Chiropractor, Dr. Alexander Jimenez investigates this very common knee injury...
Introduction
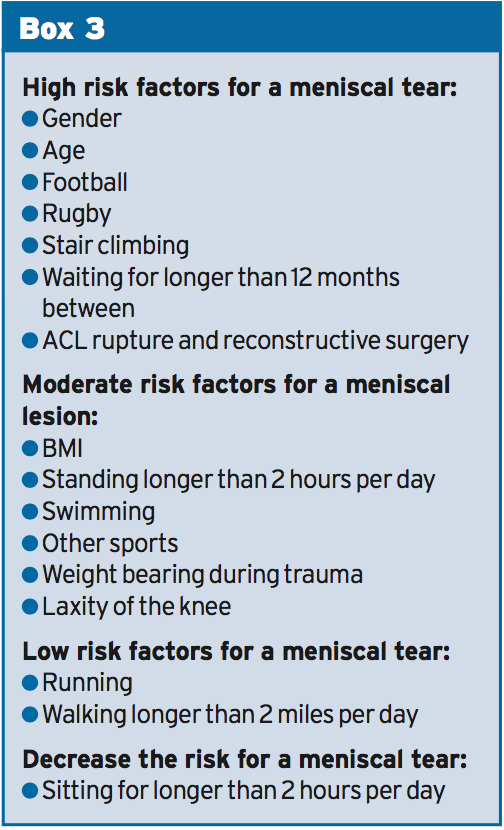
Meniscal tears can result in a great deal of time lost from bodily activity or employment, and therefore understanding the risk factors for meniscal tears may allow for a quicker and more accurate diagnosis. Meniscal lesions normally occur in the athletic arena as a result of dynamic demands placed on the knee through specific movements. Additional a meniscal tear can also result due to the numerous repetitive places continuing within the work area.Normal positions adopted in a work environment such as standing, lifting, squatting, kneeling and sitting have all been suggested to influence the danger of meniscal damage(2). Furthermore, the period between anterior cruciate ligament (ACL) rupture and surgical reconstruction has also been recognized as a risk factor for a meniscal lesion(3). Various risk factors are recognized to contribute to a meniscal lesion nonetheless, there is limited study within the literature to support them(4).
A systematic review, together with some meta-analysis, was published in 2013 by scientists in the University of Amsterdam(4) who investigated some of the key risk factors for meniscal tears. The purpose of the present review is to outline the findings based on a number of the articles which were included in that distinct systematic research review whilst also drawing on the results from other study also. Furthermore, the current review may also assist a physiotherapist or sports therapist within their own clinical evaluation by identifying key risk factors that may help form their identification.
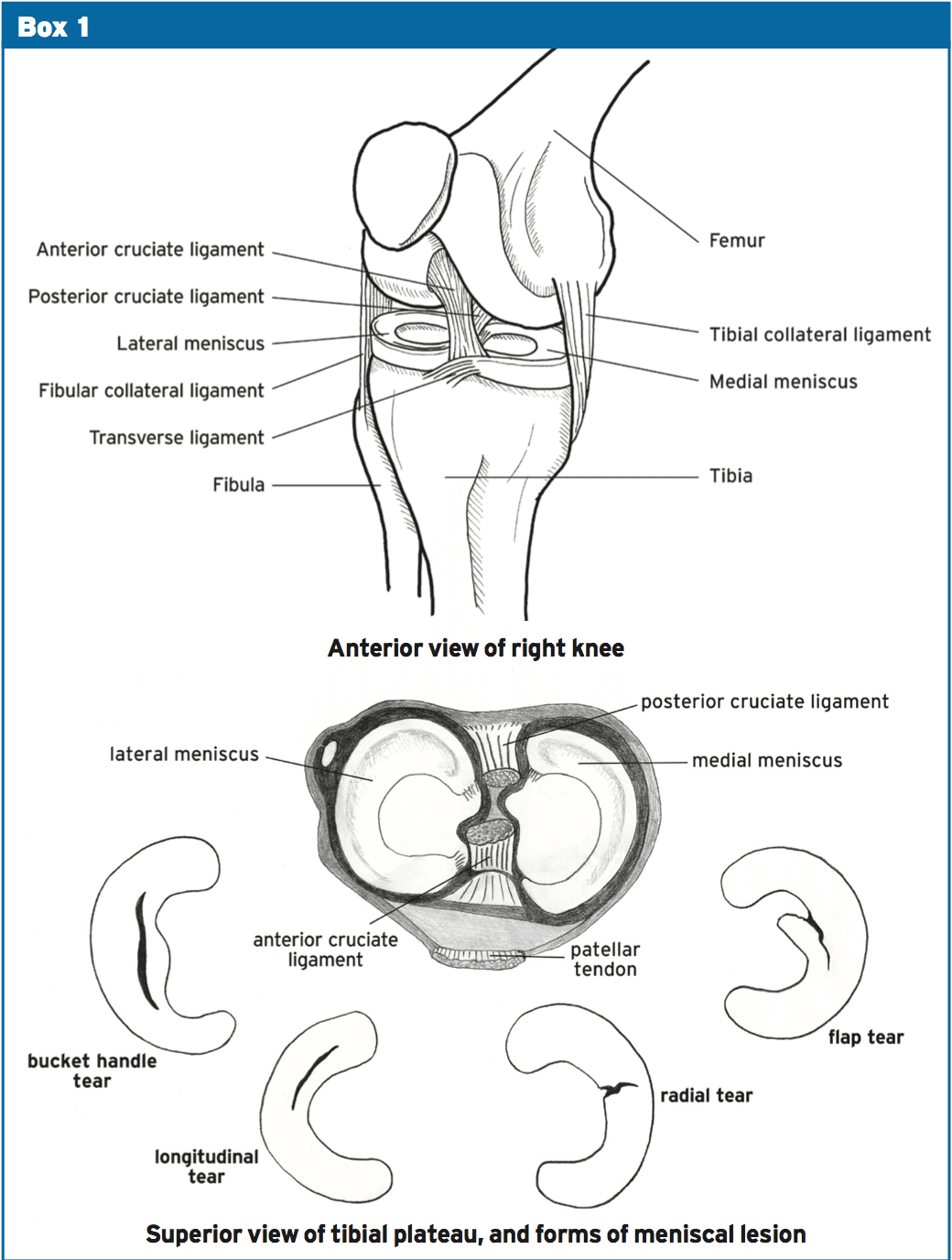
The menisci are just two semilunar form- like structures which sit positioned on the medial and lateral surface of the tibial plateau (see Box 1) (5). Additionally, the menisci allow the transference of weight and absorption of shock during dynamic motions, whilst acting to protect the articular cartilage(5). Meniscal lesions could be either acute or degenerative in nature and might present in different kinds, ie a bucket handle tear, a flat equilibrium or a degenerative tear.
Degenerative Risk Factors
