Frozen shoulder isn’t a common disorder in women and sportsmen, however when it does happen & it can be debilitating. Chiropractor, Dr. Alexander Jimenez looks at the most recent thinking on the best treatment options for restoring shoulder functionality.
Frozen shoulder, even more properly known as adhesive capsulitis (AC), has been a frequent source of shoulder pain and loss of movement in the over 40s. In ‘primary’ cases of AC, there is absolutely no reason for the onset stiffness or pain, whereas AC can happen following illness, trauma, surgery or an injury. AC is believed to affect around 3 percent of the population, with women at higher risk than men. In people below age 40, AC that is primary is likely to be secondary in character — for instance, also is infrequent, however. However, it could lead to significant disruption particularly given the timescale it requires to resolve, when it does occur.
Causes Of AC
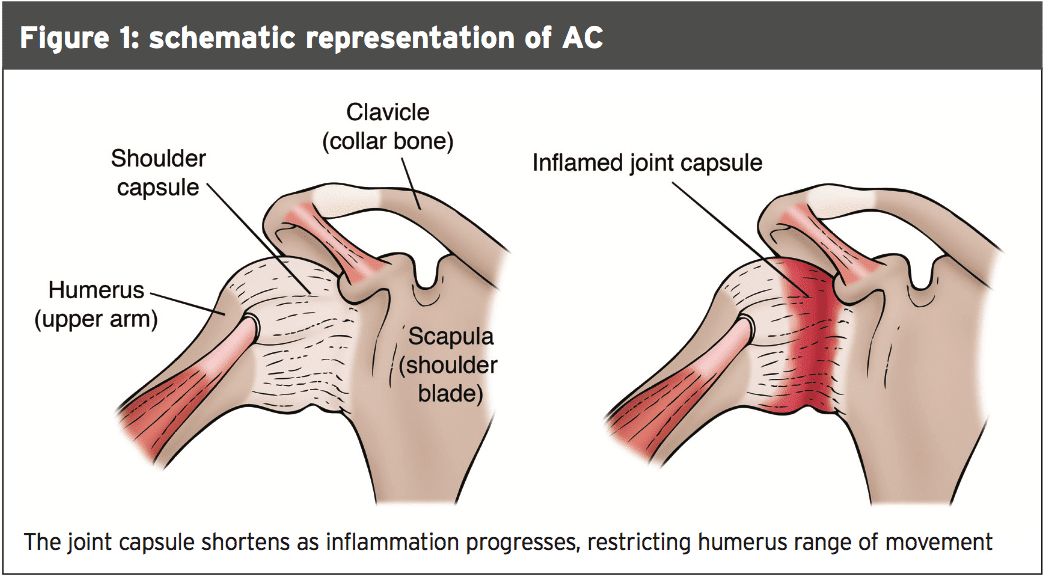
As its terminology implies, adhesive capsulitis describes a state where the joint capsule becomes inflamed and ‘sticky’ (see Figure 1), making the whole joint rigid and difficult/painful to move. AC’s etiology is known. We do understand, however, that because the capsule becomes inflamed, scar tissue forms, which leaves space for the humerus to move through its normal selection of motion and causes pain.Some studies have suggested that poor posture (especially rounded shoulders) can cause shortening of at least one of the ligaments of the shoulder, which might also lead to the condition. Athletes whose training results in and/or that are overdeveloped abbreviated pectoral and anterior musculature may therefore be at increased risk. Also, prolonged immobility (such as after a rotator cuff injury or shoulder fracture) is regarded as a risk factor for AC — a fantastic reason for athletes to rehab a shoulder injury as quickly as possible.
There appears to be a link between AC risk and some conditions. For example, studies indicate that a greater than normal amount of blood sugar (eg in diabetes) is a risk factor for AC(3). Insulin-dependent diabetics are at the maximum risk, and the problem is particularly severe in such cases. Likewise, high blood lipid levels are also associated with an increased risk of AC(4), while AC is also frequently observed in thyroid disorders, Parkinson’s disease, and a variety of cardiac and pulmonary disease. Despite each of these risk factors, however cases of AC remain idiopathic in nature, something which can be very frustrating for clinicians and sufferers .
