In the first of a two-part article, scientific injury chiropractor, Dr. Alexander Jimenez explains the anatomy and biomechanics of the medial knee ligaments, the consequences of injury, and how these injuries are identified and graded.
The shallow lateral collateral ligament (s-MCL) is among the most commonly injured structures in the knee, in both contact sports and sports that involve sharp cutting and direction changes. It might also be associated with more serious injuries to the medial knee including deep lateral collateral ligaments (d-MCL) and posterior oblique ligament(1-6).
The vast majority of MCL tears are isolated. These injuries occur predominantly in young individuals participating in sports activities, together with the mechanism of harm between valgus knee loading, external rotation, or a combination of these. These are common in sports as skiing, ice hockey, rugby and football, all of which involve motions requiring knee flexion and valgus loading and potential of direct contact to the outside of the knee(7-9).
The treatment of medial-sided knee injuries has moved away from competitive surgical remedies to largely non-operative management. Surgery is generally reserved for chronic MCL lack that has neglected non-operative therapy, or more acute and intricate injuries. The vast majority of athletes who sustain an MCL injury will reach their pre-injury action level with non-operative treatment.
Anatomy
The iconic anatomy reference point for understanding that the lateral knee joint stabilisers comes from Stan James in Iowa State University, who performed a very thorough dissection study about the lateral knee joint at the 1970s(10). The medial knee was divided into dynamic and static stabilizers:
