In the first part of this two-part article, chiropractor, Dr. Alexander Jimenez reviewed the recent research on the underlying biomechanics of iliotibial band syndrome. In part 2, he looks at diagnosis and treatment options.
In some athletes, repeated knee flexion causes the iliotibial band (ITB) to produce friction over the lateral femoral condyle (LFE), or compression of the tissue underneath it. That tissue could be a fat pad or an outcropping of the synovial lining. Whether the cause is friction or compression, or the tissue is adipose or synovial, is really academic. The end result is the same: persistent lateral knee pain that can side-line an athlete.
Functional Anatomy
Every gait cycle requires an abduction moment during unilateral stance. As the weight transfers to the single leg, the posterior portion of the gluteus medius and the entire gluteus minimus produce force vectors parallel to the neck of the femur and stabilise the femoral head within the hip socket. The anterior and middle fibres of the gluteus medius, with their vertical force production, initiate the abduction moment at the femur, which is fully realised with the activation of the tensor fascia lata (TFL) (see Figure 1).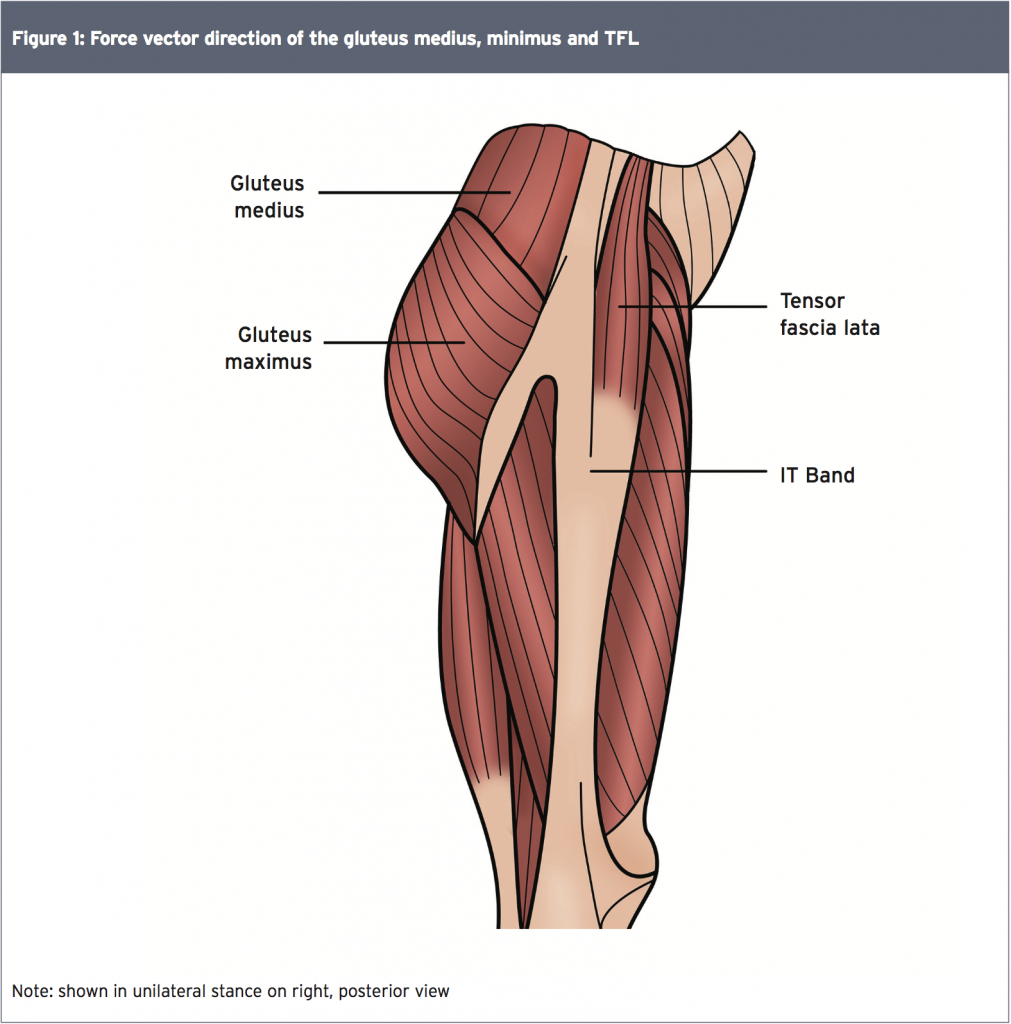
To resist adduction and slow forward progression of the stance leg, these muscles must fire eccentrically and sequentially. When this process is imperfect (for example due to sub-optimum hip biomechanics), ITB is activated in order to assist with abduction. However, while it anchors fibres from the abductor muscles, ITB itself is not a muscle and thus has limited elasticity. The critical point in the gait cycle where the lateral hip muscles are most active coincides with the knee angle that brings the ITB closest to the LFE(1). Therefore, it is easy to see how any dysfunction at the hip strains the ITB and causes pain at the knee.
