Patellar tendinopathy is a common injury in jumping sports, especially when loads are high or suddenly increase. With this in mind, chiropractor, Dr. Alexander Jimenez guides the practitioner through the problem- solving steps required to formulate a rehabilitation program for restoring the load absorption capacity of a grumbling patella tendon…
Patellar tendinopathy (PT) affects an athlete’s performance ability to jump, land, change direction and run. It can lead to a reduction in tolerance of training and competition load, and eventually a decline in performance, resulting in missed training and competition.
Managing PT during the competition phase of a season can be frustrating. High loads are continually placed on the tendon, and the condition can be frequently slow to respond to treatment interventions. It is important to be realistic and not expect a full recovery of the tendon during this in-season phase.
Managing PT during the competition phase of a season can be frustrating. High loads are continually placed on the tendon, and the condition can be frequently slow to respond to treatment interventions. It is important to be realistic and not expect a full recovery of the tendon during this in-season phase.
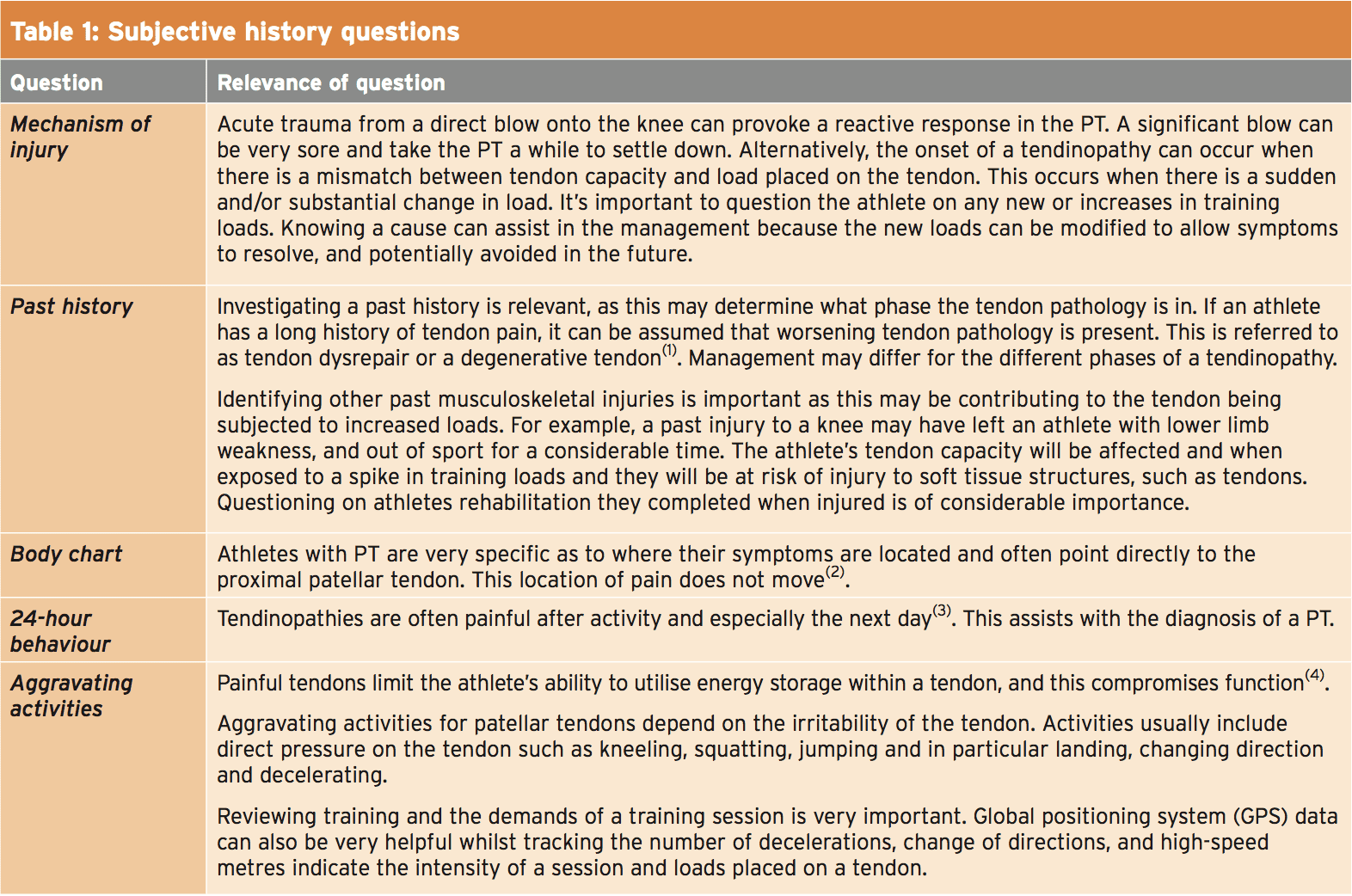
Subjective History
When diagnosing athletes with suspected PT, a thorough subjective history must be taken before a clinical examination takes place. This helps with not only an accurate diagnosis, but also gives an understanding of the potential causes and the severity of the tendinopathy. Critical questions to ask are shown in Table 1 below.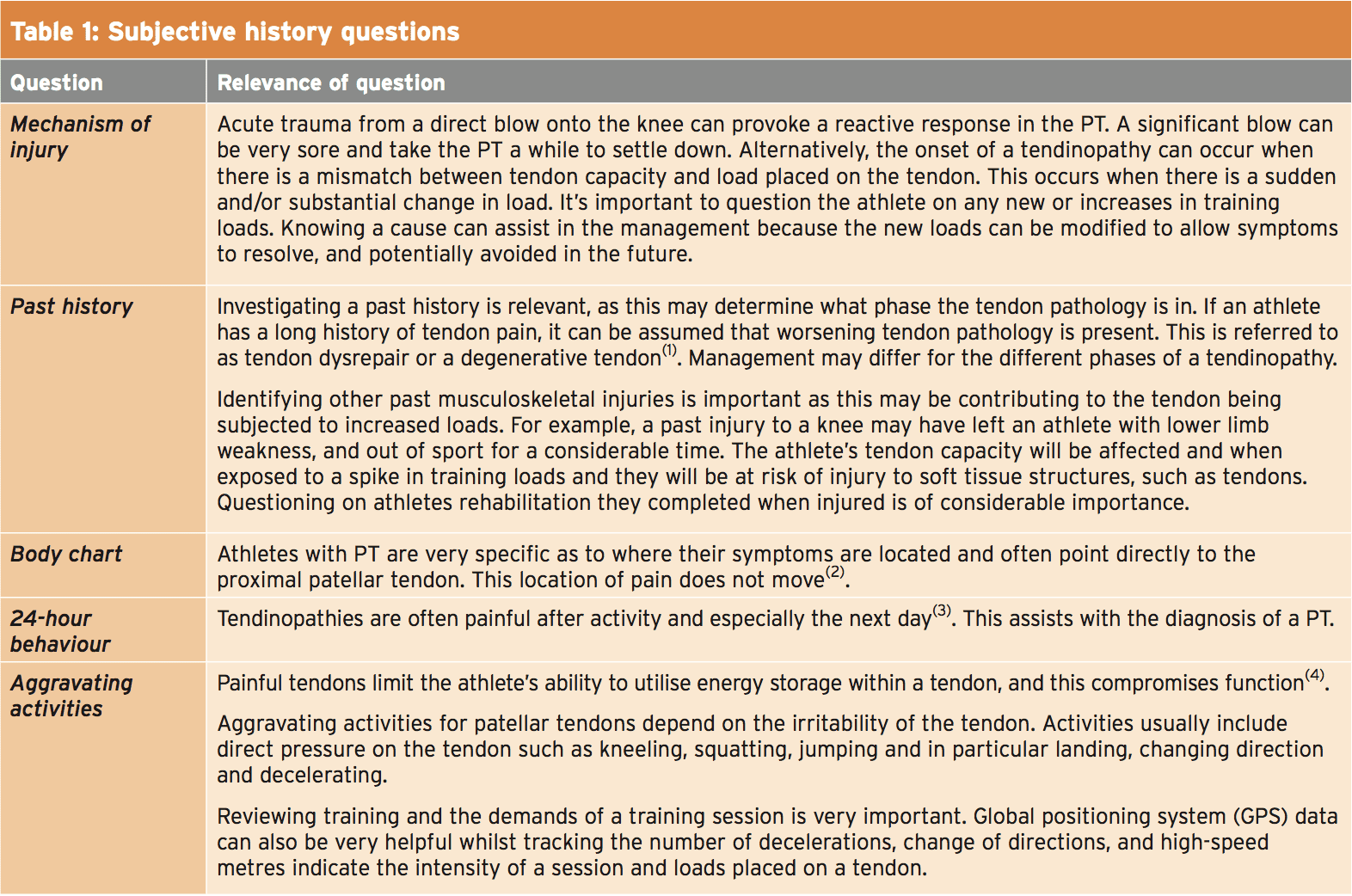
Once a thorough subjective history has been completed, a clinician should have a primary diagnosis, understand how irritable the tendon is, what phase the tendon is in and reasons as to why the PT is present. This will help guide a physical assessment.
