Hyperextension knee injuries can differ from chronic to acute, depending on their severity, and these
are generally considered quite painful. The infrapatellar fat pad, abbreviated as IPFP, is one
of the most commonly affected structures due to hyperextension knee injuries.
In the presence of an acute knee hyperextension injury, for example, when an
athlete is tackled in rugby, the posterior cruciate ligament, or PCL and/or the
posterior lateral corner, or PLC, of the knee may become injured.
Infrapatellar Fat Pad
Anatomy
The
infrapatellar fat pad is identified as an extrasynovial structure which is
located on the anterior of the knee, away from the area of the patella. It’s
characterized as a mobile formation and its shape, volume and pressure is
altered with the movement of the knee. The infrapatellar fat pad attaches
anteriorly to the immediate patellar tendon and inferior pole of the patella,
posteriorly attaching to the intercondylar notch of the femur and in some
individuals, the ACL. It is a heavily vascularized structure, also innervated
by branches of the obturator, saphenous and the well-known peroneal nerve. The
fibres which denote pain from the stimulation of the nerve cells are most dense
in the central and lateral sections of the infrapatellar fat pad.
Mechanism of Injury
Injuries or
conditions affecting the infrapatellar fat pad may commonly result from a direct
blow or as a result of chronic irritation due to hyperextension knee injuries.
Both conditions present a series of painful symptoms which can be debilitating.
Individuals or athletes with these types of complications experience knees that
hyperextend and they may walk with poor quad control and knee hyperextension. The
IPFP, or infrapatellar fat pad, can also become injured as a result of direct
trauma to the knee, either through a blunt force or through shear injury along
with a patellar dislocation or ACL rupture.
Assessment
Individuals with hyperextension knee injuries
originating from infrapatellar fat pad issues often describe a sharp, burning
and/or aching deep pain on either side of the patellar tendon. Certain sports
or physical activities, including maximal knee extensions or basic activities
which require active knee extension, such as going upstairs or prolonged knee
flexion, may aggravate the symptoms of hyperextension knee injuries from the
IPFP.
Healthcare professionals may perform various clinical tests to diagnose
and set apart infrapatellar fat pad complications from other hyperextension
knee injuries.
Upon medical assessments, patients with IPFP disorders frequently
present swelling and inflammation along the bottom of the patella, displaying
the appearance of puffy knees.
Objective tests include: Hoffa’s test, performed where the infrapatellar
fat pad is palpated on either side of the patella tendon, with the knee in a
30-degree flexion. The knee is then fully and passively extended where
increased pain in the IPFP will indicate a positive test; the passive knee
extension test is performed by having the patient lie supine, where the knee is
passively extended. Pain along the bottom of the patella indicates a positive
test result; the differentiation test, as the name pertains, helps to
distinguish between infrapatellar fat pad and patellar tendon injuries and/or
conditions. Primarily, the location of most tenderness is palpated in 30-degree
knee flexion. The patient is then ordered to gently activate their quadriceps
muscle while the healthcare professional providing the test resists this
movement. The isometric activation of the quadriceps lifts the patellar tendon
off the IPFP, decreasing the symptoms on palpation.
Imaging
MRI is the most common modality of choice for suspected hyperextension
knee injuries to the infrapatellar fat pad. According to the results of an MRI,
increased T1 or T2 hypointense signals may conclude the thickening and scarring
of the connective tissue of the fat pad, also referred to as fibrosis, usually
the result of trauma from an injury. T2 weighted images which display
hypointense signals may demonstrate inflammation or acute hemorrhage or edema.
Treatment
Hyperextension knee injuries caused by disorders of the IPFP effective
respond to conservative treatments. The fundamental goal of treatment is to
reduce the stress and pressure being placed against the fat pad to decrease the
symptoms of pain as well as allow the quadriceps to regain their strength. Infrapatellar
fat pad deloading taping procedures should be taught to the affected
individuals to prevent continuous compression of the fat pad. Limiting the
athlete’s stance and gait must be suggested as early as possible to avoid
hyperextension knee injuries during these activities. Helpful exercises which
can further benefit throughout the rehabilitation process includes wall squats,
splits squats and lunges. Exercises which involve full knee extension should be
avoided. To re-train the muscles, quadriceps strengthening drills should
specifically be performed in closed kinetic chain positions.
Surgical procedures are rarely required but may include fat pad
excision, debridement, synovectomy, infrapatellar plica release and denervation
of the inferior pole of the patella.
Posterior Cruciate Ligament Injuries
The posterior cruciate ligament, or PCL, frequently becomes injured when
the knee is flexed, although, it can also be injured in hyperextension knee
injuries, such as a rugby tackle. Approximately 60 percent of PCL injuries also
affect the posterolateral corner, an increased estimate of injuries are
primarily involved with knee hyperextension.
Anatomy
The posterior cruciate ligament is also an extrasynovial structure which
functions to prevent the posterior shift of the tibia on the femur. It’s made
up of an anterolateral bundle which is most rigid during knee flexion and a
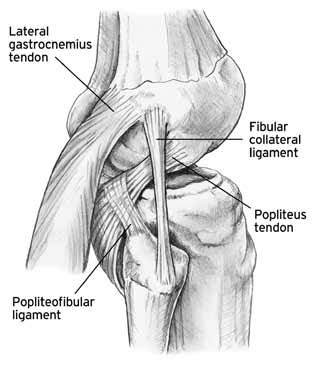
posteromedial bundle which is most rigid in extension. The posterolateral
corner consists of the popliteus muscle, the lateral collateral ligament, bicep
femoris tendons and the popliteofibular ligament. Isolated injuries to the
posterior cruciate ligament are rare but may be often associated with PCL
complications.