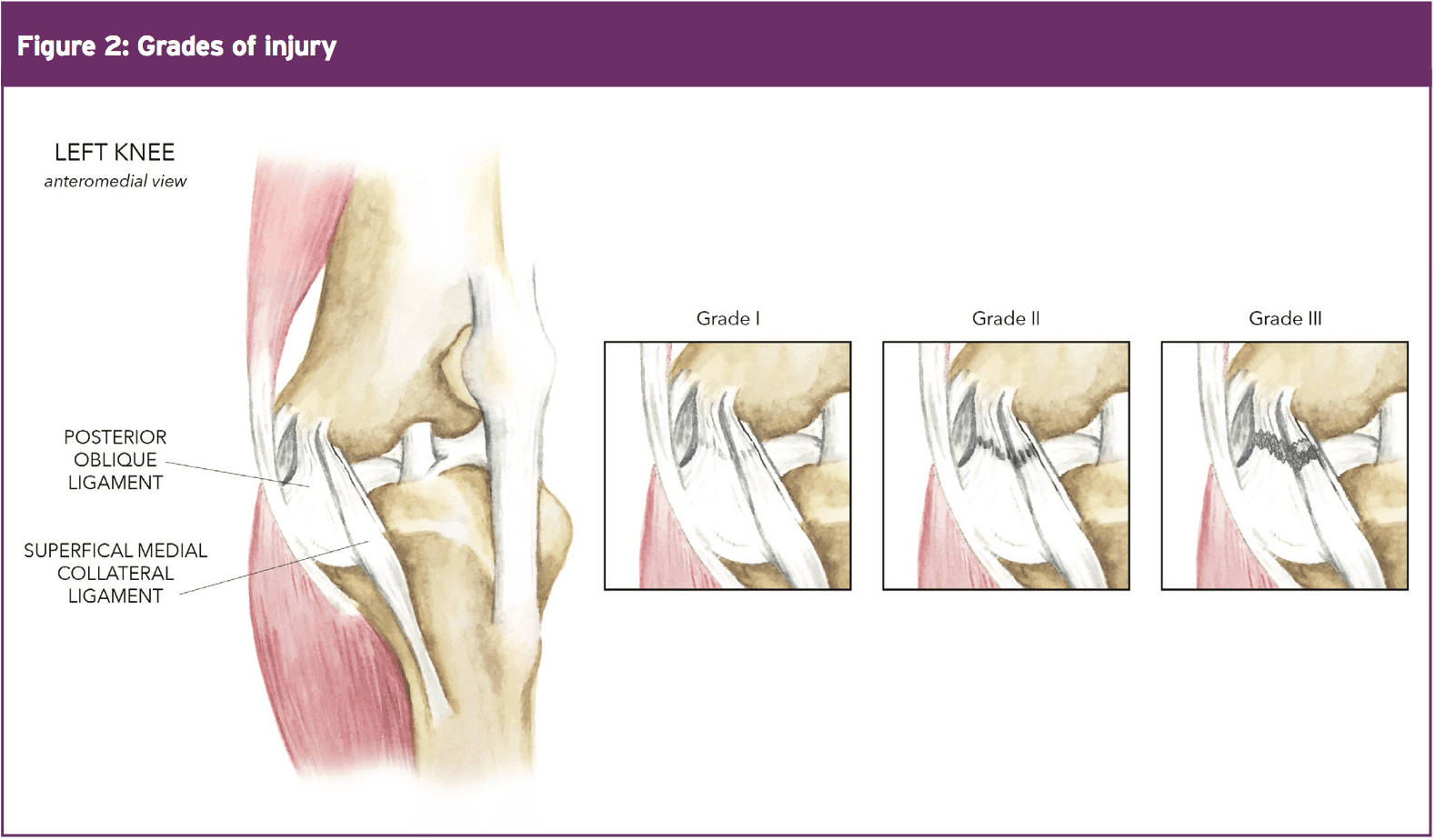
1. The static stabilisers of the medial knee include the superficial MCL (s-MCL), the deep MCL (d-MCL) or medial capsular ligament, and the posterior oblique ligament(5, 10).
2. Dynamic stabilisers include the musculotendinous units of the semimembranosus, quadriceps, and the combined tendon of the semitendinosis, gracilis and sartorious (pes anserinus(10)). The semimembranosus plays a significant role in the dynamic stability of the medial side of the knee. It achieves this by tightening the normally lax posterior oblique ligament, while posteriorly displacing the posterior horn of the medial meniscus to prevent impingement during knee flexion(11). Furthermore, the quadriceps and pes anserinus complex may potentially increase the effective stiffness of the MCL complex of the knee by 164 percent and 108 percent respectively(12).
The anatomy is described as having three layers: superficial (I), intermediate (II), and deep (III)(13, 14):
- The superficial layer (I) consists of the deep crural fascia, which invests the sartorius and quadriceps and continues into the deep fascia of the lower extremity to cover the gastrocnemius and popliteal fossa.
- The intermediate layer (II) comprises the s-MCL and medial patellofemoral ligament (MPFL).
- The deep layer (III) includes the joint capsule and d-MCL. A bursa separates the d-MCL and s-MCL, and is biomechanically important by allowing anteroposterior excursion of the s-MCL during flexion and extension(15).
Superficial Medial Collateral Ligament
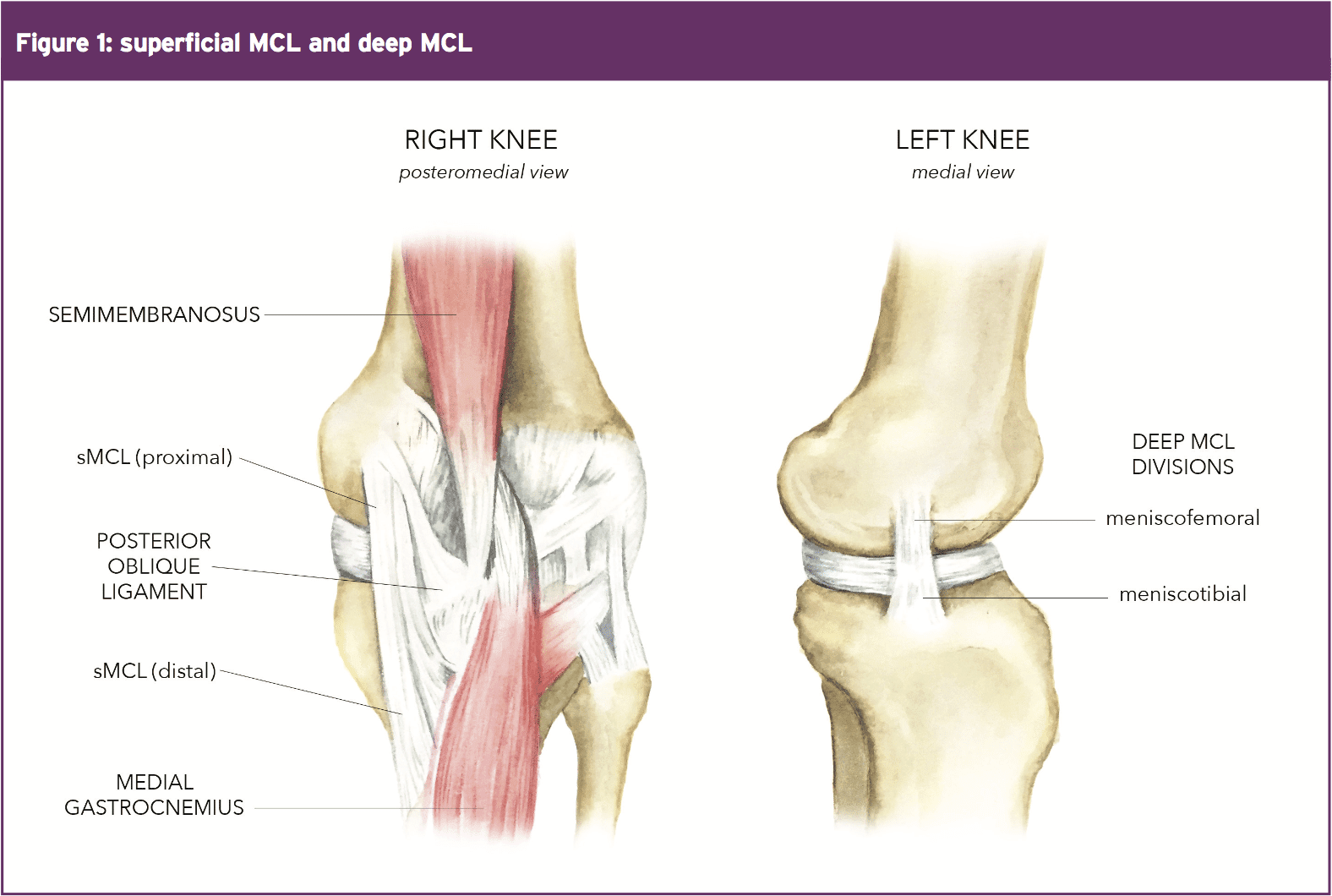
