Aaron was a final-year high school student and keen soccer referee. Complaining of mid-back pain, especially after he had refereed three or even four matches in a single day (which he often did). He experienced this same pain when he was sitting studying, but it was more prevalent after refereeing. He also advised me his quadriceps appeared to fatigue a whole lot more than the rest of his muscles after running around a whole lot. Scientific spine specialist, Dr. Alexander Jimenez takes a look at the case.
My first assessment of Aaron's spinal posture was that he was quite kyphotic (bent forwards) through his torso, with accompanying cervical spine flexion -- in sitting he simply flexed forward all the way through his spine.
He experienced his mid-back pain when he strove to extend or straighten himself up, so when he corrected his stance that the pain came on. The erector spinae muscles in their own mid-back proved very developed and seemed like thick ropes.
When I assessed Aaron's lumbo-pelvic stability, things got really interesting. I was seeking the way gluteus maximus and the psoas major muscles were performing, each of which help to control the impartial position of the pelvis under load. He'd shake all around the area.
To assess psoas major, I asked Aaron to sit and control the natural arch in his low back (neutral posture) as he lifted and hauled his bent leg in flexion past 90° (just an easy knee elevator). He was not able to maintain the leg even slightly off the floor without slipping together with his low back.
The runner needs to have quite an upright posture, letting the upper body to flex forward slightly, but not too much. The gluteus maximus gives a small amount of hip extensor muscle torque but much more importantly, it controls the upright position of the pelvis on the hip. Without this the body would just bend ahead. Isolated hip flexion is also necessary, in order that the lower back is kept in its neutral arch when the runner initiates the swing phase.
