Injury specialist, Dr. Alexander Jimenez looks at the latest study about concussion in sports, especially regarding early/on-field assessment and diagnosis of this condition.
The proper medical definition of concussion is: a clinical syndrome characterized by immediate and transient change in brain function, including alteration of mental illness and level of consciousness, resulting from mechanical pressure or injury. But, it is more commonly described as an injury to the brain caused by a blow to the head (eg an uppercut in boxing, a clash of heads in soccer or a fisherman moving over the handlebars on the ground etc), which leads to temporary loss of normal brain function, including disturbances in memory, judgment, reflexes, speech, balance and muscle coordination. A less obvious cause is an indirect blow where the force is transmitted up to the head from a different portion of the body -- for example when a stationary rugby player is tackled from behind causing his head to abruptly flick back, with a number of the force of the tackle passing through his brain; the participant may end up concussed without ever taking a direct blow to the head.
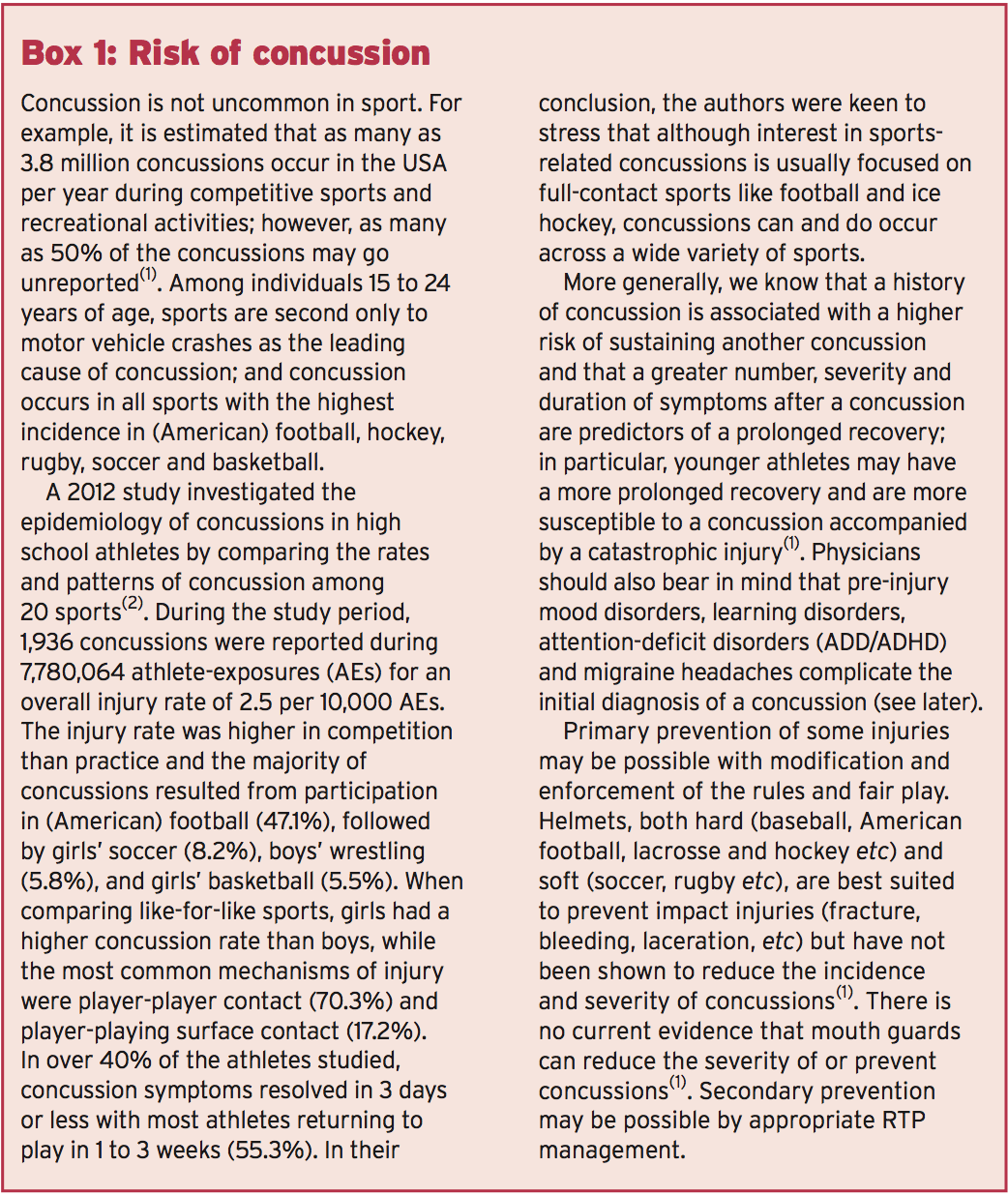
While bruises and cuts might be present on your face or head as a consequence of this blow, in most cases a person with a concussion never loses consciousness. Because of this, less experienced coaches and sports physicians may not immediately assume concussion, or if they do they presume that it's unlikely to be a cause for concern. But, though some concussions are less severe than others, there's absolutely no such thing as a 'minor concussion'; while a single concussion should not result in permanent damage, another concussion shortly after the initial one doesn't have to be very powerful for its consequences to be fatal or permanently disabling. Animal and human studies support the concept of this so-called 'post-concussive vulnerability', showing that a second blow before the mind has regained results in worsening metabolic changes within the cell(1). This explains the crucial importance of correctly and immediately identifying when a concussion has occurred because it affords the opportunity of this athlete to be taken out of the field of play, thereby ensuring a second concussion cannot happen.