Physical Assessment
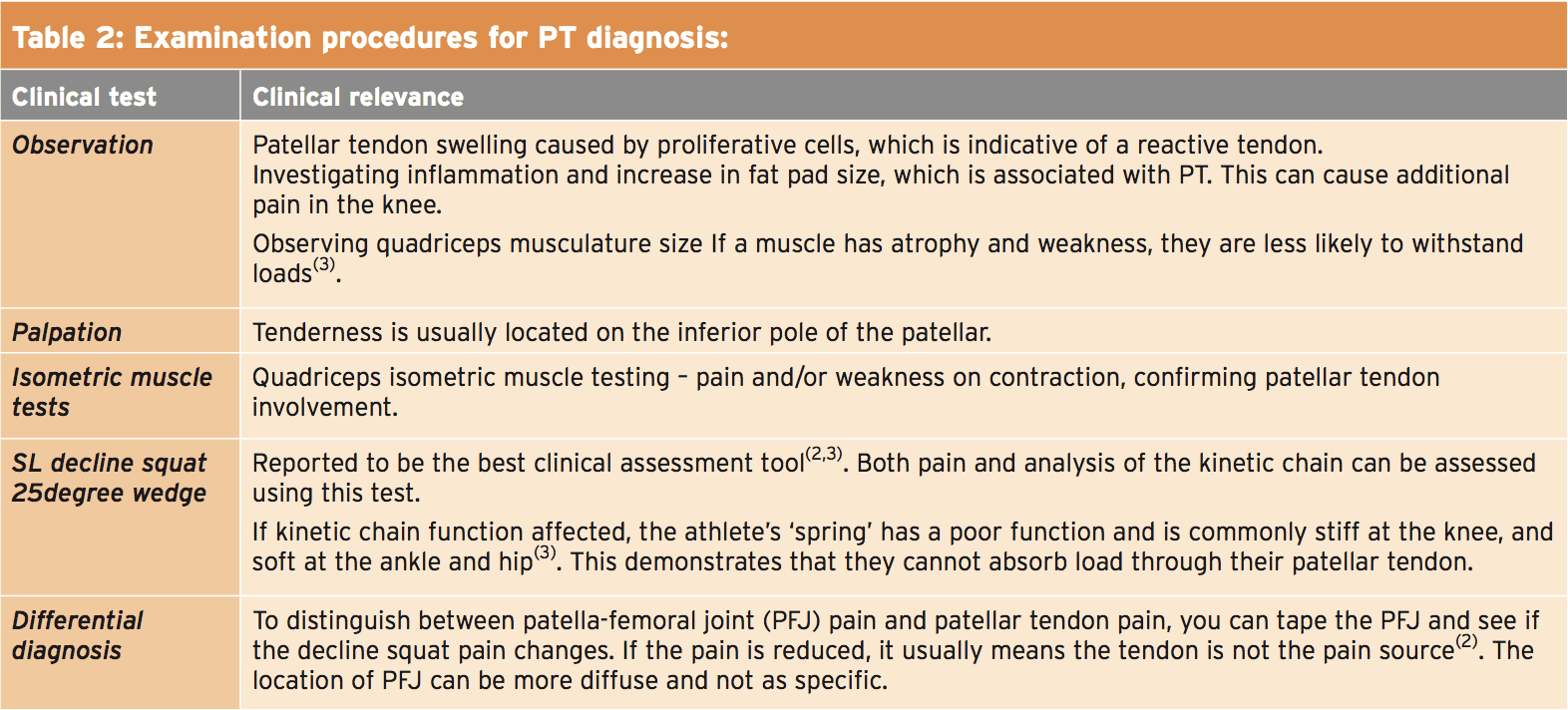
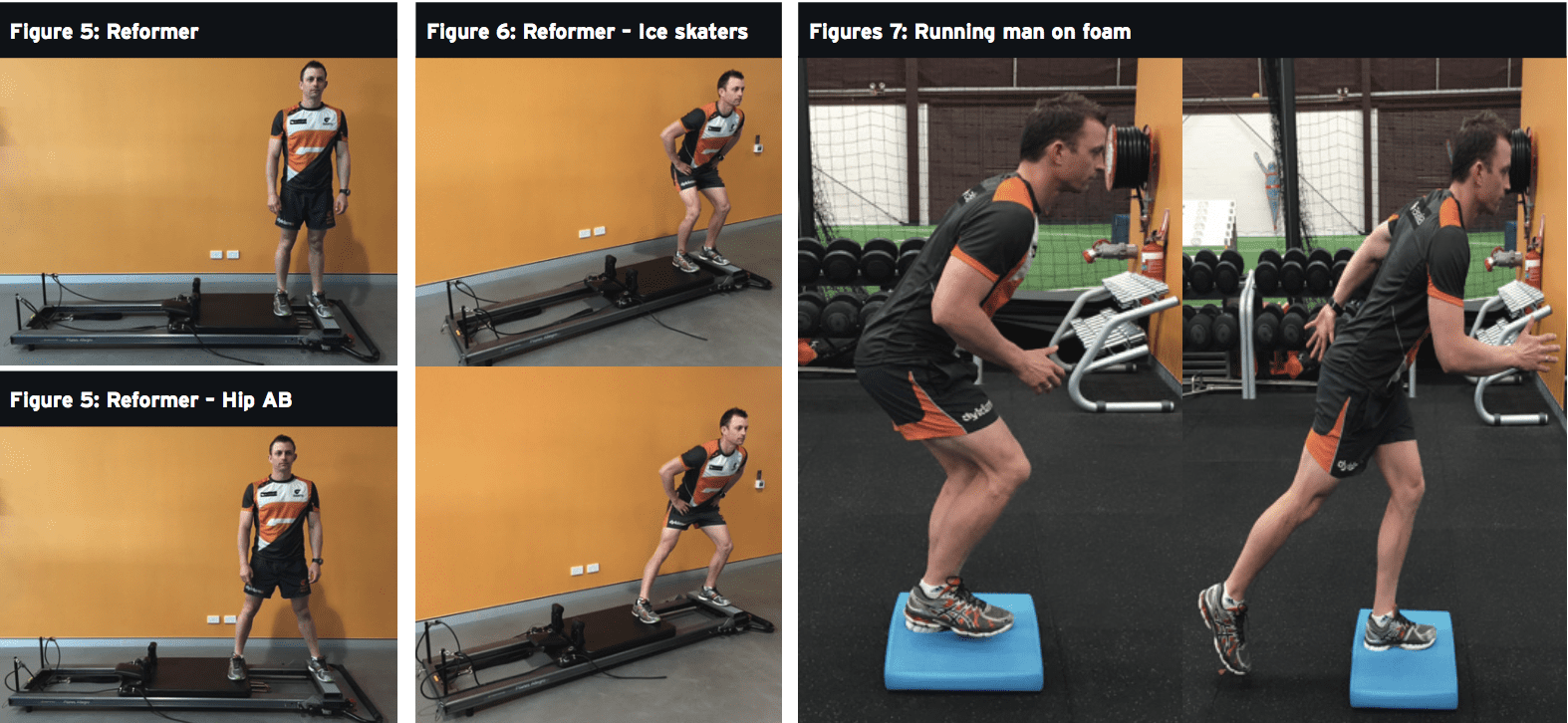
A therapist assessing the athlete should already have a strong primary diagnosis based on the subjective history. The priority of the physical examination is to confirm the primary hypothesis, exclude other potential hypothesis and to determine the irritability of the tendon, which will ascertain the functionality of the athlete. Table 2 outlines the best current thinking on examination procedures.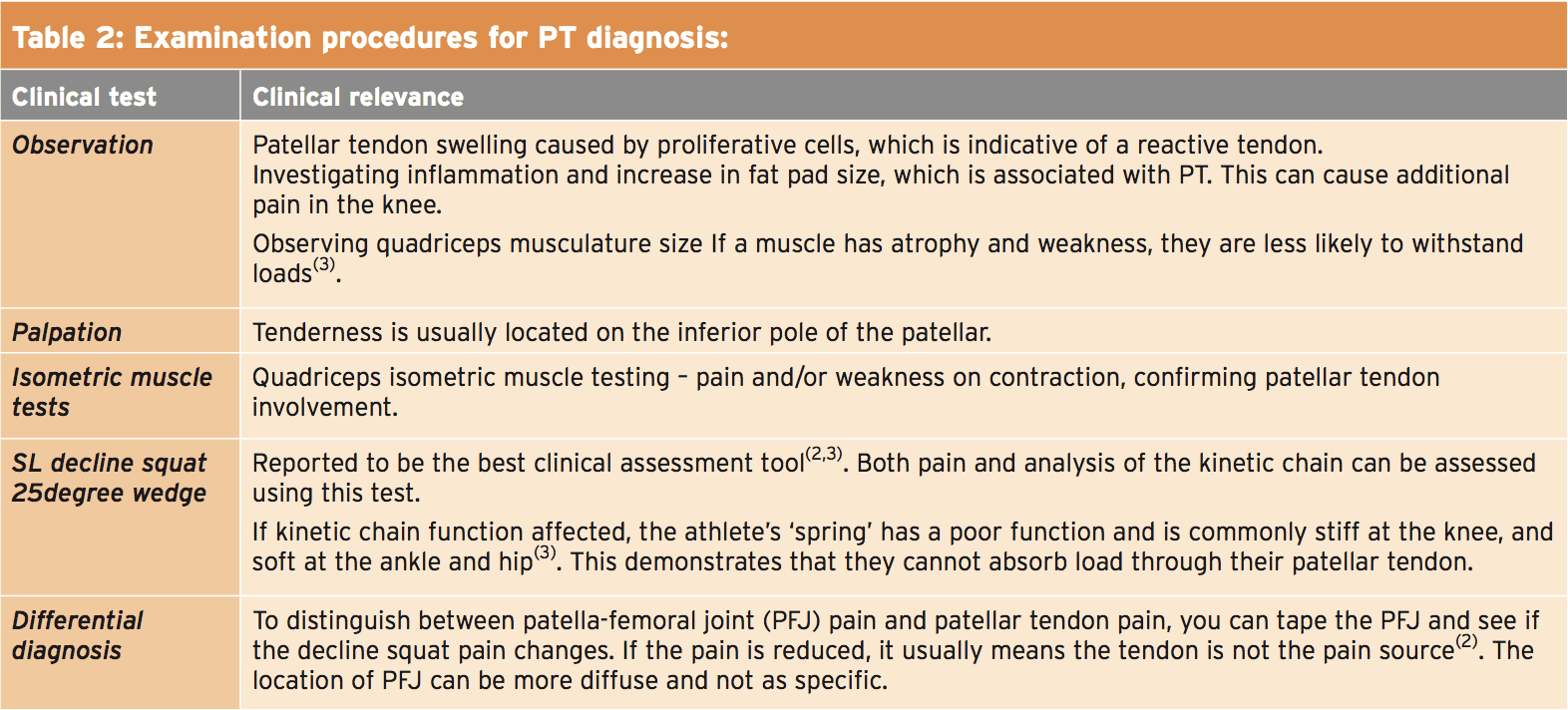
Further Investigations
Imaging using MRI and ultrasound can identify the presence of pathology in the tendon. Ultrasound (US) tissue characterisation shows