Body mass index (BMI) was identified in 2 research studies and has been shown to be important with degenerative meniscal changes(4). Scientists from Boston University(5) analyzed the BMI of 991 (565 females and 426 men) participants also found that females with a meniscal tear had a significantly higher BMI (29.9) than females with no meniscal damage (27.9). It had been reasoned, through statistical analysis, that a BMI greater than 25 kg/m2 yielded a greater propensity for meniscal damage than people with a lower BMI(4). It is important to remember that this doesn't just involve those of more obese proportions but those who have a larger muscle mass therefore increased body mass too.Age is considered to be a significant risk factor as identified in 2 research(4). Researchers have(5) determined that the older the individual the higher the meniscal injury, for example 19 percent of females and 32% of males aged 50-59 had meniscal destruction(5). This is compared to 51 percent of guys and 56% males aged 70-90 years presenting with meniscal trauma. It was reasoned that individuals over 60 years of age were significantly more likely to sustain a degenerative meniscal tear compared to a person under 60 years of age(4 years). But, that doesn't suggest that a younger person can't maintain a meniscal lesion.
Gender is regarded as a three-fold risk factor for a meniscus tear in men as identified in three articles(4). Additional study completed at Boston University studied the connection between meniscal tears, pain and atherosclerosis in 154 patients symptomatic of knee osteoarthritis(7). The results obtained by MRI scans ascertained that 91 percent of individuals had a lateral or lateral meniscal tear and of this group males had a significantly greater incidence of meniscal lesions than females. The second study compared the qualities of meniscal lesions in 991 participants through MRI(5). Males again revealed significantly higher prevalence of meniscal tears in all age groups even though females combined with greater meniscal degeneration in the 70-90 years old class(5). Whether the greater incidence in men is due to greater participation in game or by occupational activities was not determined.