Diagnosis
Clinicians should suspect ITB syndrome in any athlete who presents with sharp or burning lateral knee pain 2-3cm proximal to the knee joint near the LFE(2). The area may be somewhat swollen or exhibit crepitus or snapping during knee flexion (see Table 1). The clinical exam should include full evaluation of the strength and range of motion of both legs.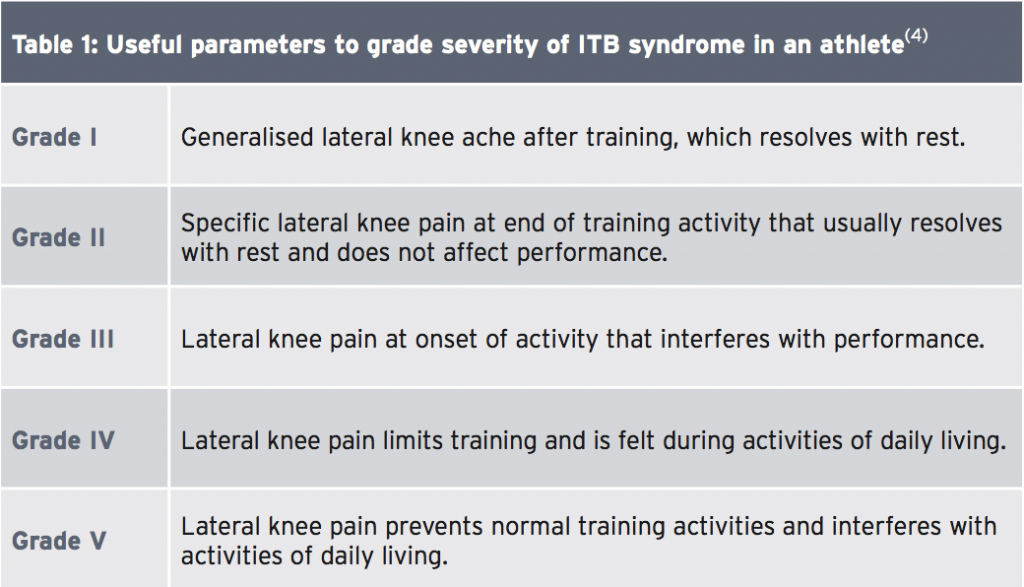
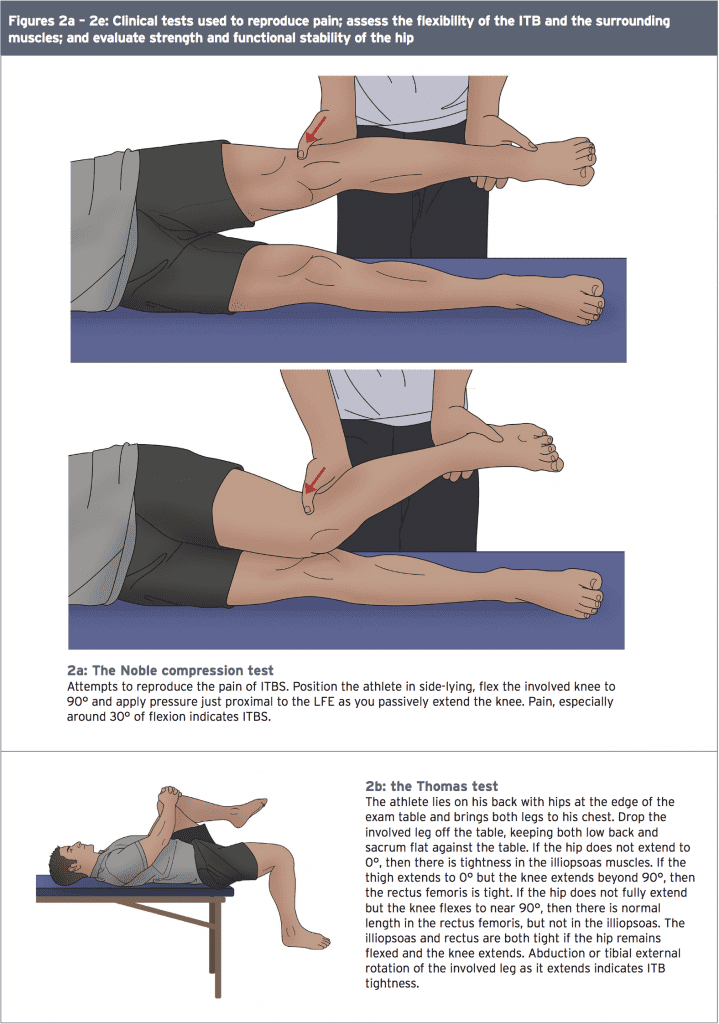
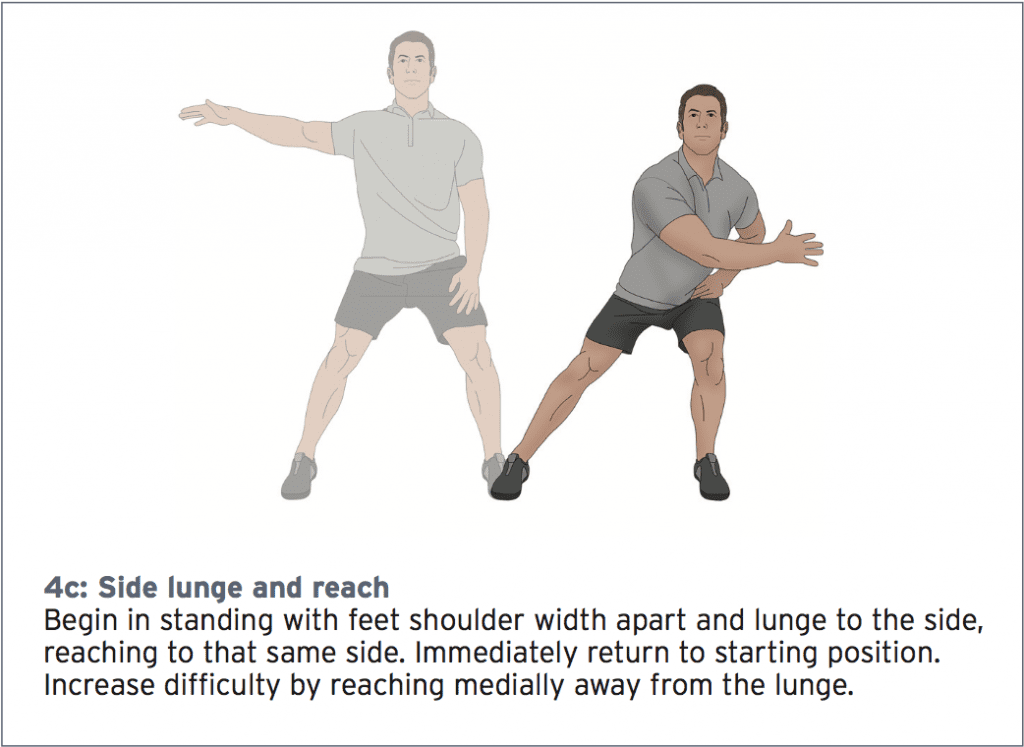
Several clinical diagnostic tests can help determine the presence of ITBS (see Figure 1). The Noble compression test attempts to illicit pain in the ITB at 30 degrees of knee flexion when it is closest to the LFE. The Thomas test assesses flexibility in the ITB and the TFL, along with the quadriceps and hip flexors, while the Ober flexibility test isolates the ITB.