the amount of disorganisation within a tendon and can help characterise the extent of structural pathology(2). However the presence of a PT on imaging does not always mean it is the source of pain, and clinical confirmation is necessary(3). MRI and US imaging are the two modalities used in my practice; an acute strain to a tendon should be excluded and the US can help confirm worsening tendon pathology. Management of a tendon differs according to what phase a tendinopathy is in.Acute Management
Whilst the pathology of the tendon may never completely resolve, conservative management of a PT is favourable. The initial treatments goals are aimed at pain management, education and planning.Pain Management
- Relative rest is the first priority to unload the reactive tendon. However, there should not be complete cessation of activities because this will decrease the overall capacity of the tendon(5). The overall capacity refers to the amount of load a tendon can withstand and by resting completely, a de-training effect will occur.
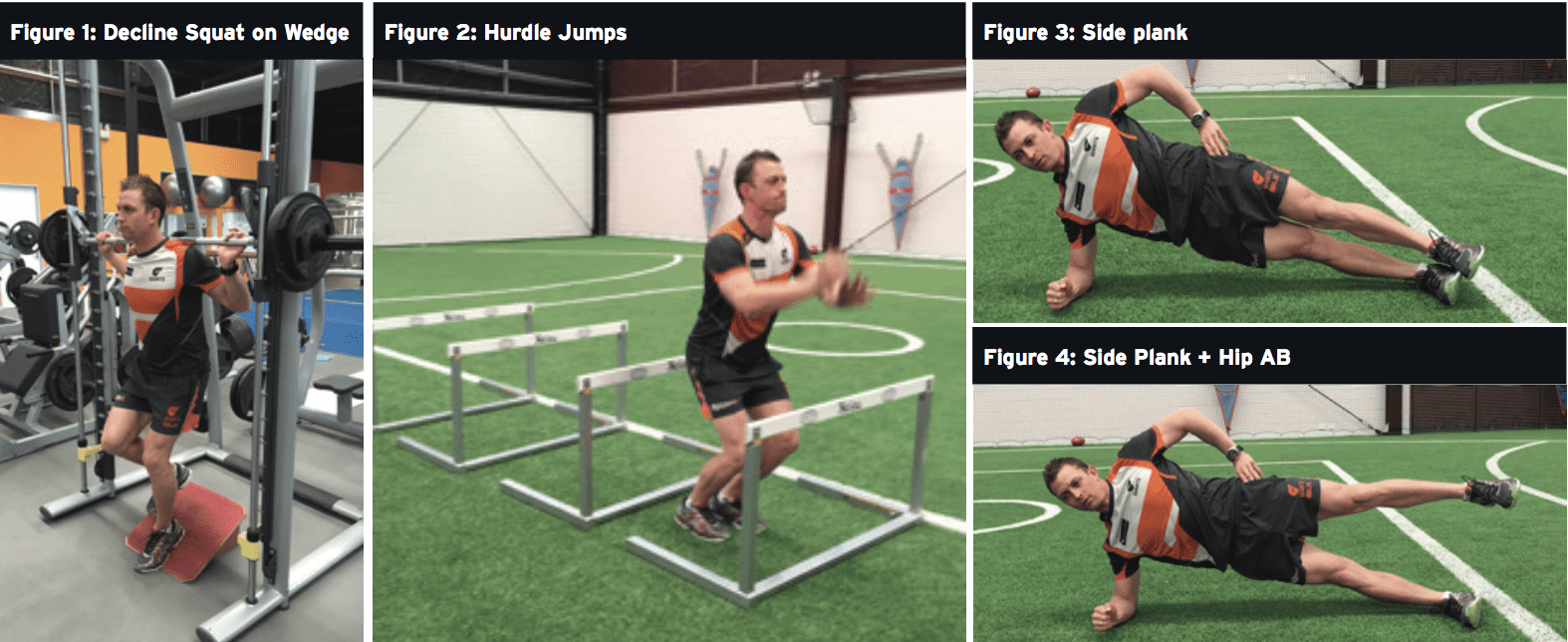
- Isometric single leg knee extensions and/or single leg decline squats should be prescribed for pain reduction: 5 repetitions x 10-60 second holds performed four- times per day. In reactive tendons, isometric contractions with moderate- heavy loads has been reported to be effective in reducing pain for hours(2,3,6).