Initial Diagnosis Of Concussion
As soon as an athlete suffers a blow to the head, the first priority should be that someone qualified is available to assess whether concussion has occurred. In an ideal world, this assessment could always be performed by a physician specifically trained in this area. In many sporting events (eg a small league football game), it is unlikely that such a individual will be there standing on the sidelines. However, as stated by the America Medical Society for Sports Medicine (AMSSM), the competence to execute this assessment also needs to be decided by training and experience and not purely dictated by specialty(1). To put it differently, with the right training and expertise, coaches, trainers and health care professionals are more than capable to perform a concussion examination.The AMSSM additionally points out that the identification of concussion is ideally created by a healthcare provider who is not only knowledgeable in the recognition and analysis of concussion but also familiar with the person concerned. The reason for this is that while standardized sideline tests are a useful framework for making an appraisal, the validity and reliability of these tests are greatly reduced without some type of individual baseline test result with which to compare, and some other baseline rating will vary based on the individual athlete concerned.
AMSSM New Guidelines
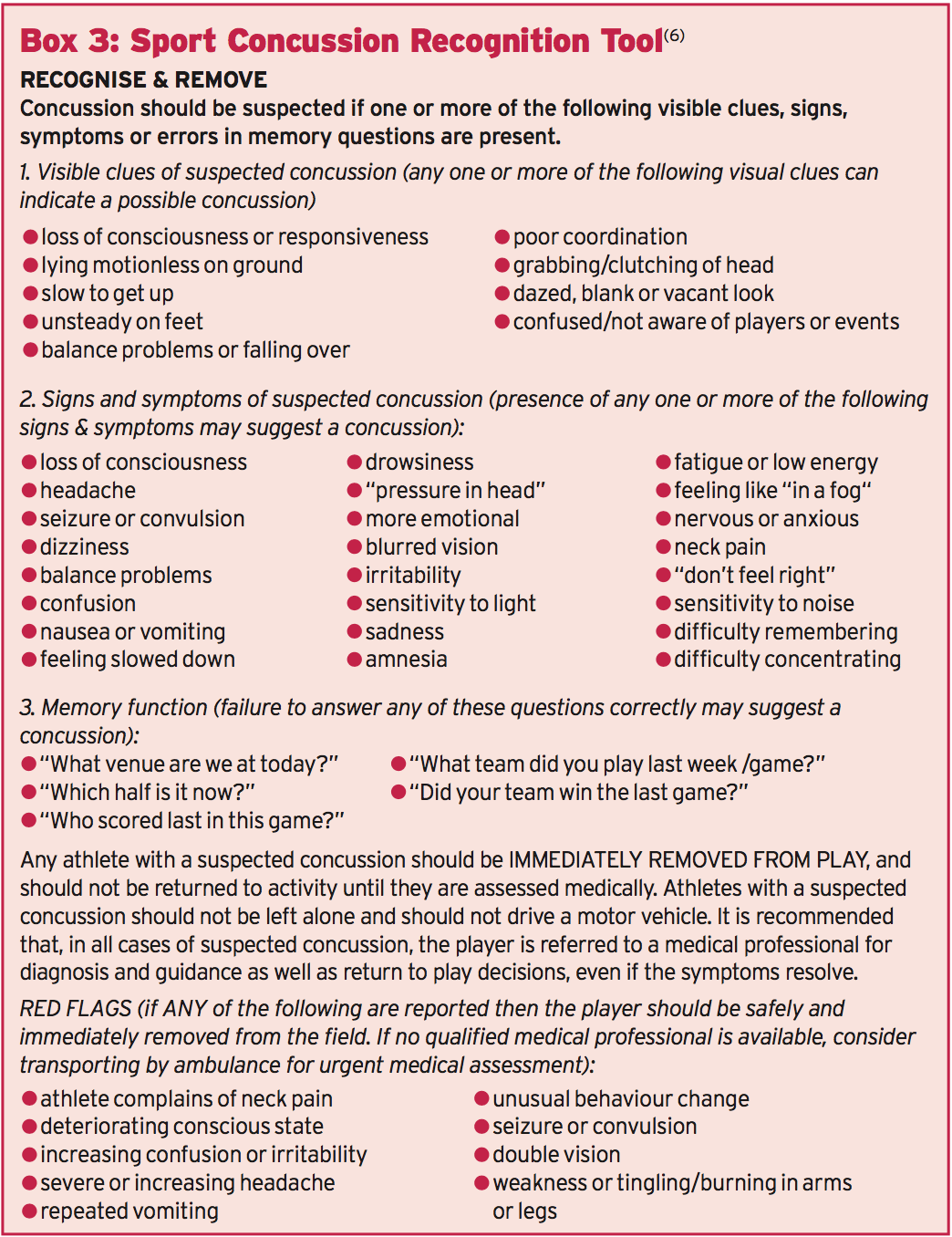
The primary recommendations were assembled by reviewing the evidence over a number of years and are summarized as follows:- Any athlete suspected of having a concussion should be stopped from playing and assessed by a qualified healthcare provider trained in the evaluation and management of concussion and ideally someone who is familiar with