Clinicians should assess the active and passive range of motion of the entire hip joint, observing any tightness in the gluteal muscles. Myofascial constrictions should also be identified and trigger points noted especially ones that refer pain to the lateral thigh or knee.
Tightness in areas besides the hip can also functionally affect the ITB. Examples include tightness in the gastrocnemius and soleus, which decrease closed chain dorsiflexion and therefore increase pronation and knee flexion. Excessive pronation increases internal rotation of the tibia, knee valgus and hip adduction, especially in the presence of weak hip abductors. A leg length discrepancy greater than one centimetre produces a similar effect and therefore should be corrected, along with any foot deformities, with an orthotic insert.
Clinicians should assess the active and passive range of motion of the entire hip joint, observing any tightness in the gluteal muscles. Myofascial constrictions should also be identified and trigger points noted especially ones that refer pain to the lateral thigh or knee.
Tightness in areas besides the hip can also functionally affect the ITB. Examples include tightness in the gastrocnemius and soleus, which decrease closed chain dorsiflexion and therefore increase pronation and knee flexion. Excessive pronation increases internal rotation of the tibia, knee valgus and hip adduction, especially in the presence of weak hip abductors. A leg length discrepancy greater than one centimetre produces a similar effect and therefore should be corrected, along with any foot deformities, with an orthotic insert.
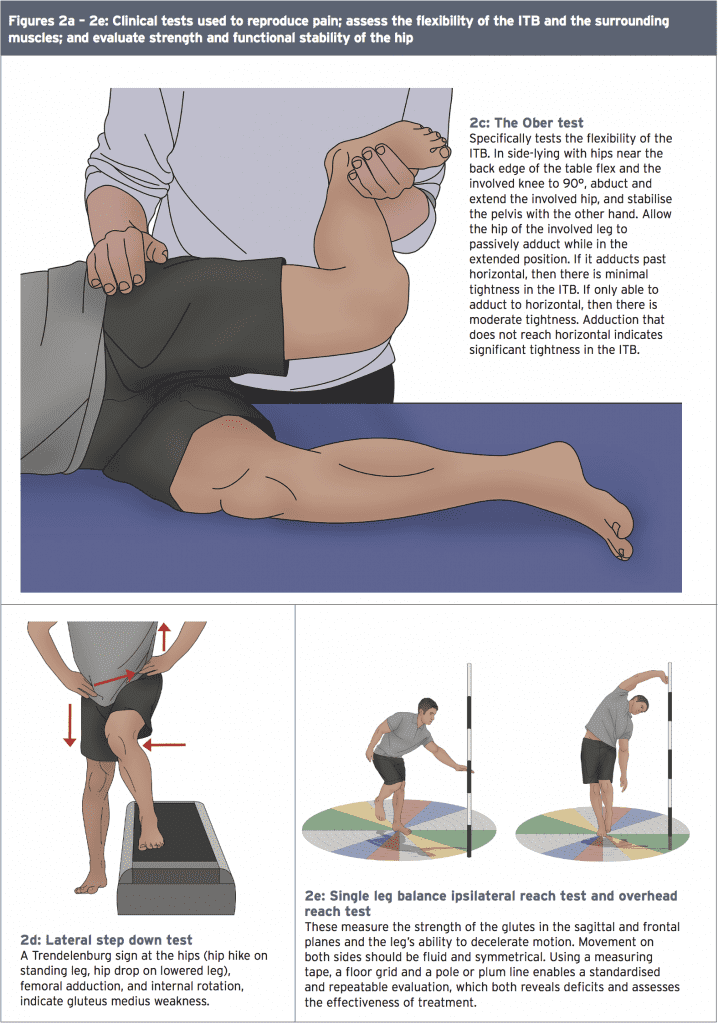
Clinicians should test functional stability and muscle firing patterns at the hip using the step down, unilateral knee flexion, or Trendelenburg test (see Figure 2)
