Chiropractor, Dr. Alexander Jimenez looks at the surgical interventions required to manage a SLAP lesion and presents in-depth guidelines on the necessary post-surgical rehabilitation following a SLAP repair…
There are a number of varying types of treatment options available in different types of SLAP lesions. The type of lesion, the age of the athlete and the functional level of the athlete will determine the type of treatment plan prescribed for the SLAP lesion. Labrum repair, biceps tenodesis, debridement, tenotomy, and conservative treatment have all been recommended depending on the characteristics of the lesion.
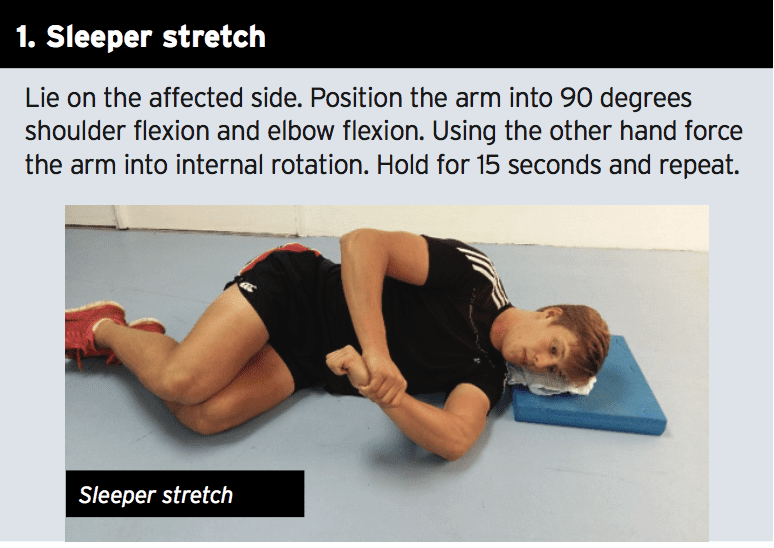
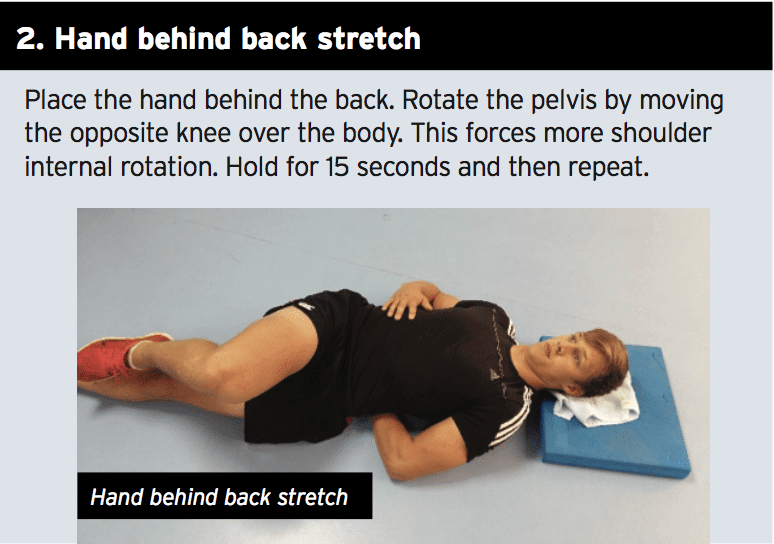
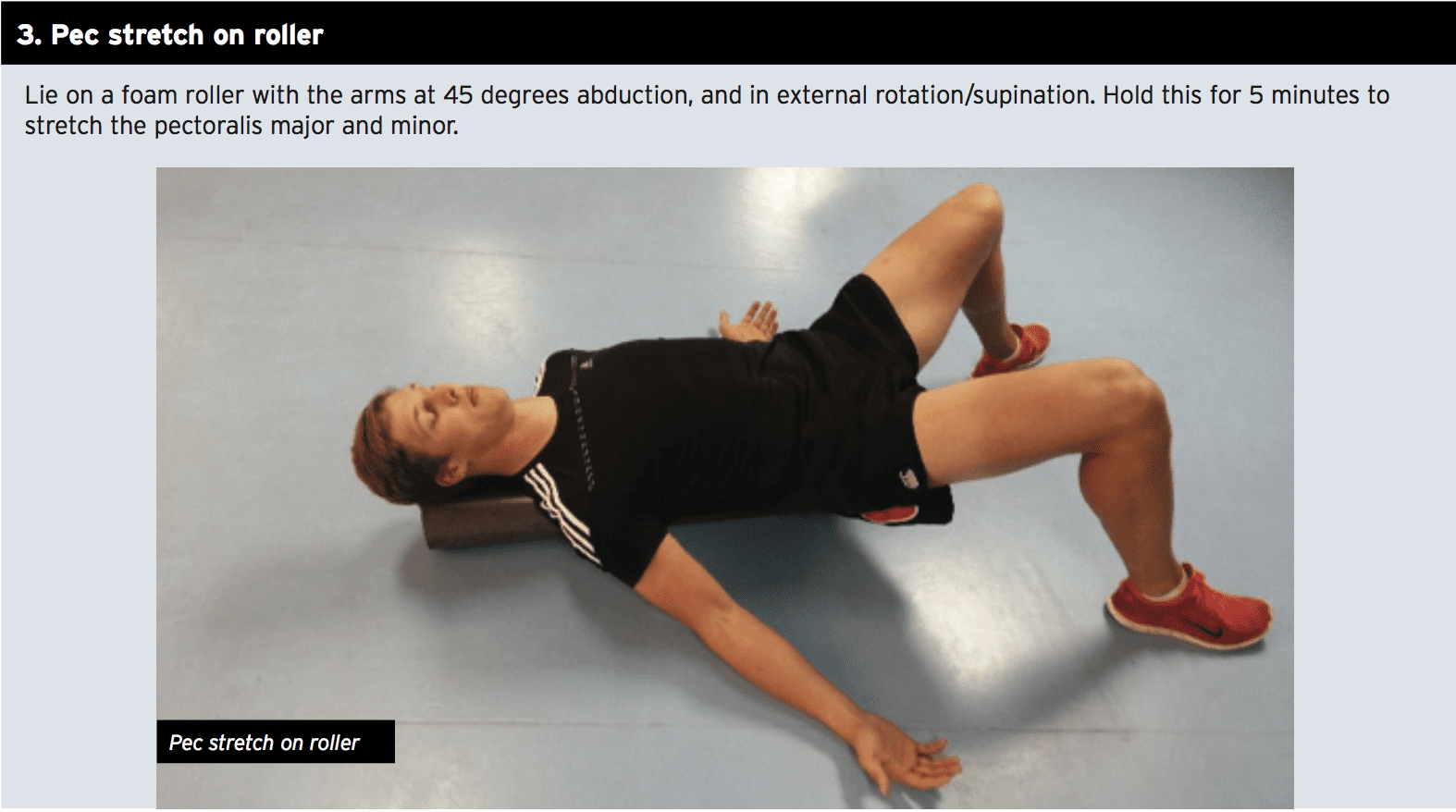
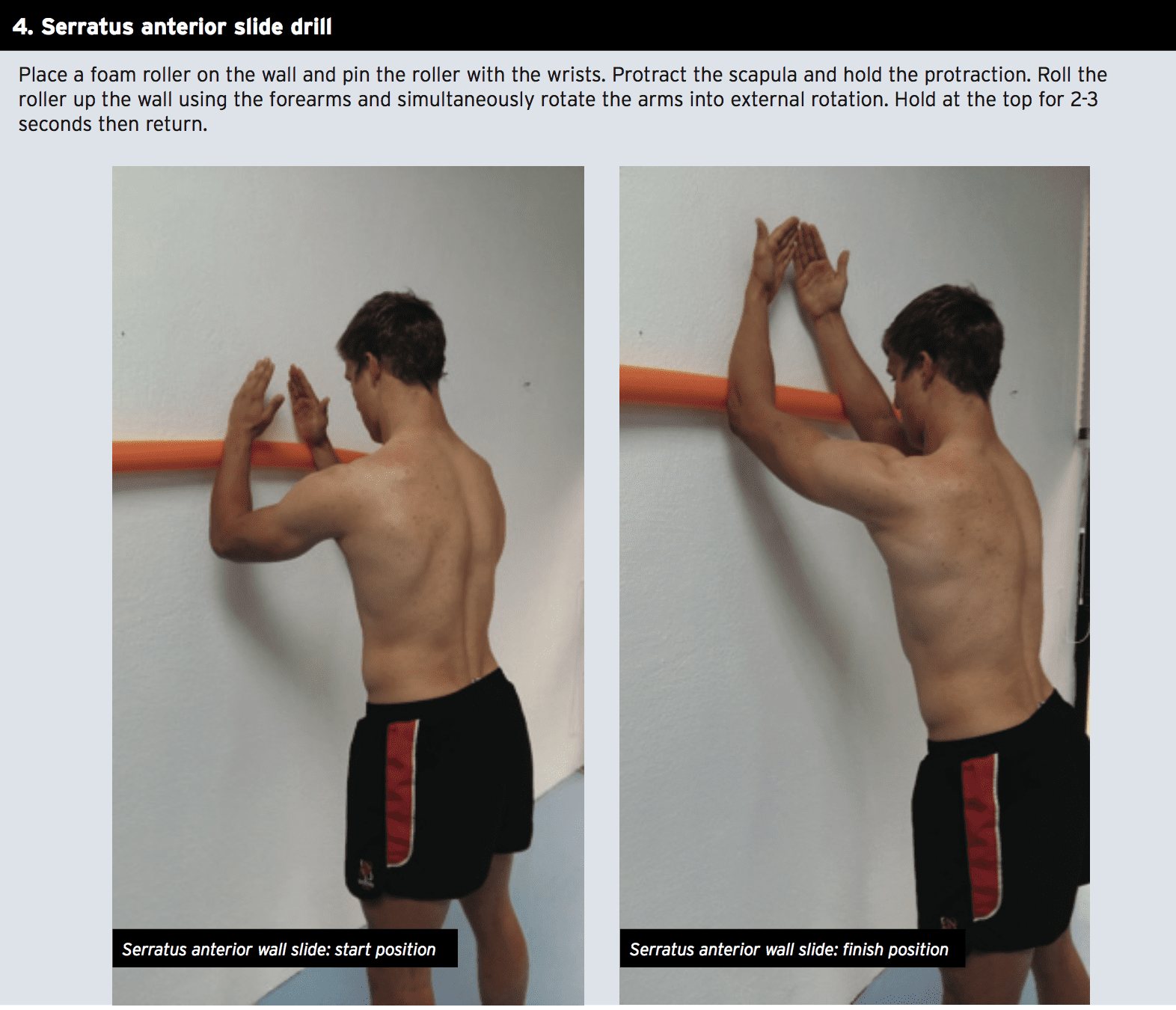
Many variations of SLAP lesions are initially treated conservatively with measures to primarily improve the patho- mechanical factors that impinge on the SLAP lesion such as glenohumeral internal rotation deficit (GHIRD) and scapular dyskinesis. For many of the lower-level type 1 lesions, this may be quite effective in eliminating the symptoms of the SLAP lesion without the need for surgery. However for the purposes of this article, the focus will remain on surgically treated SLAP lesions and their rehabilitation.