LaPrade et al 2007 have made the most comprehensive examination to date on the s-MCL(18). They claim the s-MCL is the most significant structure of this medial part of the knee (see figure 1). It's one rectal attachment and 2 tibial attachments(18). The femoral attachment is oval in shape and, on the average, 3.2mm proximal and 4.8millimeter lateral to the medial epicondyle.A more recent study by Liu et al discovered that the s-MCL was triangular in form and the proximal and distal components were composed of parallel fibers. By comparison, the middle area of the s-MCL consists of parallel and oblique fibers, along with the middle portion was 1.7 times wider than the proximal/distal components(20). It's would be interesting to note if the 'oblique' fibers in this study refer to the posterior oblique ligament, which is discussed further below, and numerous authors have made this identical point(13, 14, 21,22).
Deep Medial Collateral Ligament
Deep into the s-MCL is that the d-MCL, which is comprised of this thickened medial aspect of the joint capsule. It is divided into meniscofemoral (MFL) and meniscotibial (MTL) parts (figure 1) and can be firmly attached to the medial meniscus at the joint line(20)The bigger, but thinner MFL has a slightly curved convex attachment 12.6 mm distal and profound into the femoral attachment of this s-MCL. The MFL is about three times more than the MTL(20). The MTL attaches just distal to the edge of the articular cartilage of the medial tibial plateau, 3.2 mm distal to the lateral joint line,and9.0mmproximaltotheproximal tibial attachment of the s-MCL(18), also is 1.7 times wider than the MFL(20). It has also been reported that that the MFL attaches deep into the s-MCL, and the MTL attaches just distal to the tibial articular surface(25, 27). The d-MCL might play an important part to anchor the peripheral parts of the lateral meniscus in the medial side of the knee(20).