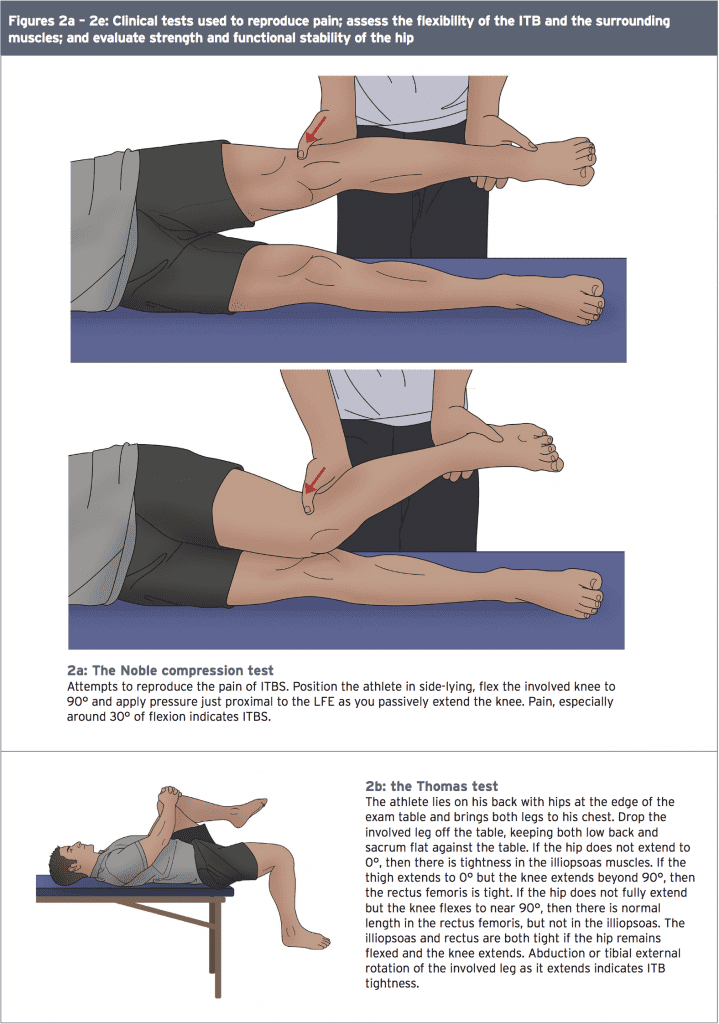
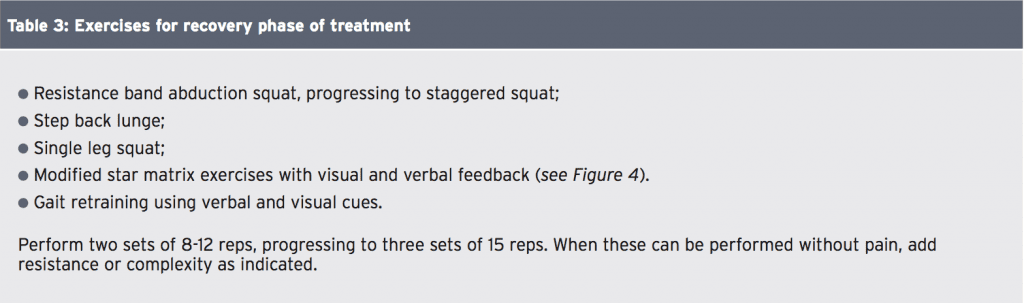
The hallmark of the recovery period is beginning functional closed-chain strength training (see Table 3). These exercises emphasise eccentric muscle contractions and tri-planar movement, because that is how the muscles work in the unilateral stance phase of gait. Provide visual and verbal cues in a mirror while the athlete moves through the exercises.
The next step is to transition biofeedback from these exercises to treadmill running, providing visual and verbal cues for gait retraining. A study at the University of Kentucky found that such cues resulted in decreased hip adduction, internal rotation, and contralateral pelvic drop in ten runners with patellofemoral pain syndrome(5). The cues, provided over eight treatment sessions (15-30 minute treatments, four times each week, for two weeks), gradually faded in the last three sessions. The study required participants to run only during the treatment sessions for those two weeks. The changes in gait patterns also decreased vertical load rates – noteworthy since (as explained in part I of this series) increased strain rate is found in athletes who later develop ITB syndrome. A one-month follow up with the athletes showed they maintained their improved level of pain, function, and gait patterns without further treatment.
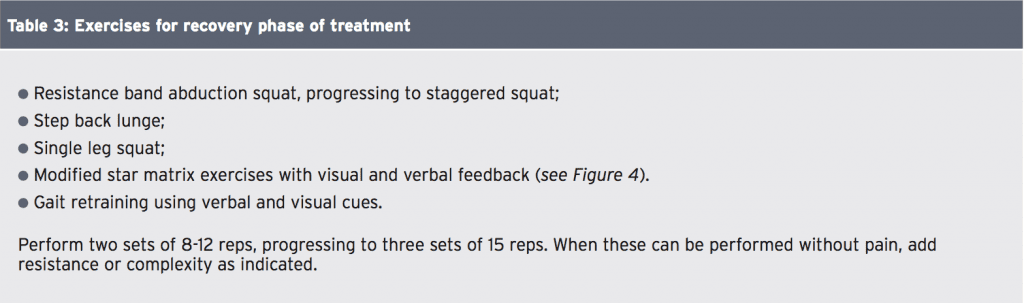
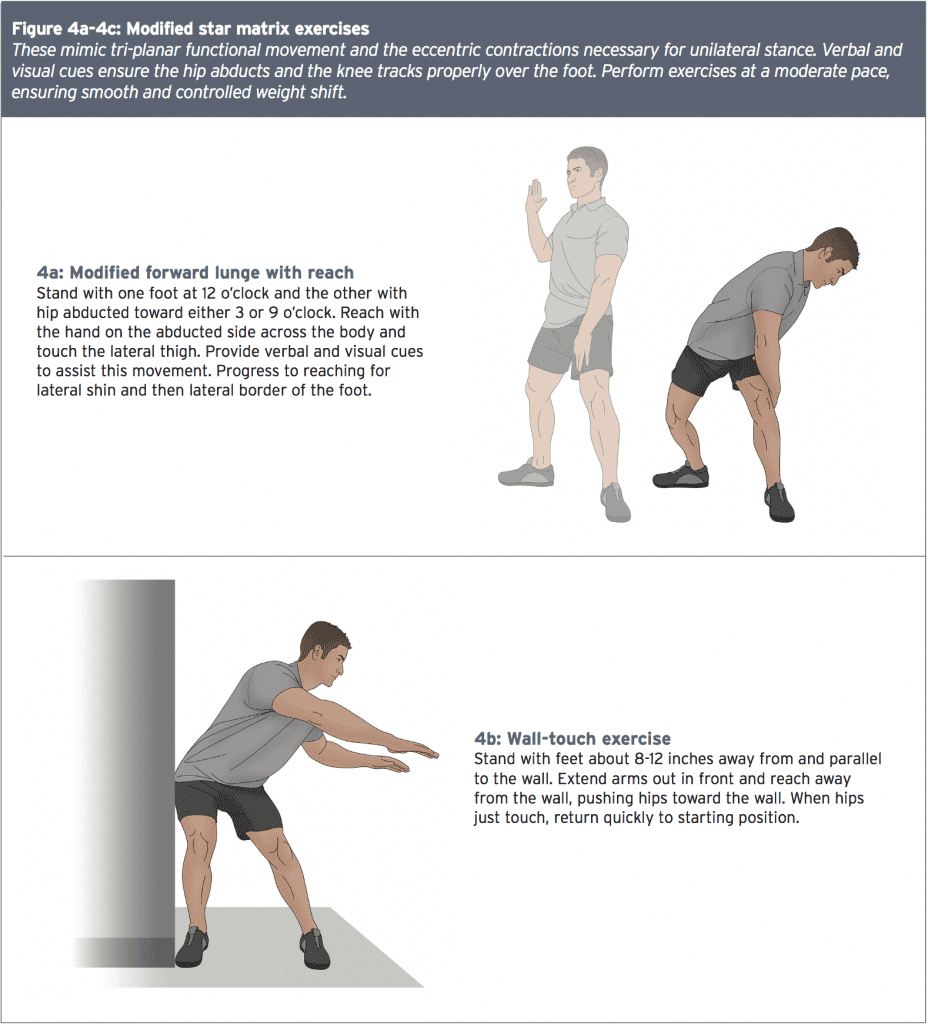
These mimic tri-planar functional movement and the eccentric contractions necessary for unilateral stance. Verbal and visual cues ensure the hip abducts and the knee tracks properly over the foot. Perform exercises at a moderate pace, ensuring smooth and controlled weight shift.