Surgery Types
Simple type-1 lesions may only require a simple debridement without disrupting the biceps anchor(1), whereas type-2 lesions are the most commonly seen type in sports medicine clinics, and these involve a detachment of the biceps anchor from the labrum. Type-2 lesions can be treated with arthroscopic fixation of the superior labrum to establish biceps anchor stability.Type 3 lesions are characterized by bucket-handle tears of superior labrum with intact biceps anchor. This bucket handle fragment can easily be debrided by an arthroscopic shaver, and repair is often not needed(2). However, if the type 3 lesion is associated with a Buford complex then it should be treated as a type 2 lesion(3). The other types of SLAP lesions are not as common as the type 2 lesions, although if they do exist will certainly need surgical intervention.
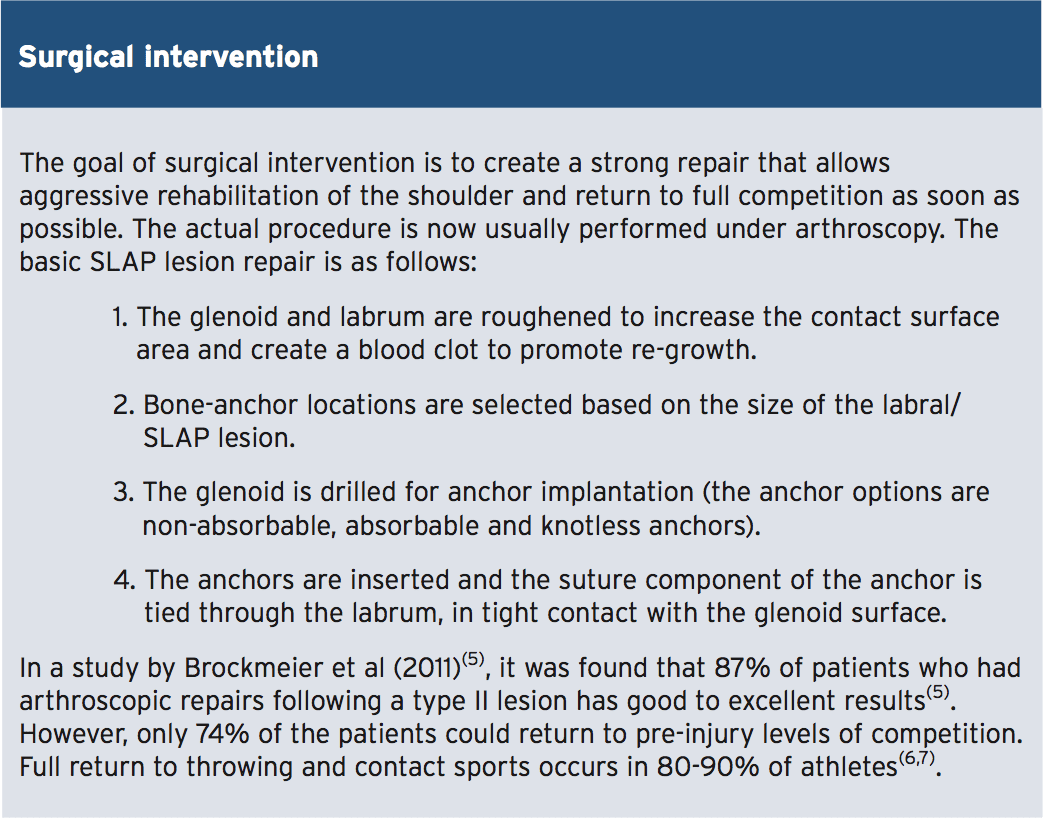
In a large database search of over 25,000 arthroscopic SLAP repairs, Zhang et al (2012) found that the highest incidence of repair is in the 20-29 years and 40-49 years of age groups(4). This may reflect how the younger population are more likely to be involved in sports and other activities where they may suffer an acute SLAP lesion. In the 40-49 year old group however, the high incidence is most likely down to the degeneration of the labrum, which may be initially make its presence felt around this age. Also there is a significant gender difference, with men having three times higher incidence of repair. This probably reflects how males are more likely to play a sport, or behave in a way that may lead to a SLAP lesion.