Typical Characteristics
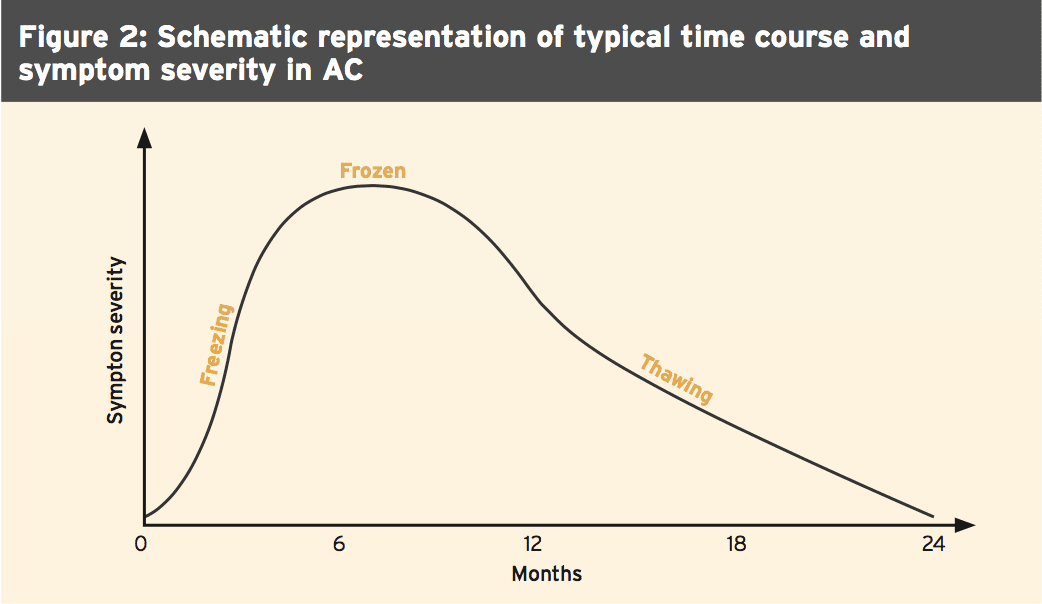
Concerning characteristics, AC typically displays a progression through three distinct phases: freezing, frozen and thawing (schematically represented in Figure 2). In the initial phase (freezing), patients typically present with noticeable pain that comes on over a span of a couple weeks with action. There isn’t a loss of range of movement. During this phase, many individuals respond by utilizing the shoulder which subsequently contributes to stiffness, developing a kind of vicious cycle.The thawing (resolution) stage typically lasts for 9-18 months, and is characterized by steadily diminishing levels of pain and stiffness. The advancements are just slow and it might thawing to happen. Indeed, several studies have clarified AC for a self- limiting condition which typically resolves in 12-36 months(5-7). But some studies have suggested that a substantial percentage of patients may remain symptomatic for up to ten years after the initial phase(8). Regardless, even an early resolution of AC still present a challenge for any sportsman or woman. If their sport does not rely heavily on shoulder joint usage and variety of motion, there are few sports in which shoulder motion is absent, meaning that sport exercise may cause or increase pain and distress.
Diagnosis
AC can be difficult to differentiate from ordinary shoulder ailments and to diagnose in its early stages. Because of this, X-rays of the shoulder can be very useful to exclude constipation of the other or joint pathologies. Besides the clinical features described above (specifically the nearly total loss of external rotation in passive movement), the typical routine of AC beginning is also useful in making a diagnosis. In situations where uncertainty remains, MRI scans demonstrating a thickening in the joint capsule and the ligaments that are affected, in addition to indications of synovitis provide further evidence for AC(9,10).The widely held opinion among clinicians is that a diagnosis of AC can typically be verified in the practice and doesn’t normally require extensive investigation(11). However, recent research published this season suggests caution, especially in early- stage AC(12). Scientists studied the validity of widely used clinical identifiers of early- phase primary/idiopathic adhesive capsulitis. These identifiers were range of motion pain and loss during eight moves. The results demonstrated (rather surprisingly) that none of the clinical identifiers for early-stage AC formerly suggested by expert consensus were verified as well as the researchers concluded: “Clinicians should bear in mind that commonly used clinical identifiers may not be related for this point.”