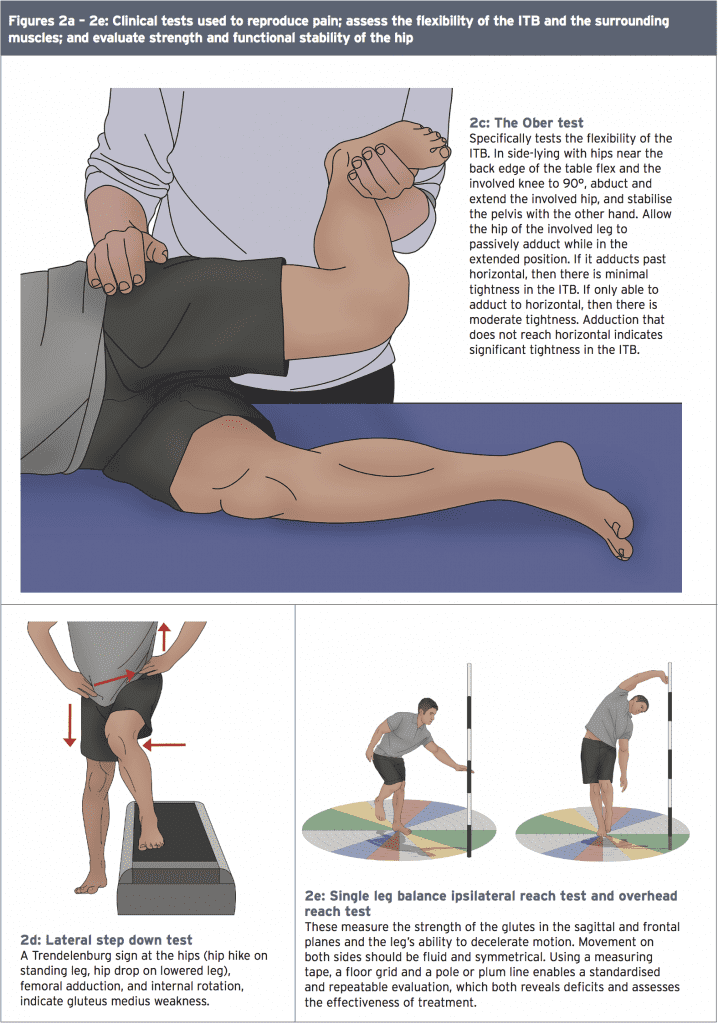
Further functional tests, such as the single-leg balance reach tests assess movement and control in both frontal and sagittal planes of movement. Evaluating running gait to detect imbalances that occur with fatigue is also recommended. Magnetic resonance imaging (MRI) may show thickening of the ITB and fluid accumulation under the ITB near the FLE; however, it is rarely used to diagnose ITB syndrome(3).
With grades IV and V injury, stop all training activity during the acute period other than swimming with a pool buoy. Manage discomfort and swelling with nonsteroidal anti-inflammatory drugs as directed, ice massage, phonophoresis or iontophoresis, kinesio tape, ultrasound, and electrical muscle stimulation. If obvious swelling and pain persist despite conservative management, suggest a localised corticosteroid injection.