Relevant Biomechanics
The s-MCL is the primary restraint to valgus laxity of the knee and at 25 degrees flexion it provides 78 percent of the valgus controlling force(1,2,28-30). At this angle of flexion, the posterior oblique ligament gets lax and does not provide valgus support. In total extension, the ACL, posteromedial corner and semimembranosus bring about valgus restraint and the s-MCL only provides 57% of the controlling force(1,2). In general, an isolated s-MCL tear contributes to valgus laxity in flexion, whereas additional injury to the secondary valgus restraints (posterior oblique ligament or ACL) contributes to greater laxity in extension.The posterior thoracic fascia acts as a stabilizer of the two inner rotation and valgus movement at between 0 and 30 degrees of knee flexion(1-4,19,31-35). With the tibia internally rotated at 0 degrees flexion, the loads on the anterior oblique ligament are considerably greater than those on either branch of their s-MCL, which can be tauter in external rotation(19). Furthermore, the load reaction involving the anterior oblique ligament and s-MCL is reciprocal since the knee approaches 90 degrees flexion.
Also of interest is the fact that if d-MCL and s-MCL are surgically cut, significant gains in force are advocated by the posterior oblique ligament under valgus loads at 0, 20 and 30 degrees of knee flexion(36). As a result, the posterior oblique ligament in complete knees experiences tensile load using valgus forces, particularly near knee extension(19,36), and it also has a secondary function in supplying valgus stability of the knee(13,14,31,36).
The operation of the d-MCL (both the MTL and MFL) is poorly understood in comparison to the s-MCL. Its specific role is to function as a secondary stabilizer of the knee to valgus load(35,36). Valgus stabilization is offered by the MFL part at all tested flexion angles. The MTL portion stabilizes mostly at 60 degrees of knee flexion. The d-MCL provides restraint against external rotation torque in knees flexed between 30 and 90 degrees(36).
In studies, It's Been found that the maximum load to failure to the three structures were as follows(36):
- s-MCL -- 534 Newtons
- d-MCL -- 194 Newtons
- Posterior oblique ligament -- 425 Newtons
- The location of maximum strain of the entire medial collateral complex from cadaver studies was found to be near the femoral insertion when the knee was in full extension(36).
- Other clinical and laboratory studies suggest that the femoral insertion is the most common location for MCL injury(37-39).
- However, intraoperative findings have found that the tibial attachment is the most common injury site for the s-MCL, and the femoral attachment as the most common injury site for the d-MCL and the posterior oblique ligament(11,40).
- Finally, Hughston et al demonstrated that the tibial insertion was the most common site of injury for all the components of the MCL complex(3).