Treatment Options
AC’s treatment stays controversial, based on the extent of the pain and stiffness, and the stage of the disorder. Conservative treatment options include the use of non-steroidal anti- inflammatory medication (NSAIDs) and physiotherapy. NSAIDs can help provide some symptomatic relief but there’s little evidence they affect the disease development. Physiotherapy by contrast may be more successful. Lots of studies examining the use of physiotherapy in the early and mid-stage of AC have shown an improvement in pain scores, operation and range of motion(13-19). Despite these more recent study is much equivocal, as we will see.When treatment options are ineffective, surgery or injections remain options. The most common approaches are manipulation under anaesthesia capsular release and capsular distension medications. In a poll of UK caregivers, just 3 percent recommended surgical procedures for the initial painful freezing stage but for its second and third phases, this increased to almost 50 percent of the surveyed(20).
There remains controversy about efficacy. As an example, 1 study on 110 instances of AC found that patients receiving physiotherapy alone had better clinical results than patients undergoing MUA(14). By contrast, however, a study of 77 patients with AC demonstrated that ‘supervised neglect’ supplied better results at two years in comparison with a intensive physiotherapy regime, suggesting that physiotherapy might not alter disease progression, especially if the regime is too aggressive(21).
Latest Thinking
The character of AC perhaps explains why there’s no clear consensus on the optimum treatment protocol for AC. It so happens that 2014 watched the publication of a Cochrane Database systematic review to the efficacy of manual therapy and exercise — specifically, how it than the glucocorticoid shots(22).The research groups accumulated statistics from 32 randomized controlled trials (RCTs) and quasi-randomized trials (a total of 1836 patients), which compared with any manual therapy or exercise intervention versus placebo, no intervention, another sort of manual therapy or exercise or any other intervention. Interventions included mobilization, manipulation and exercise, delivered independently or in conjunction. The outcomes of interest were active shoulder abduction, overall pain, shoulder function, global evaluation of treatment success pain relief of 30% or greater, quality of life and also the amount of participants.
The main findings were as follows:
- The outcome differences involving interventions Which Were clinically important were discovered up to seven weeks, after
- A combination of exercise and therapy for six months resulted in improvement at seven months but a similar number of adverse events compared with glucocorticoid injection;
- The mean improvement in pain with shot was 58 points on a 100-point scale, and 32 points with exercise and manual therapy;
- The improvement in function with glucocorticoid injection was 39 points onto a scale, and 14 points with exercise and manual therapy;
- Forty-six per cent of participants reported treatment success with manual therapy and exercise in comparison to 77 percent (40/52) of participants receiving glucocorticoid injection;
- Including a combination of manual therapy, exercise and electrotherapy for four months to injection did not confer benefits over glucocorticoid injection at every time point.
- 1 trial of 119 participants discovered a combination of manual therapy, exercise, electro therapy and or alnon-steroidalanti- inflammatory drug (NSAID) for 2 weeks didn’t confer clinically significant benefits over oral NSAID independently in terms of function and patient-reported treatment achievement at fourteen days.