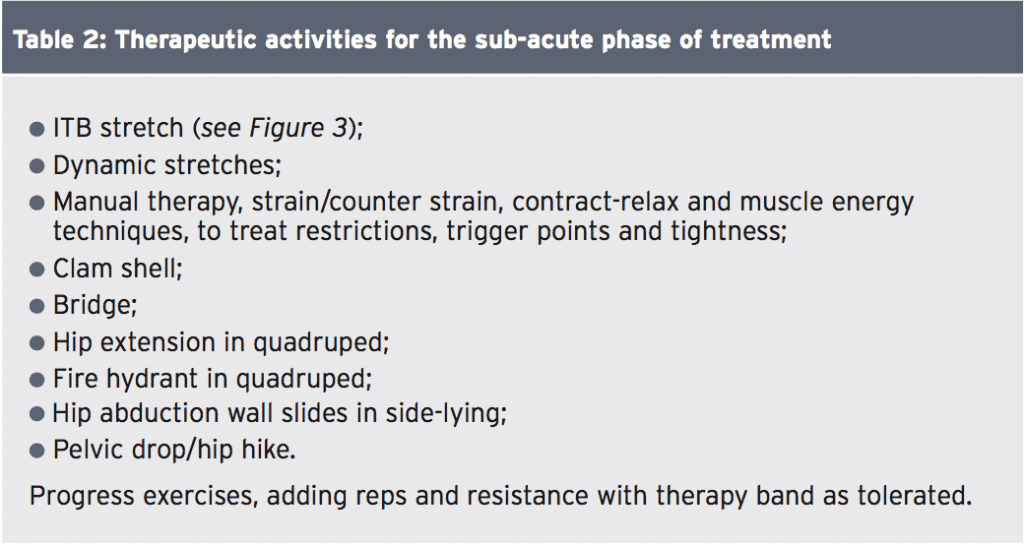
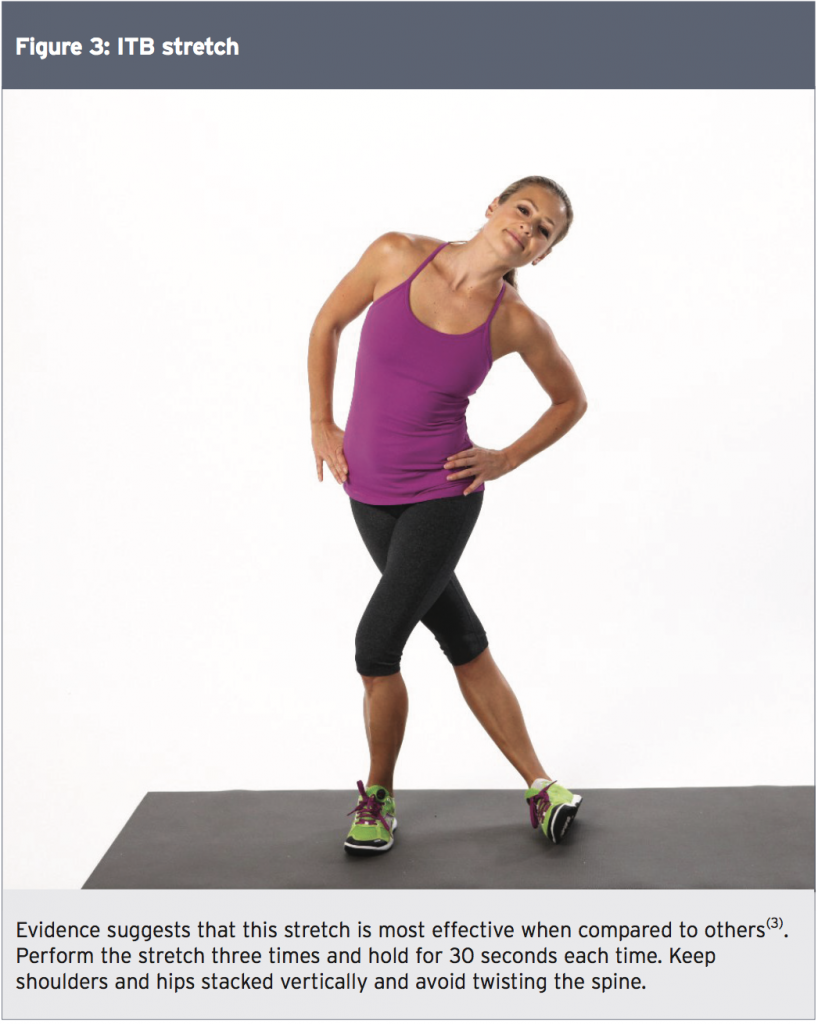
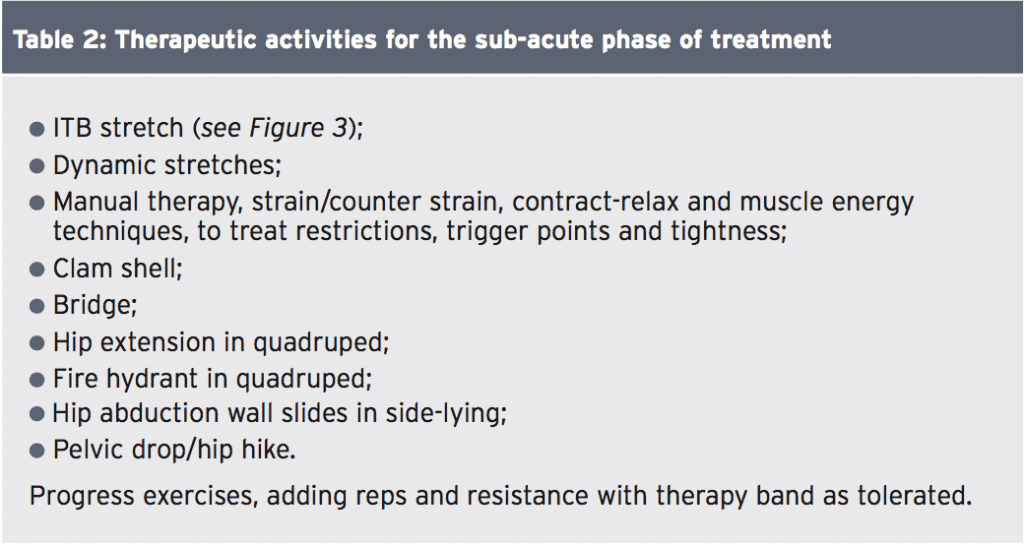
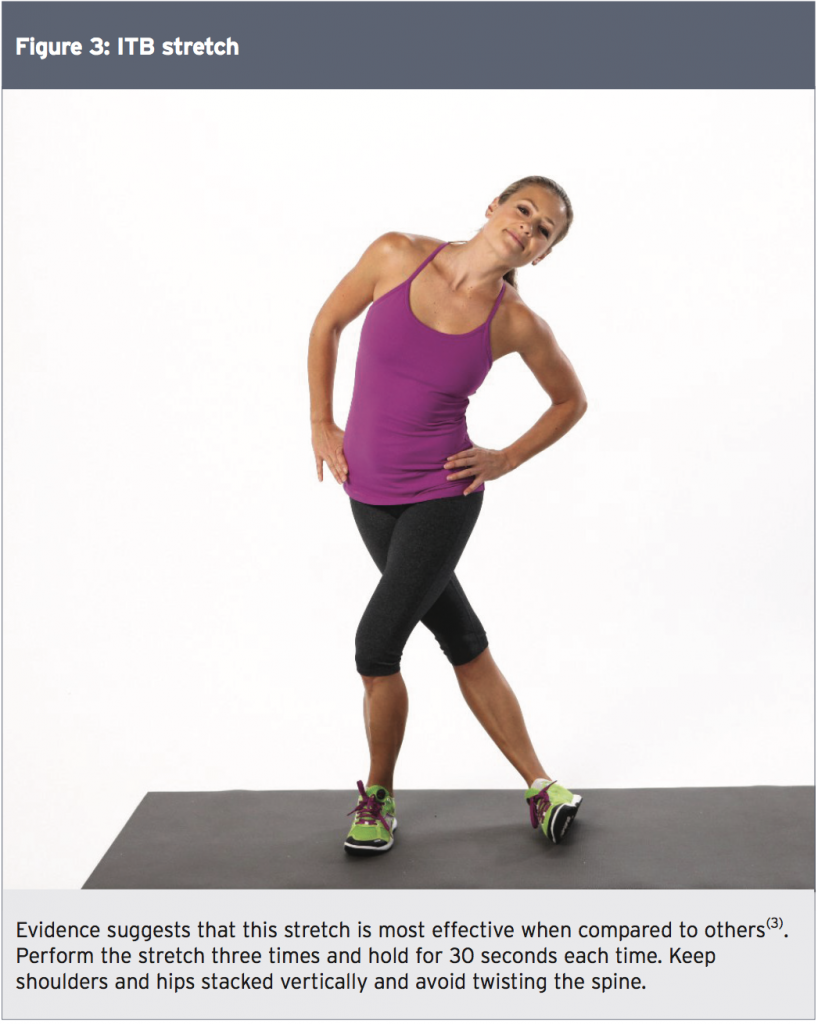
*Sub-acute phase – When the acute pain and inflammation subsides, begin the sub-acute phase of treatment (see Table 2). The goal of this phase is to improve flexibility, joint range of motion, and strength in open-chain positions. Progress the exercise program from two sets of 8-12 reps, to three sets of 15 reps. When these can be performed without pain, add difficulty to exercises with a resistance band. Progress to recovery phase activities when the athlete can execute resisted exercises without pain.
Treatment
*Acute phase – Focus on decreasing pain and inflammation at the lateral knee. Rest is the first line of defense against further damage. For a low-grade injury, this may mean a few days off from training and amending external causes. Buying new shoes, avoiding downhill runs, or running the opposite direction on a track may clear up the condition quickly.With grades IV and V injury, stop all training activity during the acute period other than swimming with a pool buoy. Manage discomfort and swelling with nonsteroidal anti-inflammatory drugs as directed, ice massage, phonophoresis or iontophoresis, kinesio tape, ultrasound, and electrical muscle stimulation. If obvious swelling and pain persist despite conservative management, suggest a localised corticosteroid injection.