Assessment
Through diagnosis and evaluation of individuals or athletes with
posterior cruciate ligament injuries have been recorded with poorly defined
knee pain along with minimal swelling. Various assessments are utilized to
conclude the presence of injury to the PCL, including: posterior drawer, a test
which comprises of having the patient lying supine with the affected knee bent
to 90-degrees. The position of the tibia relative to the femur is recognized
and recorded by the healthcare professional providing the assessment, where a
posterior-positioned tibia indicates the presence of a posterior cruciate
ligament injury; with the posterior sag test, the patient lies supine with
their hips flexed to 90-degrees and their knees bent to 90-degrees as well. The
healthcare professional then supports under the lower calf of both legs,
looking for a posterior sag of the tibia; and finally, the quad contraction
test is used in the case that a posterior tibial translation is suspected while
the patient is supine and their knees are bent to 90-degrees. To perform this
test, the medical specialist holds the lower shin and asks the patient to
contract their quads. If a posterior sag is present, then, contraction of the
quadriceps will lead to an anterior shift of the tibia.
Posterior cruciate ligament injuries are classified from 1 to 3 and are preferably
measured with the knee in 90-degree flexion where the tibia normally lies 1 cm
anterior to the femoral condyles. The grading system is outlined as follows: G1,
where the tibia lies anteriorly to the femoral condyles, however, the distance
is reduced to 0-5mm; G2, where the tibia lies flush with the condyles; and G3,
where the tibia can be pushed beyond the medial femoral condyle.
As previously mentioned, injuries to the posterolateral corner may also
develop with the presence of an injury to the PCL, such as in the case of
hyperextension knee injuries. Various evaluation tests are characterized to
help determine whether a posterolateral corner injury is present, including:
the external rotation recurvatum, or hyperextension, test, performed where the
patient lies supine and the healthcare professional stabilizes the distal thigh
with one hand while lifting the great toe with the other. If the specialist
recognizes more hyperextension in the affected knee, then, a posterolateral corner
injury can be concluded; to perform the dial test, the patient must lie prone
with the knees flexed to 30-degrees. The healthcare professional then
externally rotates the tibia of both legs, making sure the thighs maintain a
stabilized position. A greater range of external rotation of more than
10-degrees represents a positive test result. This test can also be performed
with the knees flexed at 90-degrees and in the case of increased range, then, a
combined injury to the posterior cruciate ligament and PLC injuries are
suspected.
Gait evaluations should also be performed. Patients whom result with
instability on the posterolateral corner present varus gait at foot strike when
their knee is extended.
Imaging
Posterior cruciate ligament and posterior lateral corner injuries
commonly result due to an acute injury. In the case of a considerable acute
injury, X-rays may be requested to exclude the presence of a bony avulsion of
the PCL from its tibial insertion. If so, surgical intervention may be
necessary to repair this type of injury. MRI scans may also be useful in this
instance to help determine the presence of posterior cruciate ligament and
posterior lateral corner injuries.
Treatment
According to various treatment results, individuals and athletes with
isolated posterior cruciate ligament tears or ruptures experience an effective
functional outcome through a properly designed rehabilitation program, despite
of ongoing laxity. However, research studies have concluded that PCL
deficiencies do occur during increased pressure within the joints on both the
patellofemoral tibiofemoral joints. This may therefore indicate that meniscal
tears and articular damage to the medial compartments of the knee, may develop
gradually over time. If PCL injuries occur conjointly with the damage of other
structures of the knee, including PLC, or whether a considerable instability is
found, surgical interventions should be considered. An individual with a grade
3 PCL injury is recommended to participate in immobilized extensions for up to
two weeks. An individual with a grade 1 to 2 injury is recommended to
participate in a specific rehabilitation program with a focus on strengthening the
quadriceps.
Do You Need Surgery for a PCL Injury?
Many healthcare professionals specialize in the diagnosis and
rehabilitation of a variety of sports injuries, including hyperextension knee
injuries. Chiropractic care is a popular, alternative treatment option which
emphasizes on the overall health of the body through the proper alignment of
the spine and its surrounding structures, including the muscles, ligaments,
tendons, joints and other essential tissues. Chiropractors are also specialized
in evaluating many types of sports injuries. Once a doctor of chiropractic, or
DC, determines the presence and origin of an individual’s symptoms, they
commonly utilize a series of chiropractic adjustments to reduce the stress and
pressure around the complex structures of the injury, helping to decrease the
athlete’s pain and discomfort. Along with several other types of treatment
options, a chiropractor may also recommend a course of rehabilitation stretches
and exercises to improve an individual’s original strength, flexibility and
mobility as well as speed up the rehabilitation process.
Before engaging in a rehabilitation program, the individual or
athlete must primarily seek medical attention from a qualified healthcare professional who will follow up with the most appropriate group of exercises according to each individual’s grade of injury and needs. Advancing with a rehabilitation program will be commonly determined by the patient’s improved symptoms and therefore, should only be modified
by the specialist to avoid further injury.
By Dr. Alex Jimenez