Stretching Success
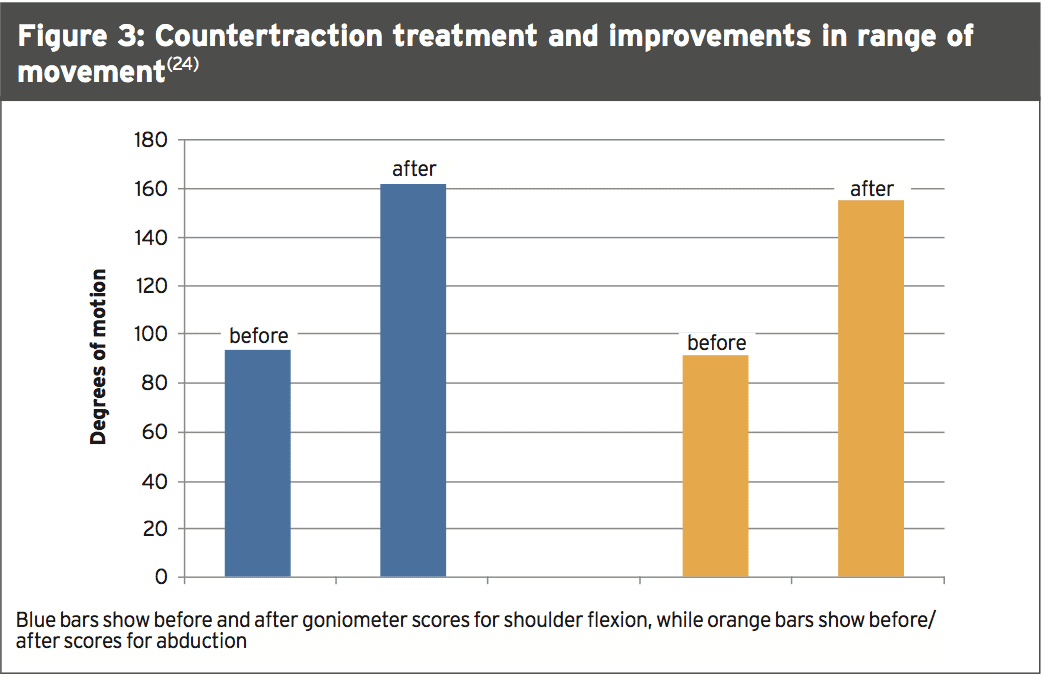
One study that wasn’t included in the above mentioned review (since it is too recent) is much more promising. This analysis looked at the efficacy of sustained stretching of the inferior capsule in the managing of a frozen shoulder — specifically the potency of a shoulder counter grip apparatus on range of motion, pain, and function in patients with a frozen shoulder(24). A total of 100 participants were randomly assigned to a control group or an experimental group, with each group. While the experimental group obtained traction and physiotherapy the control group received. The treatment time was 20 minutes a day for five days per week for two weeks.When countertraction was given along with physiotherapy, the scores for shoulder flexion improved from 94.1° at baseline to 161.9° after intervention (see Figure 3). Abduction selection of movement rose from 90.4° into 154.8° after intervention, while pain decreased from a score of 8.00 to 3.48. Overall, 60 percent of the participants were enhanced to the fourth stage of satisfactory joint function (based on the Oxford Shoulder Score) at the experimental group compared to only 18% in the management group. Whether these improvements were sustained over a longer period of time was not investigated, but the first results are encouraging.
Ultrasound/PRF Benefits?
Recent studies have demonstrated that pulsed radiofrequency (PRF) lesioning of the suprascapular nerve (SSN) using a fluor-oscopy- or computed tomography-guided technique can relieve shoulder pain.Until recently, there were no studies into PRF lesioning using practices. However, a newly published 2014 study has compared the effect of physical treatment alone with physical treatment and PRF lesioning of their SSN using guided ultra- noise(25). From the study, 60 patients have been randomised to the following two classes:
- An intervention group comprising patients who received a treatment of weeks of therapy;
- A control group comprising patients who received 12 weeks of therapy alone.
The results demonstrated that the intervention group had a notably shorter time to onset of significant pain relief (6.1 vs. 28.1 times) and a much greater decrease of VAS score at week 1 (40% .4.7 percent) than the control group. A comparison of both groups indicated progress in the intervention group at all times in shoulder pain and VAS, passive array of motion and in handicap index scores — an effect that lasted for at least 12 weeks.