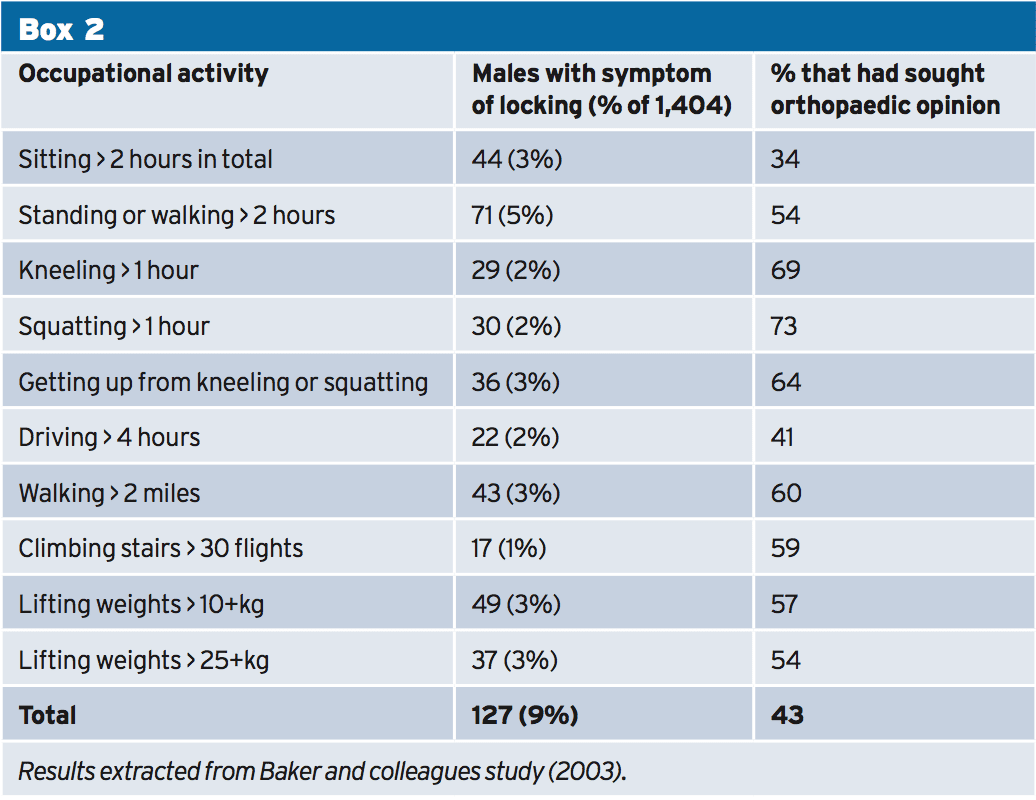
Kneeling and squatting in the office are often places adopted by those in certain professions or trades such as carpentry, electrician and pipes which are largely occupied by men. Three newspapers were identified that analyzed these sustained places and found that kneeling and squatting for longer than one hour per day is considered to be influential in the development of meniscal tears(4). Research carried out at Southampton University (England) found that 59 respondents experienced bending of their knee with 29 being exposed to kneeling and with 30 exposed to squatting in their workplace (see Box 2)(8). Of these 59 patients (several may cross over in both groups), 69 percent and 73% respectively had consulted with an orthopedic surgeon. These participants participated in repetitive kneeling and squatting through their job but had also reported participation in soccer too which is thought of as another risk factor.
Standing or walking for longer than two hours per day for 12 weeks ahead of the beginning of symptoms, in contrast to less than two hours per day, were regarded as influential in the growth of meniscal lesions. Two studies were found to have evaluated the effects of prolonged walking or standing(8), 9). The results found that from 71 patients that were subjected to prolonged walking or standing for longer than two hours every day, 54% had consulted an orthopedic surgeon with symptoms of meniscal damage (see Box 2). In contrast, standing and walking are considered to be effective from different perspectives in terms of energy expenditure, mechanical bone loading, cardiovascular fitness and general wellbeing and shouldn't be compromised unless symptoms decide.
Walking longer than two kilometers per day (in the 12 months before the onset of symptoms) was identified by 2 studies(8, 9) where this variable was thought of as a very low risk for a meniscal lesion(4).) Again, the health benefits of walking outweigh the probability of meniscal lesions, and should not be negotiated unless symptoms prevent.
Climbing more than 30 flights of stairs every day (in the 12 months before the beginning of symptoms) has been contrasted by two studies(8, 9). 17 male patients complained of meniscal-related symptoms (locking) on stair climbing using 59 percent resulting in a consultation with an orthopedic surgeon (see Box 2)(8).
Snoeker and coworkers(4) concluded that there was a significant effect that lifting or carrying in excess of 10kg, 25kg and 50kg more than 10 times each week substantially increased the risk of a meniscal lesion.
