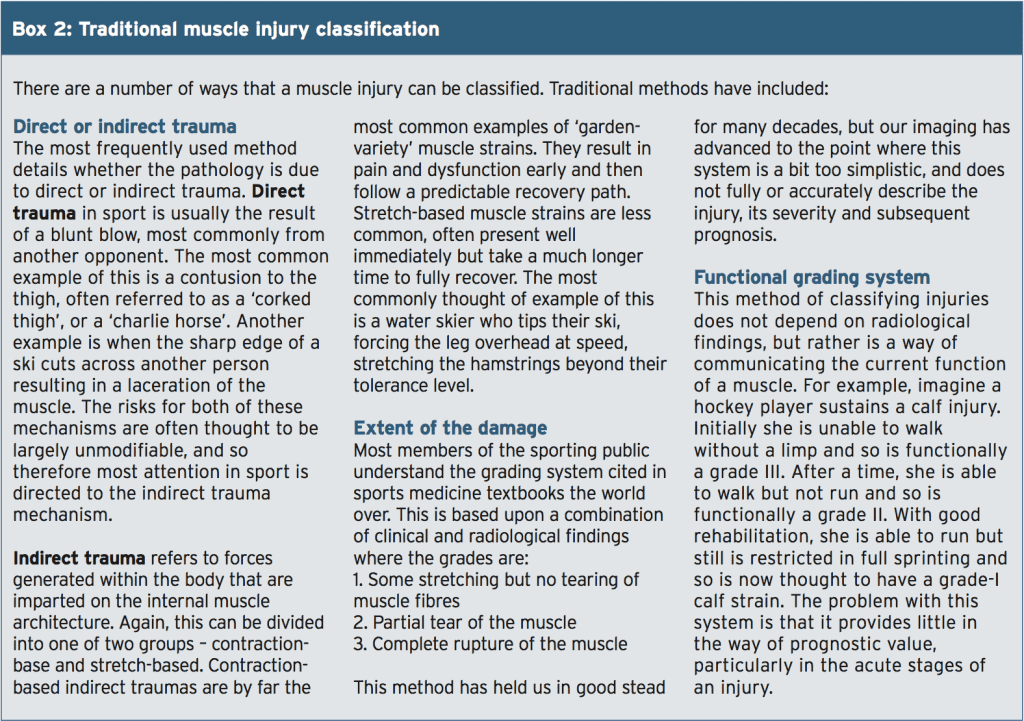
Last year, a group of researchers and practitioners from FC Barcelona and Aspetar published the third iteration of their Muscle Injuries Clinical Guide(3). This classification system seeks to provide a lot more information regarding the injury severity, and therefore help guide the appropriate management. Let me take you through this clumsy sounding acronym:
M = Mechanism. This refers to whether it is a direct (D) or indirect (I) mechanism, as we have discussed previously.
L = Location. This refers to where the injury is localised. For direct injuries (D), it could be located in the proximal third (Dp), middle third (Dm), or distal third (Dd). Indirect injuries (I) are categorized according to the type of connective tissue that is implicated, whether that is tendon (IT) (more severe) or the more common musculotendinous junction (IJ). These are then subdivided according to whether they are proximal (ITp/IJp) or distal (ITd/ IJd). The final indirect location (IF) refers to those indirect mechanisms that are thought to have injured the myofascia. In my experience, these recover at up to twice the rate of injuries involving the contractile mechanisms.
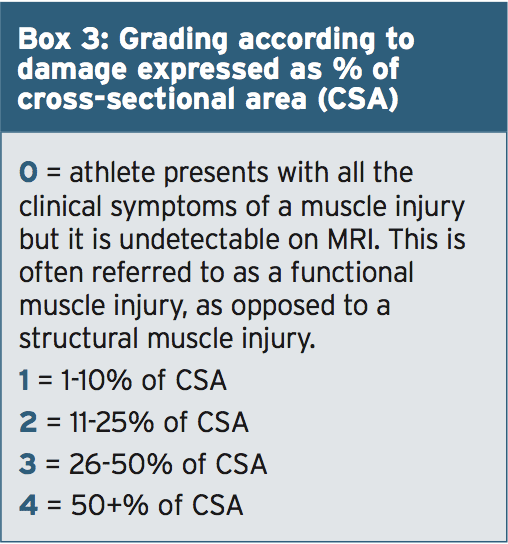
G = Grade. This requires MRI verification and refers to the extent of the damage expressed as a percentage of the cross sectional area (CSA) of the affected muscle (see Box 3).
R = Re-injury. This is the final brick in the nomenclature wall that denotes how often this injury has occurred. So, if this was the first time occurrence, it would be classified as a R0, whereas if it was the 4th time the same injury had occurred to the same muscle, it would be written as R4.
MLG-R Examples
Let’s look at some real examples to bring this seemingly complicated system to life:Example 1
Last weekend, the captain of our football club was running for the ball and felt a sudden grab in the back of his thigh. Despite having endured many injuries over the years, he’d never experienced anything like this before. He had to come off to be assessed and it was determined that he could not come back on to play any further part of the match. The following day, we sent him for an MRI and it revealed a tear of his biceps femoris tendon, 13 cm below the ischial tuberosity with almost a third of the CSA of the muscle torn as well. Accordingly, his injury would be classified as: Left Biceps Femoris ITp3R0.Example 2
Three weeks ago, one of our forwards was waiting to receive the ball from a teammate. The kick was a bit too high and allowed an opponent to smash into the back of him to spoil his attempt. Despite our best efforts, he was unable to continue playing due to the extreme pain coming from his hamstrings whenever he tried to run. Whilst we do not scan every single injury at our organisation, we decided to in this case because he began to complain of some tingling down in his calf and we were concerned about bleeding and swelling compressing his sciatic nerve. The results of the scan showed that he had extensive bleeding coming from his left biceps femoris and the affected tissue accounted for about 20% of the muscle’s CSA. He felt particularly aggrieved because he had just returned from a similar injury two weeks before. Accordingly, we notated this injury as a Left Biceps Femoris Dm2R1.Example 3
Last year, when I was working in rugby union, one of our second row players complained of an odd chest pain. He thought it may have occurred following a collapse of a scrum. He was point tender near his sternum, had difficulty with horizontal arm flexion. I suspected that he had sustained a pectoralis major injury. Subsequent imaging revealed almost a complete separation of the lower half of the sternal head of his pectoralis major, an extremely uncommon injury. Under this classification system, his injury would be written down as a Right Pectoralis Major (sternal head) IJd4R0.Conclusion & Practical Value Of Precise Classification
As more specialists become involved with the care of these athletes, ranging from sports doctors, to radiologists, to physiotherapists, to strength coaches, it is really important to ensure that we are all on the same page when communicating about the mechanism, location and extent of a soft tissue injury.Whilst this classification system proposed by the folk from FC Barcelona and Aspertar may seem convoluted, it is actually a very efficient method of concisely and accurately communicating the injury, ensuring consistency in terminology. Sub-categorising in this manner provides us with the first step in ensuring consistency in data collection/ epidemiology, and in communication. This in turn can help clinicians by more accurately guiding the top-quality class management that all athletes deserve.
References:
1. Ekstrand, J., Hagglund, M., and Walden, M.(2011) Injury incidence and injury patters in professional football: The UEFA injury study. BJSM, 45, 553-558.
2. Hagglund, M et al. (2005). Methods for epidemiological study of injuries to professional football players: developing the UEFA model. BJSM, 39, 340-346.
3. Pruna et al. (2015). Muscle Injuries ClinicalGuide 3.0.