the athlete (for the reasons given above). The recognition and initial assessment of a concussion should be guided by a symptoms checklist, cognitive evaluation (which should include orientation, past and immediate memory, new learning and concentration), balance tests and further neurological and physical examination.
- Coaches/physicians/healthcare providers should take note that while balance disturbance is a specific indication of a concussion, it isn't very sensitive. In particular, performing equilibrium testing about the touchline may yield substantially different results than baseline evaluations simply because of differences in shoe/cleat-type or surface, use of ankle tape or braces, or the presence of other lower extremity injuries that might have also happened during the episode involving the head injury.
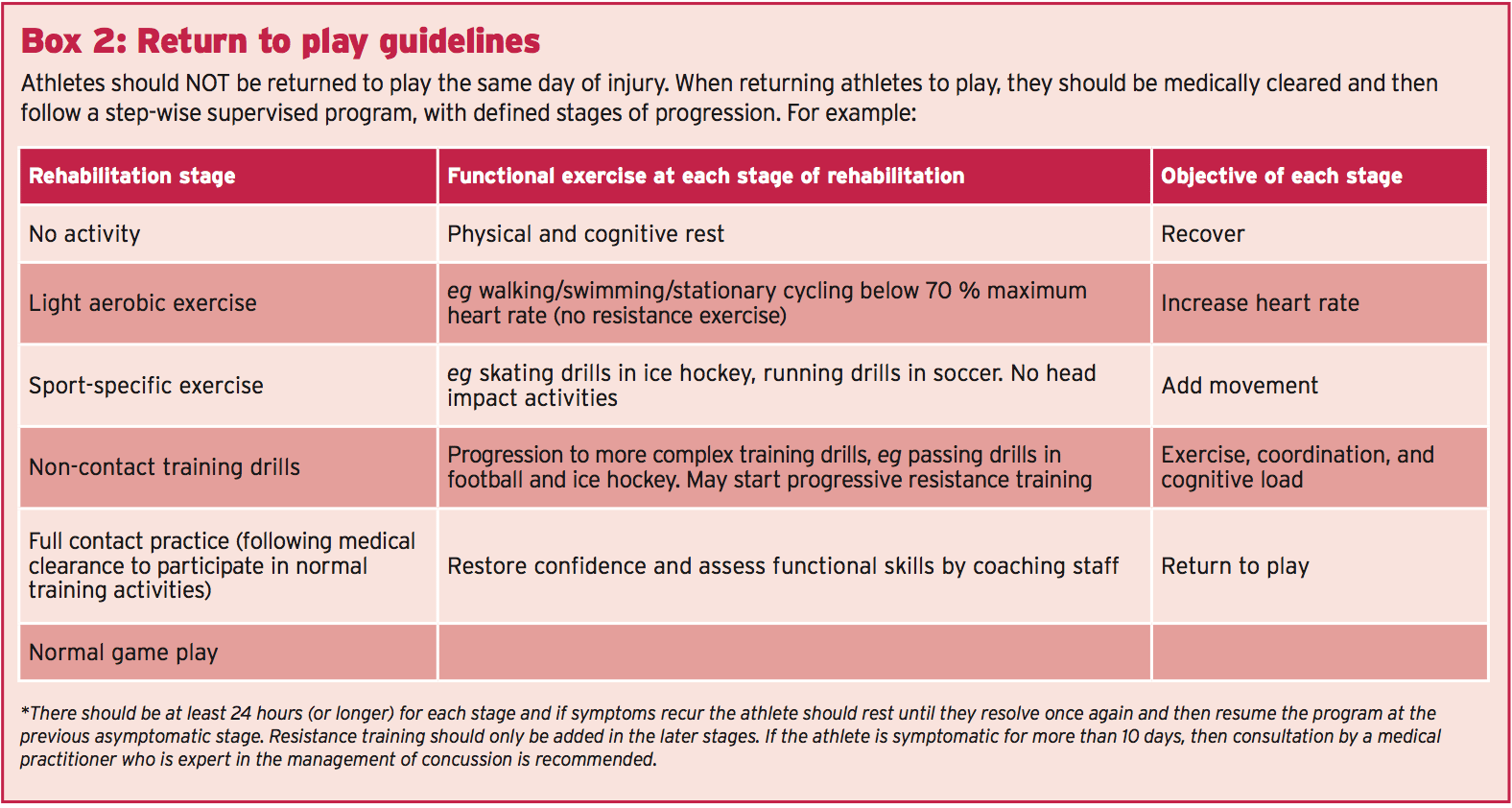
- Any athlete suspected or diagnosed with a concussion should be monitored for deteriorating physical or mental status. Importantly, there should be NO same day return to play for an athlete diagnosed with a concussion injury. Meanwhile, imaging should be reserved for athletes where intracerebral bleeding is suspected.
- Even though most concussions can be managed appropriately without the use of neuropsychological (NP) testing, those with athletes in their maintenance ought to bear in mind that NP evaluations are an objective measure of brain- behavior relationships and, as such, are somewhat more sensitive for subtle cognitive impairment than a straightforward clinical examination. However, NP testing should be used only as part of a extensive concussion management plan and should not be utilized in isolation. Also, the ideal timing, frequency and type of NP testing have not been completely ascertained.