*Sub-acute phase – When the acute pain and inflammation subsides, begin the sub-acute phase of treatment (see Table 2). The goal of this phase is to improve flexibility, joint range of motion, and strength in open-chain positions. Progress the exercise program from two sets of 8-12 reps, to three sets of 15 reps. When these can be performed without pain, add difficulty to exercises with a resistance band. Progress to recovery phase activities when the athlete can execute resisted exercises without pain.
The hallmark of the recovery period is beginning functional closed-chain strength training (see Table 3). These exercises emphasise eccentric muscle contractions and tri-planar movement, because that is how the muscles work in the unilateral stance phase of gait. Provide visual and verbal cues in a mirror while the athlete moves through the exercises.
The next step is to transition biofeedback from these exercises to treadmill running, providing visual and verbal cues for gait retraining. A study at the University of Kentucky found that such cues resulted in decreased hip adduction, internal rotation, and contralateral pelvic drop in ten runners with patellofemoral pain syndrome(5). The cues, provided over eight treatment sessions (15-30 minute treatments, four times each week, for two weeks), gradually faded in the last three sessions. The study required participants to run only during the treatment sessions for those two weeks. The changes in gait patterns also decreased vertical load rates – noteworthy since (as explained in part I of this series) increased strain rate is found in athletes who later develop ITB syndrome. A one-month follow up with the athletes showed they maintained their improved level of pain, function, and gait patterns without further treatment.