Surgical Options
Finally, in cases what exactly does the current study say about effective choices? A 2014 study has compared the outcomes of three different forms of operation in patients experiencing persistent primary AC(26). These were:- A combination of arthroscopic capsular release and subacromial decompression (21 topics);
- Subacromial decompression combined with mobilisation under anaesthesia (18 topics);
- Selective capsular release. (15 subjects).
Each of three surgical treatments enhanced the selection of motion in every direction, with equal improvements in abduction and flexion. All treatments also improved external spinning, but selective arthroscopic capsular release trended towards a greater gain than the other two treatments (though this result was not big enough to be considered statistically significant). The authors reasoned that the surgical techniques improved ranges of motion in the glenohumeral joint but that overall, arthroscopic capsular release (independently or with subacromial decompression) demonstrated the best results postoperatively and should hence be advocated as the first choice treatment in persistent AC.
Summary & Conclusions
AAC is fairly infrequent and uncommon in younger sportsmen and women . Trainers who suffer with type I diabetes are at increased risk, as are athletes near the time of the menopause it may affect anyone at any time.AC presents challenges for the clinician. Not only does this take a considerable time to resolve even in the best case situation, there remains much uncertainty about treatment approaches that are effective. But even if there is little evidence that it significantly simplifies the length of the problem, any intervention that can help reduce pain is desired, possibly making all the difference between an athlete not being able to tackle any training whatsoever and having the capability to execute some restricted training.
The evidence healing speeds is feeble although conservative approaches such as therapy remain the primary port of call. But some recent evidence suggests that the accession of countertraction or ultrasound-guided PRF lesioning into physiotherapy maybe more effective than physiotherapy.
These more specialised techniques may be harder to justify and are of course time consuming and expensive to do given the evidence from systematic reviews suggesting that shots alone may be an effective treatment. In persistent and severe cases of AC, surgery may be the best option. In this situation, while the data is limited
Evidence suggests that arthroscopic capsular release is likely to be more effective than manipulation.
References
1. J Bone Joint Surg Br. 1995;77(5 ):677
2. J Bone Joint Surg Am . 1989 ;1(10 ):1511
3. South Med J. 2008 Jun;101(6):591-5
4. Rheumatol Int. 2014 Jan;34(1):67-74
5. Br Med J 2005;331(7530): 1453-6
6. Curr Rev Musculoskelet Med 2008; 1(3): 180-9
7. Br J Gen Pract 2007; 57: 662-7
8. Scand J Rheum 1975; 4(4): 193-6
9. J Bone Joint Surg Br 1995; 77(5): 677
10. J Bone Joint Surg Am 1989 ;71(10): 1511
11. Open Orthopaedics J, 2013, 7, (Suppl 3: M10) 352-355
12. Phys Ther. 2014 Jul;94(7):968-76
13. J Bone Joint Surg Am 2000; 82(10): 1398.
14. Arch Orthop Traum Surg 1995; 114(2) : 87-91.
15. Ann Rheum Dis 1984; 43(3): 353-60.
16. Arthritis Rheum 2003; 48(3): 829-38.
17. Physiotherapy 2002; 88(8): 450-7.
18. Br Med J 1998; 317(7168): 1292-6.
19. Cochrane Database Syst Rev 2003;(2): CD004258
20. Shoulder Elbow 2010; 2(4): 294-300
21. J Shoulder Elbow Surg 2004; 13(5): 499-502
22. Cochrane Database Syst Rev. 2014 Aug 26;8:CD011275
23. Health Technol Assess. 2012;16(11):1-264
24. Clin Orthop Relat Res. 2014 Jul;472(7):2262-8.
25. Anesth Analg. 2014 Sep;119(3):686-92
26. Acta Orthop Belg. 2014 Jun;80(2):172-7.