Injury Classification
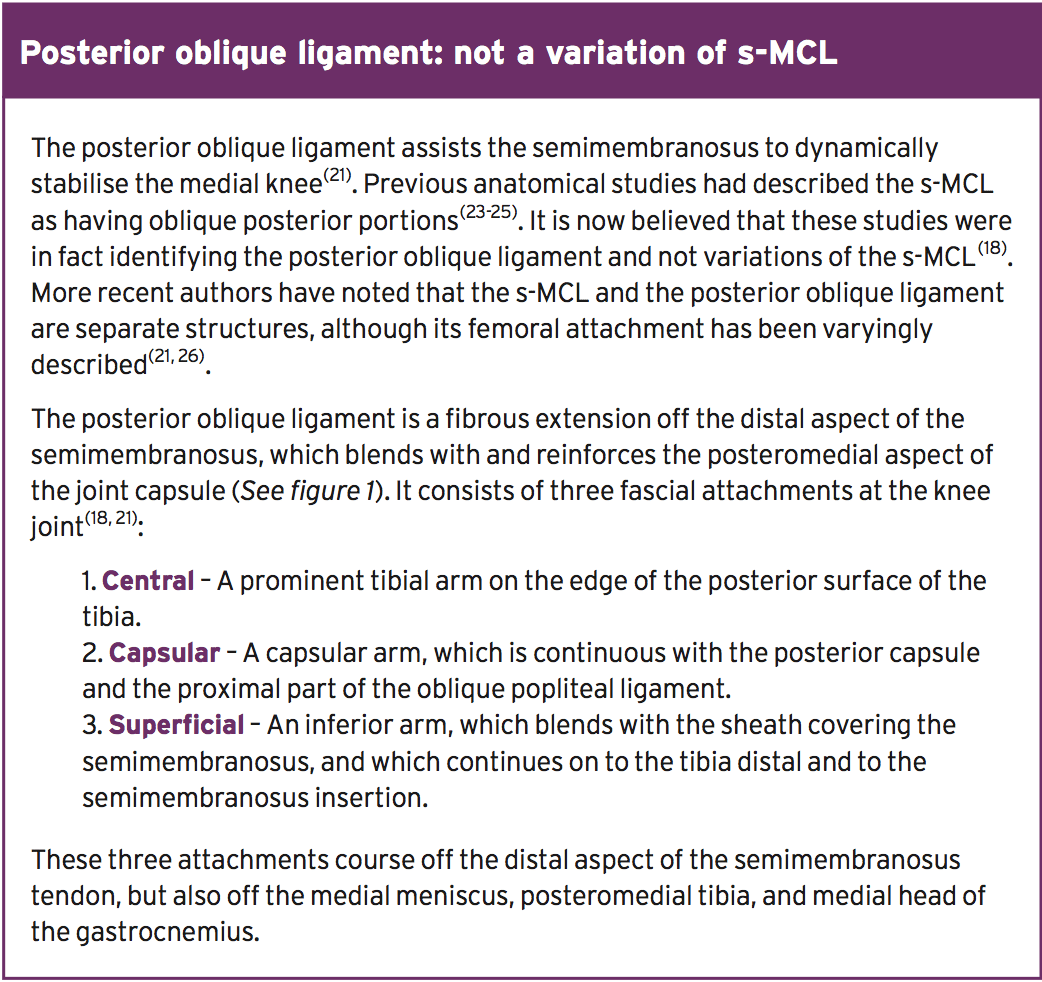
The time-honored type of grading ligament injuries is derived from the American Medical Association Standard Nomenclature of Athletic Injuries (see figure 2)(41). Inside this naming method:
1. Isolated grade-I first-degree tear presents with localised tenderness and no laxity.
2. Isolated grade-II, second-degree tear presents with localised tenderness and partially torn medial collateral and posterior oblique fibres. The fibres are still opposed, and there may or may not be pathologic laxity.
3. Isolated grade-III, third-degree tears present with complete disruption and laxity with an applied valgus stress.
2. Isolated grade-II, second-degree tear presents with localised tenderness and partially torn medial collateral and posterior oblique fibres. The fibres are still opposed, and there may or may not be pathologic laxity.
3. Isolated grade-III, third-degree tears present with complete disruption and laxity with an applied valgus stress.
Isolated medial knee injuries have also been classified in accordance with the amount of laxity observed at 30 degrees of knee flexion with a valgus applied moment compared to the uninjured limb(5,42,43):
1. Grade 1 (3-5mm)
2. Grade 2 (6-10mm
3. Grade 3 (more than 10 mm)
Fetto and Marshall have a different classification system(44):
1. Grade I injuries as those without valgus laxity in both 0 and 30 degrees of flexion.
2. Grade II injuries as those with valgus laxity in 30 degrees of flexion but stable in 0 degrees of flexion.
3. Grade III as those with valgus laxity in both 0 and 30 degrees of flexion.
It's important to perform valgus stress testing in 0 degrees of flexion, which is different from in full extension. In full extension (almost hyperextension), there's recruitment of ACL function that may hide the laxity of the entire medial-sided injury. There is a high prevalence of associated ligamentous injuries with ACL injuries in grade III cases using this classification method.