- Computerized NP testing should be translated by health care professionals educated and comfortable with the type of test and also the individual test limitations. Paper and pencil NP evaluations are both valuable and are able to test different domain names and assess for different conditions, which may masquerade as or reevaluate evaluation of concussion.
- Concussion symptoms must be resolved before returning to perform with (RTP) and RTP after concussion should happen just with medical clearance from an experienced health-care supplier trained in the analysis and management of concussions -- see Box 2. An RTP progression entails a gradual, step-wise increase in bodily demands, sports-specific activities and the danger of contact. If any signs recur using action, the progression ought to be stopped and resumed in the previous symptom-free step. In the brief term, the principal concern with early RTP is diminished reaction time resulting in an increased risk of a repeat concussion or additional injury and prolongation of symptoms. In the long run, there's a growing concern that head impact exposure and recurrent concussions can contribute to long-term neurological complications and a number of studies have indicated an association between previous concussions and chronic cognitive impairment.
- Physicians should be prepared to offer counseling regarding potential long-term consequences of a concussion and continuing concussions. However, there are currently no evidence-based guidelines for disqualifying/retiring an athlete from a game after a concussion. More commonly, greater efforts are needed to educate involved parties, such as athletes, parents, coaches, officials and school administrators and health care providers to boost concussion recognition, prevention and management.