- It is important that these exercises do not further aggravate the tendon, so prescribe the correct time and appropriate resistance as tolerated by the athlete. In reactive tendons, avoiding any pain is essential to avoid any further aggravation. In tendons in the dysrepair or degenerative phases, exercising into pain of a less than 3-4 out of 10 on the visual analogue scale (VAS) is appropriate. Morning pain, single leg decline squat on a wedge and 3x vertical hops should be used to monitor pain and response to load on a daily basis every morning.
- Icing after activity for 20 minutes for an analgesic effect may help reactive tissue around the patellar tendon (such as a fat pad) settle down.
Education
- Athletes must be educated on the importance of resting the tendon and not pushing past 3/10 pain on VAS whilst in the reactive phase of a tendinopathy, because symptoms will worsen. The athlete should be educated about how tendons may feel okay during training but may sore the next day. Progressions in loads should be calculated, not to be aggressive and risk a flare up of symptoms – eg planning and measuring the amount of decelerations in a running program.
- Avoid stretching the tendon, through doing quadriceps stretches. Compressive loads can further aggravate a tendon(1). Soft tissue massage and/or acupuncture through the quadriceps and hip flexors can be utilised alternatively to maintain knee and hip ROM.
- Interdisciplinary management: management of tendon pain should be seen as an issue for an interdisciplinary team to solve. As such, it is helpful to discuss the situation with a physician and dietician as they can administer some ibuprofen, high dose of fish oil and green tea. This may help decrease tendon pain(7).
Ongoing Management
- Managing tendinopathies in-season is about trying to explore the correct balance of unloading the tendon without causing a detraining effect on the tendon. Daily pain monitoring as discussed provides useful information about tendon responses to load. Use of the VISA-P (Victorian Institute of Sport questionnaire) may also be useful.
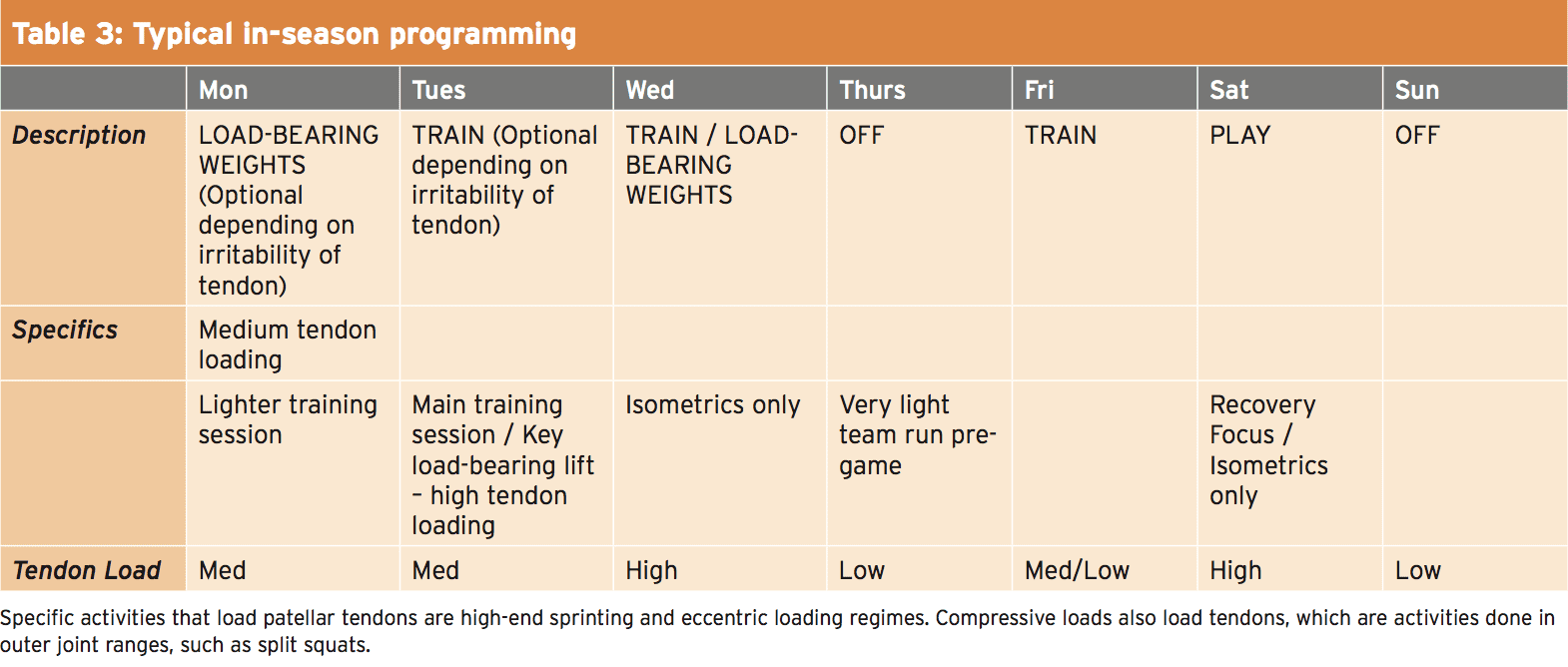