Clinical Assessment
History
The traditional mechanism of trauma reported is a sudden touch or non-contact valgus force to the knee with swelling and pain along the medial aspect of the knee. They may feel a tearing feeling with acute pain or in acute cases of rupture could hear a pop up. Those with low grade medial knee injuries involving either the s-MCL, posterior oblique ligament or d-MCL may try to continue competing. However, they often described a side-to-side feeling of uncertainty, particularly when doing pruning and cutting maneuvers.Clinical Evaluation
The key features that may be found clinically are(18):- Swelling over the medial side of the knee.
- Tenderness on palpation at the tibial or femoral insertions of the s-MCL.
- Tenderness on palpation along the medial joint line with the d-MCL.
- Valgus laxity and end point feel at 0 degrees full extension and 30 degrees knee flexion. If there is increased laxity at 30 degrees but not at 0 degrees, then the posterior oblique ligament is most likely still intact. However the ACL may still mask an instability at full extension.
- Laxity at 0 degrees flexion (not quite full hyperextension) would indicate that this would be a Fetto and Marshall grade-3 injury indicating damage to the posterior oblique ligament and posteromedial capsule(44).
- A complete injury to the medial structures will cause increased external rotation at both 30 degrees and 90 degrees of knee flexion, resulting in a positive dial test(1,2,19). Therefore, careful correlation with the results of valgus stress testing and assessment of the location of tibial subluxation during the dial test are necessary to exclude the possibility of a posterolateral, rather than a medial knee injury.
Stress Testing
With the patient lying supine, the assessor grasps the ankle with one hand and places another hand on the outside of the thigh above the knee. A gentle outward force is put on the ankle. This can be achieved at full extension, 0 degrees flexion and 30 degrees flexion:- At full extension, this assesses the s-MCL and d-MCL, the posteromedial capsule, the posterior oblique ligament and the ACL and PCL.
- At 0 degrees flexion, the posteromedial capsule and ACL and PCL are taken off slight stretch.
- At 30 degrees flexion, the s-MCL is the primary restraint to valgus stress.
Imaging
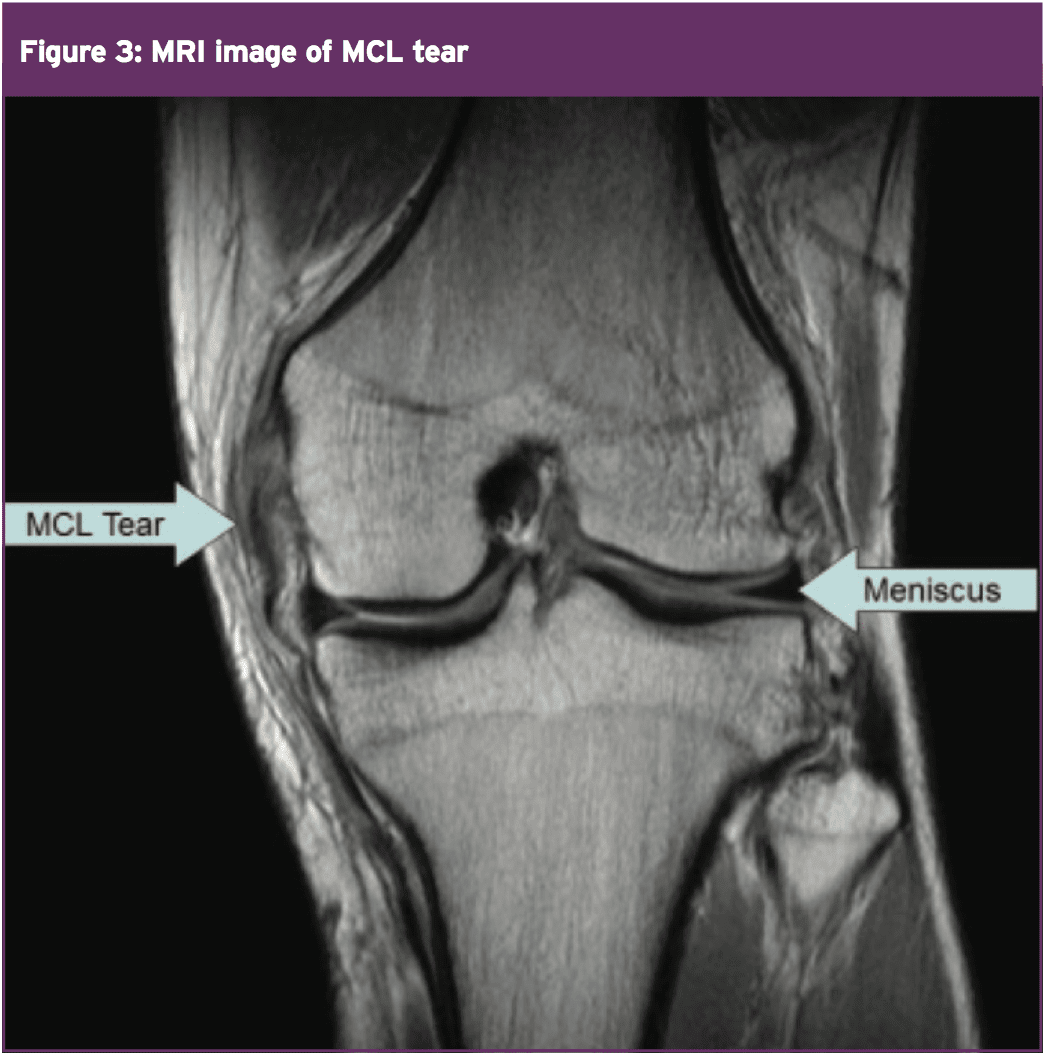