Recent Findings: On-Field & Same Day Assessment
Make no mistake, but the first assessment of concussion in the mature athlete is tough, given that the elusiveness of harm, the sensitivity and specificity of their sideline assessment tools along with the evolving nature of concussive injury. A very current (2013) review newspaper systematically examined the evidence related to on-field concussion assessment and considered questions related to same day return to play, what to do if no doctor is available onsite, as well as the benefit of distant notification of future concussive events(3). It concluded that the on-field test of sport-related concussion is often a challenge, especially given the elusiveness and variability of presentation, the strain to create a quick diagnosis (as an instance, in the middle of an important match in which the concussed athlete was making a significant contribution), the specificity and sensitivity (or rather lack of) of this on-field assessment tools, along with the dependence on symptom presentation.However, they cautioned that a range of assessments over a brief time period tend to be necessary and, since signs and symptoms may be postponed, erring on the side of caution (ie maintaining an athlete from participation whenever there's a distress for harm) is important. In addition, they concluded that although a standardized evaluation of concussion is beneficial in the evaluation of the athlete with suspected concussion, it should NOT take the place of the clinician's conclusion.
These findings have been very much in agreement with another 2013 review research on instruments currently utilized in the evaluation of sport-related concussion on the day of injury -- consequently 'same day' assessment tools(4). In this review, a total of 41 research on sports concussion were pooled and their findings analyzed. The authors concluded that several well- supported tests are acceptable to be used in the evaluation of acute concussion from the athletic athletic environment and that these evaluations can provide significant data on the symptoms and functional impairments that clinicians can integrate in their diagnostic formula. But they also cautioned that such tests should not solely be used to diagnose concussion.
SCAT3 Assessment Tool
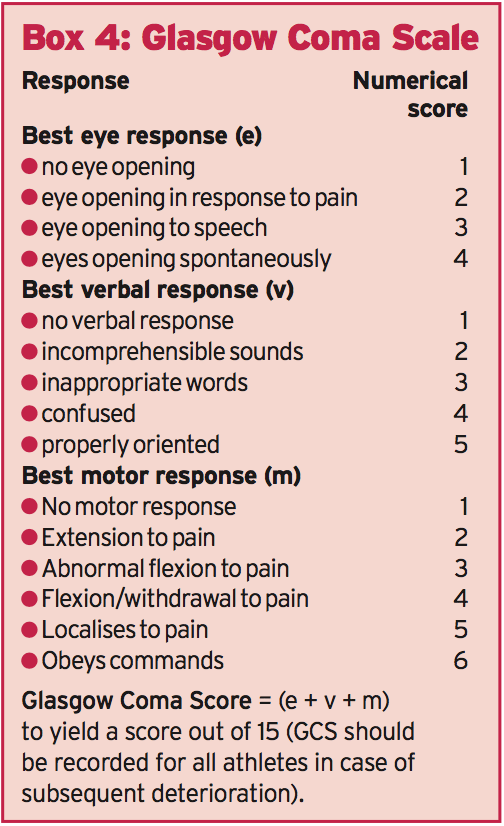
As mentioned above, the first evaluation of an injured athlete with suspected concussion remains predominant in determining subsequent action. There are a number of diagnostic tools available, but undoubtedly among the most admired is when there is no one with medical training available to tend to an injured athlete, it is recommended that the ‘Sport Concussion Recognition Tool’ be used instead (seeBox 3). The SCAT3 assessment tool can be downloaded here: http://bjsm. bmj.com/content/47/5/263.full.pdf. The SCAT3 is a standardized instrument for evaluating injured athletes for concussion, and is intended for use by medical professionals. SCAT3 supersedes the first SCAT and SCAT2 published in 2005 and 2009 respectively. Importantly, baseline testing together with the SCAT3 can be beneficial for translating post-injury test scores at a later date. The SCAT3 evaluation tool can be downloaded here: http://bjsm. bmj.com/content/47/5/263.full.pdf- a Glasgow Coma score of less than 15 (see Box 4)
References
1. Br J Sports Med. 2013 Jan;47(1):15-26. doi: 10.1136/bjsports-2012-091941
2. Am J Sports Med. 2012 Apr;40(4):747-55
3. Br J Sports Med. 2013 Apr;47(5):285-8
4. Br J Sports Med. 2013 Apr;47(5):272-84
5. Br J Sports Med 2013 47: 259
6. downloadable from: http://bjsm.bmj.com/content/47/5/267.full.pdf