Programming
Reactive tendon response is the main cause of in-season pain, so the key intervention should be aimed at reducing loads. Load modification can be programmed specifically to relieve tendon pain:- Programming should periodise an athlete’s week into high, low and medium-load days, to respect the tissue adaptation from demanding sessions where increased elastic loading is present.
- High-load days include increased amounts of stretch shortening cycle (SSC), such as field sessions including training where there may be a lot of running, jumping and mechanical load.
- Medium-load days include specific tendon strength program and/or a less demanding field/running session.
- Low days-load include isometric holds only.
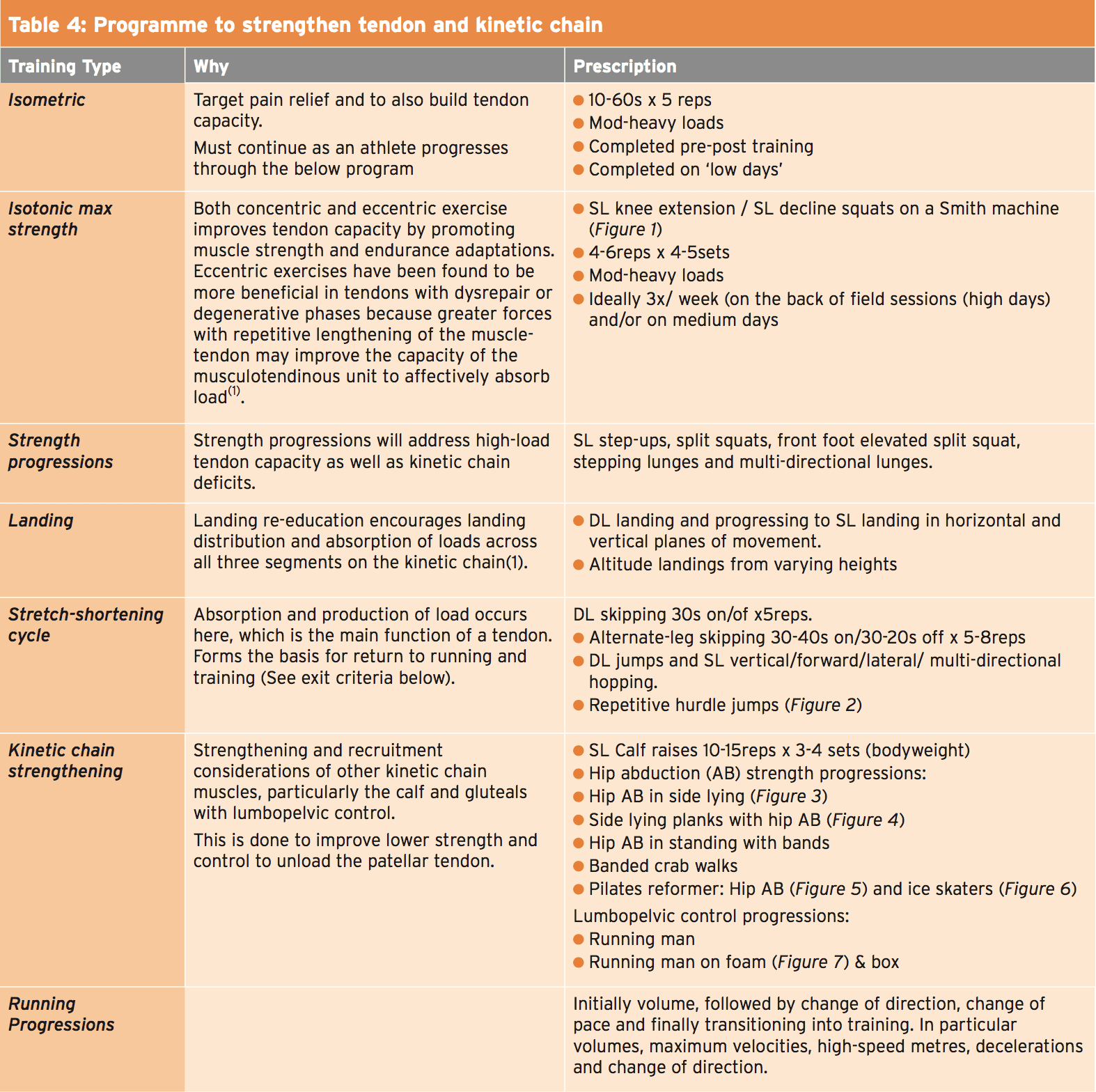
Strengthening The Tendon & Kinetic Chain
During the competition phase of the season it is hard for symptomatic PT to become completely symptom free and to achieve strength gains. The following program in Table 4 takes time and depends on the irritability of the tendon. A less than 3/10 pain level should be the threshold and exercises should not progressed if this level of pain or higher is present.Exit Criteria
Before being able to jog, the athlete must be pain-free walking, on stairs and be able to perform the following programme AND have a pain score of less than 4 out of 10 pain post session/next morning when performing a SL decline squat:- Decline SL squats on wedge to parallel (x 4 reps each side) with a pain score of less than 3/10;
- SL calf raises – x25 reps each side;
- DL skips (30 secs on/off x 5reps); Alternate skips (40 secs on/20 secs off x 10reps);
- DL hopping/landing progressing to SL hopping/landing sequences (including forward, lateral and multi-directional hopping);
- Running progressions on an Alter-G treadmill (if available) progressing from an entry level of 70-100% weight bearing;
- The introduction of running must be calculated, progressive and programmed to include high, low and medium days as discussed;
- Tendon daily monitoring must be completed and be a guide for progressing the athlete through the above exit criteria, running progressions and training.