Plain film X-rays are often unnecessary unless the clinician would like to appraise the degree of gapping of the medial joint line under imaging. In 1 study, a load applied by a clinician into a knee with a simulated isolated tier III s-MCL injury increased medial joint gapping, compared with that in the intact knee, by 1.7 and 3.2mm at 0 and 20 degrees of flexion, respectively(45). A complete lateral knee trauma, with sectioning of this s-MCL and d-MCL and the anterior oblique ligament, increased gapping by 6.5 and 9.8mm at 0 and 20 degrees of flexion respectively, below the clinician-applied load (45).Magnetic resonance imaging (MRI) is more commonly used to assess the involved structures in patients with injuries to the medial side of the knee (see figure 3). T2-weighted MRI is the gold standard for diagnosing both partial and complete tears of this s-MCL. MRI has an accuracy of 87 percent for the assessment of MCL accidents(46).
Aspects Of Healing
Studies of the variables involved with the healing of this s-MCL in animals have shown that the healing is location dependent and immobilization dependent:
1. Injuries to the attachment sites take longer to heal than mid-substance injury(47).
2. In a rabbit model, a reduction of collagen mass and increased collagen degradation were observed after twelve weeks of immobilization(48).
3. Immobilization leads to disorganization of collagen fibrils, a decrease in the structural properties of the bone- ligament-bone complex, and resorption of bone at ligament insertion sites(49).
4. These negative effects of immobilization were believed to be caused by collagen matrix reorganization and tissue catabolism within the MCL after injury(50,51).
5. In another study performed on dogs that had undergone surgical transection of the s-MCL(49) it was found that in the three groups: early motion, immobilization for three weeks, and immobilization for six weeks, the early motion protocols led to enhanced healing and improved biomechanical properties of the s-MCL.
2. In a rabbit model, a reduction of collagen mass and increased collagen degradation were observed after twelve weeks of immobilization(48).
3. Immobilization leads to disorganization of collagen fibrils, a decrease in the structural properties of the bone- ligament-bone complex, and resorption of bone at ligament insertion sites(49).
4. These negative effects of immobilization were believed to be caused by collagen matrix reorganization and tissue catabolism within the MCL after injury(50,51).