The incidence of degenerative or acute meniscal lesions have been investigated(8) and have been known to frequently in the present study. This research study contacted a community sample of 2,806 men, at the south of England, by way of a questionnaire. Of the sample contacted, 1,404 reacted with 762 having complained of past knee-related symptoms. Of the 762 patients with symptomatic knees, 127 had reported symptoms of bending during one or more of the occupational pursuits that had lasted for longer than 24 hours (see Box 2). It was considered important to illustrate the findings in this particular study as we're all exposed to these activities of daily living to some extent(8). This ascertains the risk of a potential meniscal lesion inside the 20-59 age bracket.
Acute Risk Factors
Weight posture during injury is considered to be a moderate risk factor for the incidence of meniscal tears that was identified in one study(4). Researchers from Lund University in Sweden(11) ascertained that patients using an ACL injury who participated in non-weight posture were not as likely to maintain meniscal damage. Frequently ACL trauma is continuing in load bearing positions leading to greater joint compression forces of the tibio-femoral compartment and therefore the well-known term 'miserable triad' has more suitably been termed 'the unhappy compression' harm(11). It is essential to stabilize the knee joint during conservative or surgical ways to prevent further compression to the meniscus. It was concluded that weight bearing during trauma exposed a moderate threat to meniscal trauma but the authors were not able to decide whether a substantial effect existed(4).Sport in general is regarded as a relatively large risk factor for meniscal lesions(4). Two studies were identified that analyzed the prevalence of meniscus damage during football, rugby, swimming and running(8,9). Soccer and rugby were concluded to be major risk factors in the incidence of meniscal damage(4). Compared swimming and 'other sports' (Snoeker and colleagues(4) did not determine which athletics) were thought of as moderate risk factors in the incidence of meniscal tears(4). What's more, there was a paucity of evidence available for running to be regarded as a risk factor for meniscal damage(4). It is not hard to appreciate why soccer and rugby expose a knee to higher meniscus trauma due to the demands of this transference of mass and the rotational forces implemented.
Anterior cruciate ligament injury followed by a protracted interval until cosmetic surgery has been well recorded to induce a patient to meniscus damage(3). An ACL-deficient knee demands the menisci to be a stabilizing component in the posterior-anterior, valgus-varus and internal and external rotation movements(12). Snoeker and colleagues(4) research coincided with previous research, in that the ACL deficient knee vulnerable a threat to meniscus trauma but recognized that this was in agreement with the medial, but not lateral meniscus. The authors said the reason for this shift in consistency was a result of the medial meniscus being repaired to the joint capsule. In contrast, the lateral meniscus isn't firmly attached to the joint capsule and so possesses more freedom within the joint which explains this gap in injury occurrence(4).
It was identified that by 3,475 patients having a history of ACL injury that 1,638 (47 percent) had presented with a meniscal tear(3). The authors added that for each month that passed after ACL rupture there was exponential risk of 1 percent of meniscal injury. In addition, the presence of a degenerative meniscal lesion demonstrated with 1.6-2.0% heightened risk of sustaining additional trauma to the knee.
Overview
The current review according to Snoeker and colleagues'(4) systematic review has identified a number of factors which could predispose someone to a greater incidence of meniscal injury. A meniscal lesion could be sustained amongst a broad population and should not be ruled out in any 1 sub-group based on the analysis presented. However, those risk factors identified could predispose an individual to higher chance of a meniscal lesion. Even though the study by Snoeker and colleagues is very recently published and covers a large number of risk factors, the study is extremely restricted due to some factors just being supported by just one or two studies.References
1. Open Acc J of Sports Med, 2010, 1: 45-54.
2. J Occup Rehabil, 2010, 20: 489-501.
3. The Am J Sports Med, 2009, 37 (5): 955-961.
4. J Orthop Sports Phys Ther, 2013, 43 (6): 352-367.
5. N Engl J Med, 2008, 359: 11, 1108-1115.
6. Skeletal Radiol, 2012, 41: 633-641.
7. J Bone Joint Surg Am, 2003, 01;85(1):4-9
8. Occup Environ Med, 2003; 60:794–797
9. J Rheumatol, 2002, 29: 557-563
10. Am Family Phys, 2007, 15, 75 (2), 194-202
11. Knee Surg Sports Traumatol Arthrosc, 1995, 3:144-147.
12. Clin Sports Med, 1993, 12 (4): 771-796.