Outcome Measures
The best outcome measure is the athlete’s pain provocation (VAS) during competition – more specifically VAS whilst performing specific activities such as decline squatting, hopping, jumping, running, changing direction and decelerating. Outcome measures specific to strength gains are increases in thigh circumference measured by DEXA scan or tape measure and by an increase in weight lifted, reps and sets. Quantifying lower limb power is achieved by measuring a single-leg hop for distance, vertical jump (single/double leg) and a cross-over hop test. Running sessions should be also be measured, quantifying volume, high speed metres, number of Disc herniation decelerations, and change of directions.Summary
PTs during the competition phase of a season can be challenging to manage. It is important that a thorough history is taken to understand why the athlete has a mismatch between tendon capacity and load. Once this has been established, relative rest (not complete rest) and programming of high, low, medium training days must be done to unload the tendon. Acute management aiming to decrease pain is of utmost importance. A focus on isometric exercises for pain relief will help achieve this. If symptoms are respected and monitored daily, this approach to managing PT will hopefully keep athletes competing for their season.
References
1. British Journal of Sports Medicine 2009; 43(6), 409-16
2. Sport Health 2014; 32(1), 17-20
3. Journal of Physiotherapy 2014; ,60, 122–129
4. British Journal of Sports Medicine 2014; 48, 506–509
5. Best Practice & Research Clinical Rheumatology 2007; 21(2), 295–316
6. British Journal of Sports Medicine 2009; 43(6), 409-16
7. Journal of Science and Medicine in Sport 2008; 11, 235—238
1. British Journal of Sports Medicine 2009; 43(6), 409-16
2. Sport Health 2014; 32(1), 17-20
3. Journal of Physiotherapy 2014; ,60, 122–129
4. British Journal of Sports Medicine 2014; 48, 506–509
5. Best Practice & Research Clinical Rheumatology 2007; 21(2), 295–316
6. British Journal of Sports Medicine 2009; 43(6), 409-16
7. Journal of Science and Medicine in Sport 2008; 11, 235—238