5. In another study performed on dogs that had undergone surgical transection of the s-MCL(49) it was found that in the three groups: early motion, immobilization for three weeks, and immobilization for six weeks, the early motion protocols led to enhanced healing and improved biomechanical properties of the s-MCL.
Conclusion
MCL injuries are a common occurrence in sports which require sharp cutting and changing directions, and in contact sports.The anatomy of the medial side of the knee is pretty intricate and composed of the static stabilizers such as the s-MCL, d-MCL, posterior oblique ligament and the posteromedial capsule. It is encouraged by the energetic stabilizers, the muscles. Injuries to the inside of the knee predominately demand the s-MCL. This is ideally tested with a 30-degree valgus stress test and could be confirmed on MRI. Direction of grade 1-2, and most grade 3 injuries involves brace immobilization and conservative direction. Surgery is reserved for severe and complicated ligament disruptions or even in the case of chronic valgus instability. Part two of the report will discuss in detail the conservative progression following injury to the s-MCL.
References
1. J Bone Joint Surg Am. 1981;63:1257-69
2. J Bone Joint Surg Am. 1988;70:88-97
3. J Bone Joint Surg Am 1976;58(2): 159-72
4. J Bone Joint Surg Am. 1994;76:1328-44
5. Iowa Orthop J. 2006;26:77-90
6. Rheumatology (Oxford). 2006;45:595-9
7. Am J Sports Med. 1995;23: 597-600
8. Am J Sports Med. 1988;16:392-6
9. Am J Sports Med. 2000;28(5 Suppl):S51-7
10. Fortschr Med 1978;96(4):141-6,166
11. Am J Sports Med 2004;32(2):337-45
12. J Bone Joint Surg Am 1979;61(3):398-402
13. J Bone Joint Surg Am Vol 1979;61(1):56–62
14. J Bone Joint Surg Am. 1974;56:665-74
15. Orthop Rev. 1989;18:947-52
16. J Bone Joint Surg Am. 1983;65:323-9
17. Clin Orthop Relat Res. 1990;256:174-7
18. J Bone Joint Surg Am. 2007;89: 2000-10
19. Am J Sports Med. 2009;37:140-8
20. Journal of Orthopaedic Surgery and Research 2010, 5:6
21. J Bone Joint Surg Am 1973;55(5):923-40
22. J Bone Joint Surg Br.1948; 30:683-8
23. J Bone Joint Surg Am. 1943; 25:121-31
24. J Bone Joint Surg Am. 1941;23:44-66
25. J Bone Joint Surg Am. 1968;50: 211-25
26. AmJ Sports Med. 1985;13:390-7
27. Radiographics. 2000;20 Spec No:S83-9
28. J Bone Joint Surg Am. 1944;26:503-21
29. Acta Orthop Scand. 1965;36:179-91
30. Clin Orthop Relat Res. 1995;321:3-9
31. Am J Sports Med. 1994;22:402-9
32. Am J Sports Med. 1977;5:144-53
33. Acta Orthop Scand. 1984;55:30-4
34. Arch Orthop Trauma Surg. 1984;103:165-9
35. Am J Sports Med. 2009;37:1771-6
36. Am J Sports Med. 2006;34:1815-23
37. J Orthop Res 2003;21(6): 1098-106
38. Med Eng Phys 1999;21(5):279-91
39. Am J Sports Med 2003;31(2):261-7
40. Clin Orthop 1991;(271):3-8
41. American Medical Association; 1966. p 99-100
42. Sports Med Arthrosc. 2006; 14:12-9
43. Prim Care. 2004;31:957-75, ix
44. Clin Orthop 1978;132:206-18
45. Am J Sports Med. 2010;38:330-8
46. Skeletal Radiol. 1994;23:521-4
47. Acta Orthop Scand. 1995;66:455-62
48. Clin Orthop Relat Res. 1983;172: 265-70
49. J Orthop Res. 1983;1:22-9
50. J Orthop Res. 1992;10:895-900
51. Clin Orthop Relat Res. 1992;277:277-88