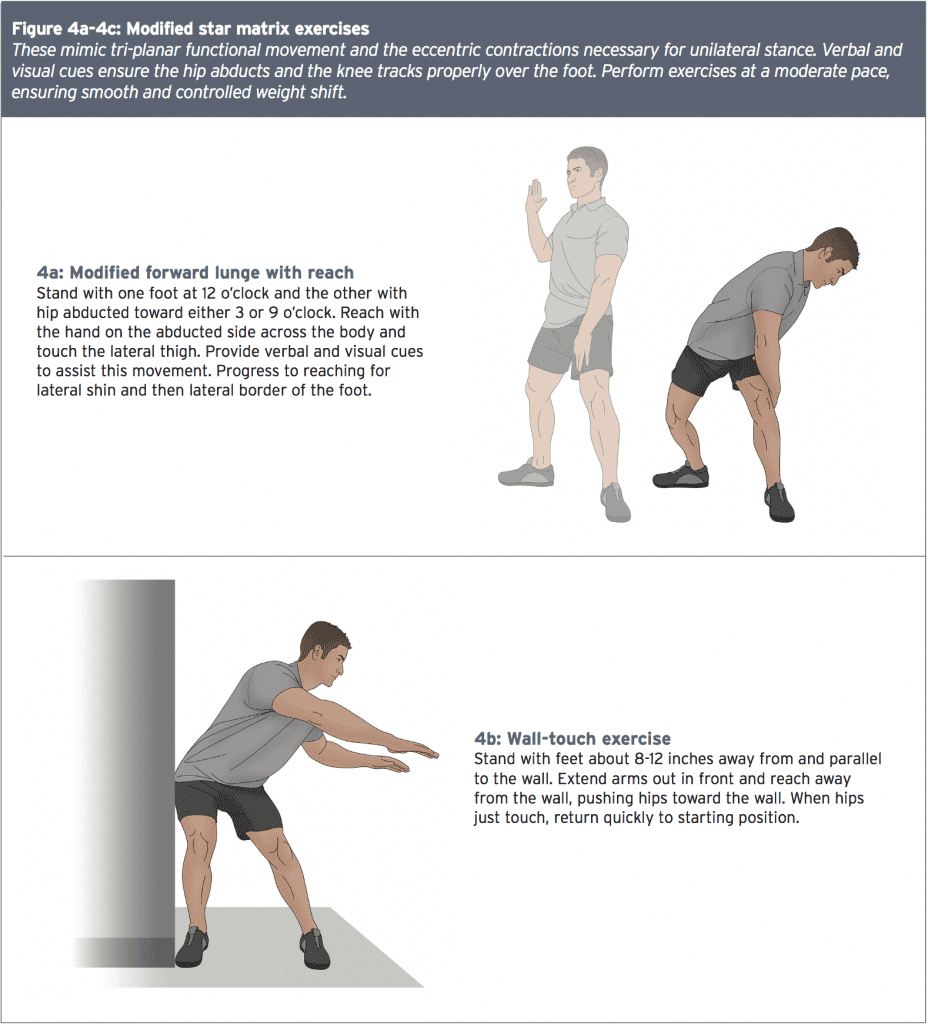
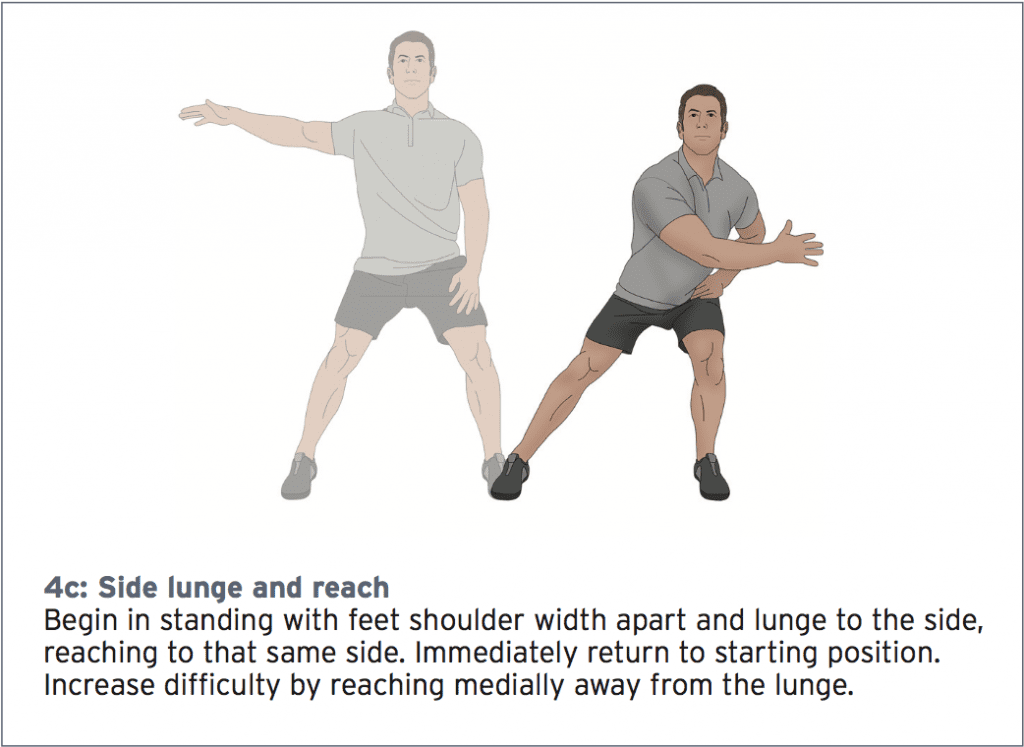
These mimic tri-planar functional movement and the eccentric contractions necessary for unilateral stance. Verbal and visual cues ensure the hip abducts and the knee tracks properly over the foot. Perform exercises at a moderate pace, ensuring smooth and controlled weight shift.
Return To Sport
Consider return to sport when the athlete demonstrates the following:- A negative Noble compression test
- Pain-free adduction with an Ober test
- Performs exercises without pain for two weeks(3)
Recommend short, easy sprints every other day for one week, followed by longer training runs on flat terrain every other day for two to three weeks. Progress distance by no more than ten percent each week.
For cyclists, the treatment course is the same; however advise return to sport only after a thorough evaluation of bike fit. Provide biofeedback and retraining using their road bike on a trainer. Lower the seat and raise the handlebars to decrease stress on the ITB and decrease strain on the gluteal muscles. Investigate cleat position, adjusting to mirror the athlete’s normal stance posture. Utilise a shoe lift or orthotics to correct leg length or foot deformities. With a functional approach to treatment, most athletes with ITBS return to sport in roughly six weeks.
For cyclists, the treatment course is the same; however advise return to sport only after a thorough evaluation of bike fit. Provide biofeedback and retraining using their road bike on a trainer. Lower the seat and raise the handlebars to decrease stress on the ITB and decrease strain on the gluteal muscles. Investigate cleat position, adjusting to mirror the athlete’s normal stance posture. Utilise a shoe lift or orthotics to correct leg length or foot deformities. With a functional approach to treatment, most athletes with ITBS return to sport in roughly six weeks.
References:
1. Sports Med. 2005;35(5):451-59
2. Sports Med. 2005;35(5):451-459
3. PM R. 2001;3:550-561
4. BioMechanics. 2006 Dec
5. Br J Sports Med. 2011 Jul;45(9):691-6
1. Sports Med. 2005;35(5):451-59
2. Sports Med. 2005;35(5):451-459
3. PM R. 2001;3:550-561
4. BioMechanics. 2006 Dec
5. Br J Sports Med. 2011 Jul;45(9):691-6