As soon as I examined Aaron's running posture, he had been very flexed at the hip, almost leaning over at about a 25° angle. He was managing to maintain his lower back neutral, however, the erector spinae muscles were working extremely hard in this place. He explained that he could feel this occurring and was hoping to liven up -- but he'd been doing this through his chest. This overuse of the erector spinae muscles are what had led to his growing mid-back pain.
The thoracic spine is affected substantially by the placement of the spinal column in all positions, from sitting postures to swinging a golf club, throwing a ball or running. The mid-back requires a stable platform in the lumbar spine where to execute its freedom functions. This is especially important in throwing sports but is also crucial in activities like swimming.
Thoracic spine motion in running should mainly involve rotation as this helps to counterbalance the hip flexion moment produced at the opposite hip. Over-activity at the thoracic extensors is counterproductive not only for performance but also for injury.
Treatment
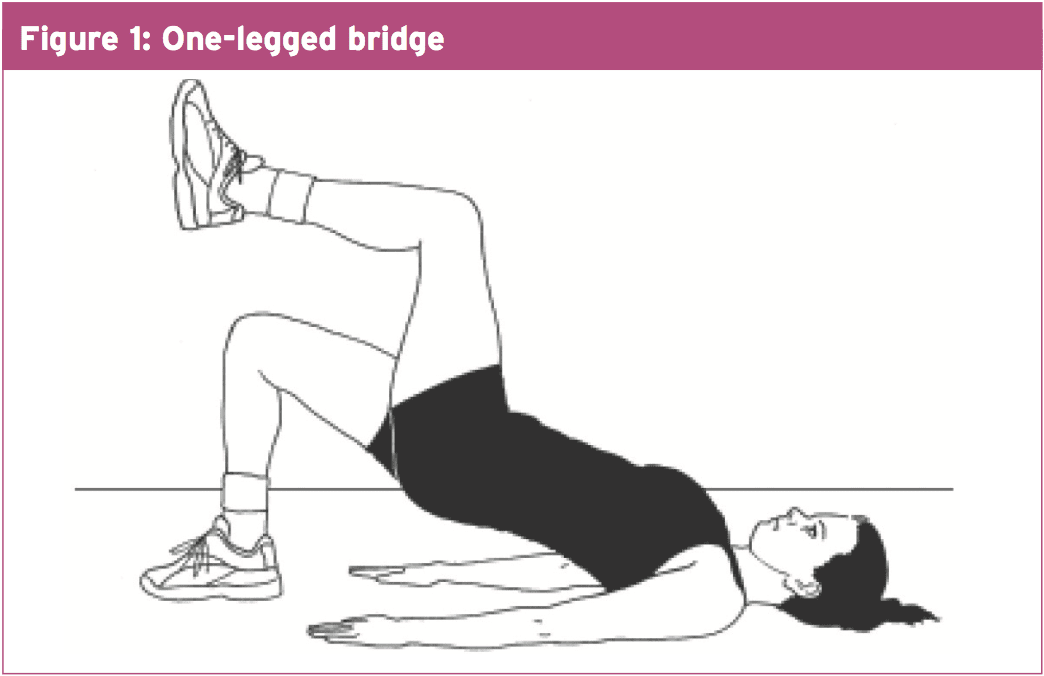
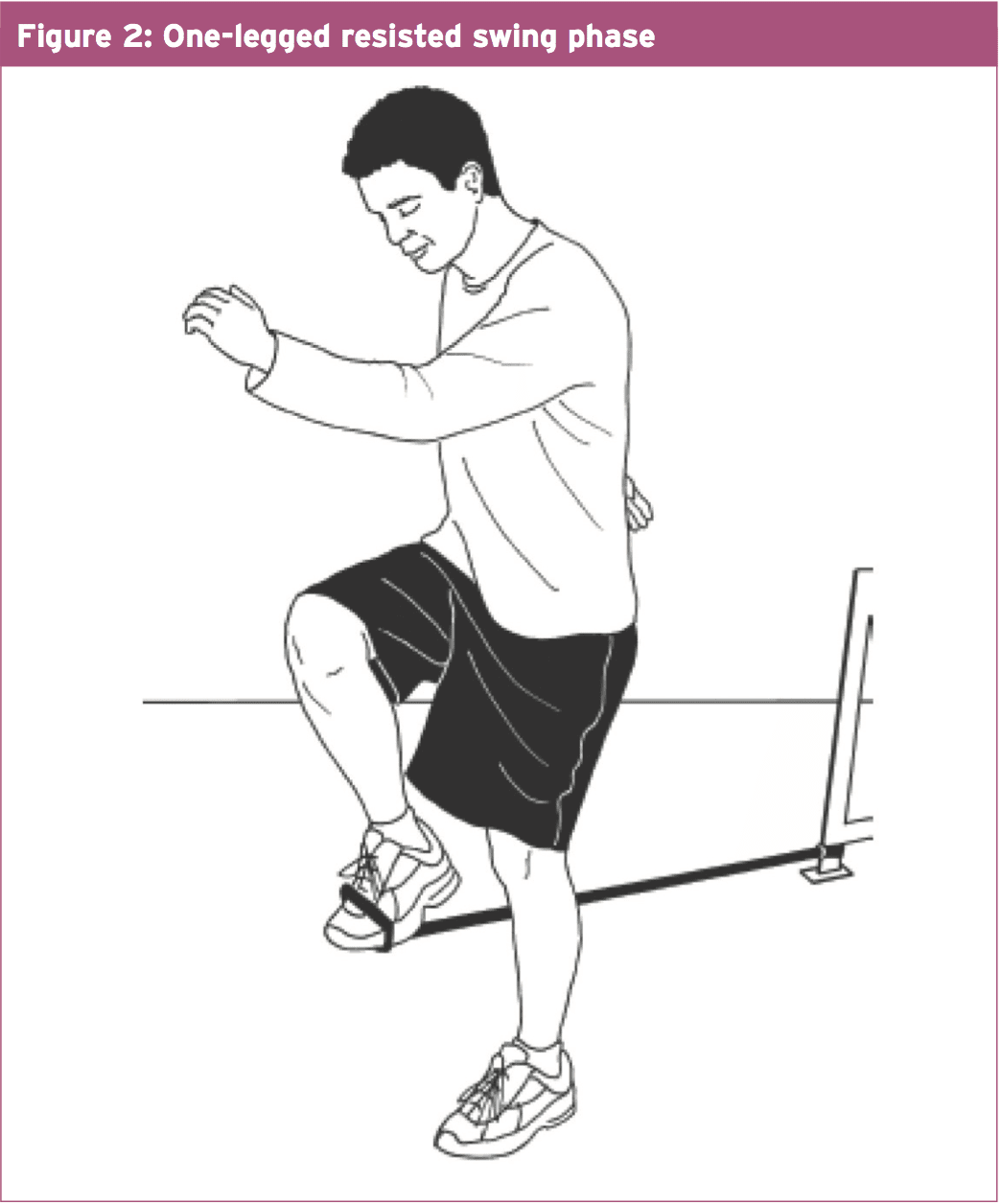
But we also needed to correct the pelvic muscle weaknesses that were acting on the thoracic spine and hip. I instructed Aaron to stand and operate tall throughout his hip place, with his gluteals, to take the load off the thoracic erector spinae. To be able to strengthen the gluteals so that they were up to the job, I made him to carry out the one legged bridges (see Figure 1). And in standing, I tied a piece of tubing around the ankle of one leg, and that he then utilized to mimic the running swing phase while he concentrated on keeping his pelvis fairly still on his stance leg (see Figure 2).Aaron's symptoms eased up quite quickly once he managed to fix his functioning posture and recruit his stabilizing muscles. I encouraged him to continue his exercises for the next six to eight months so that he would fully integrate the muscular recruitment routines into his running technique.