Rehabilitation
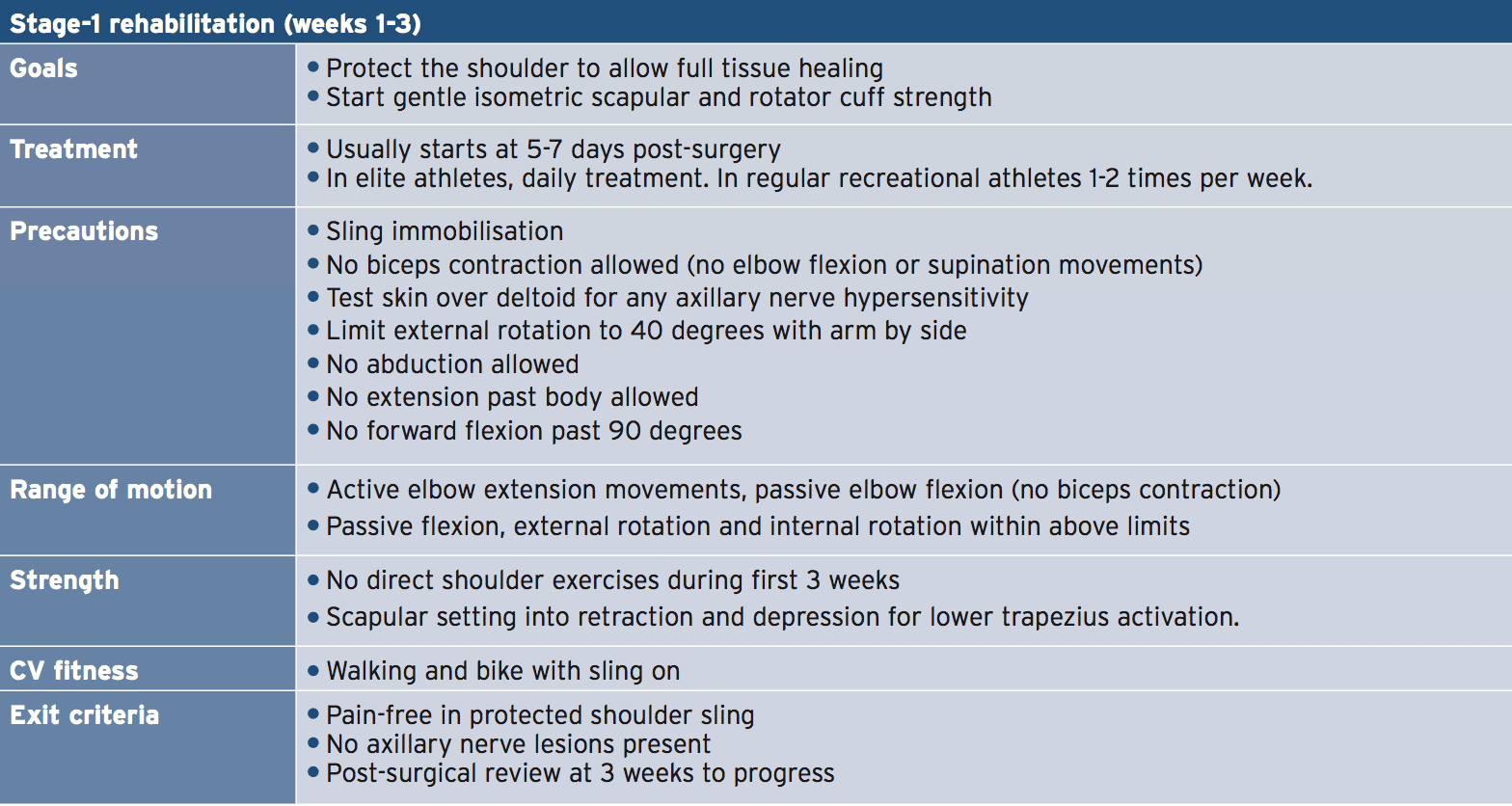
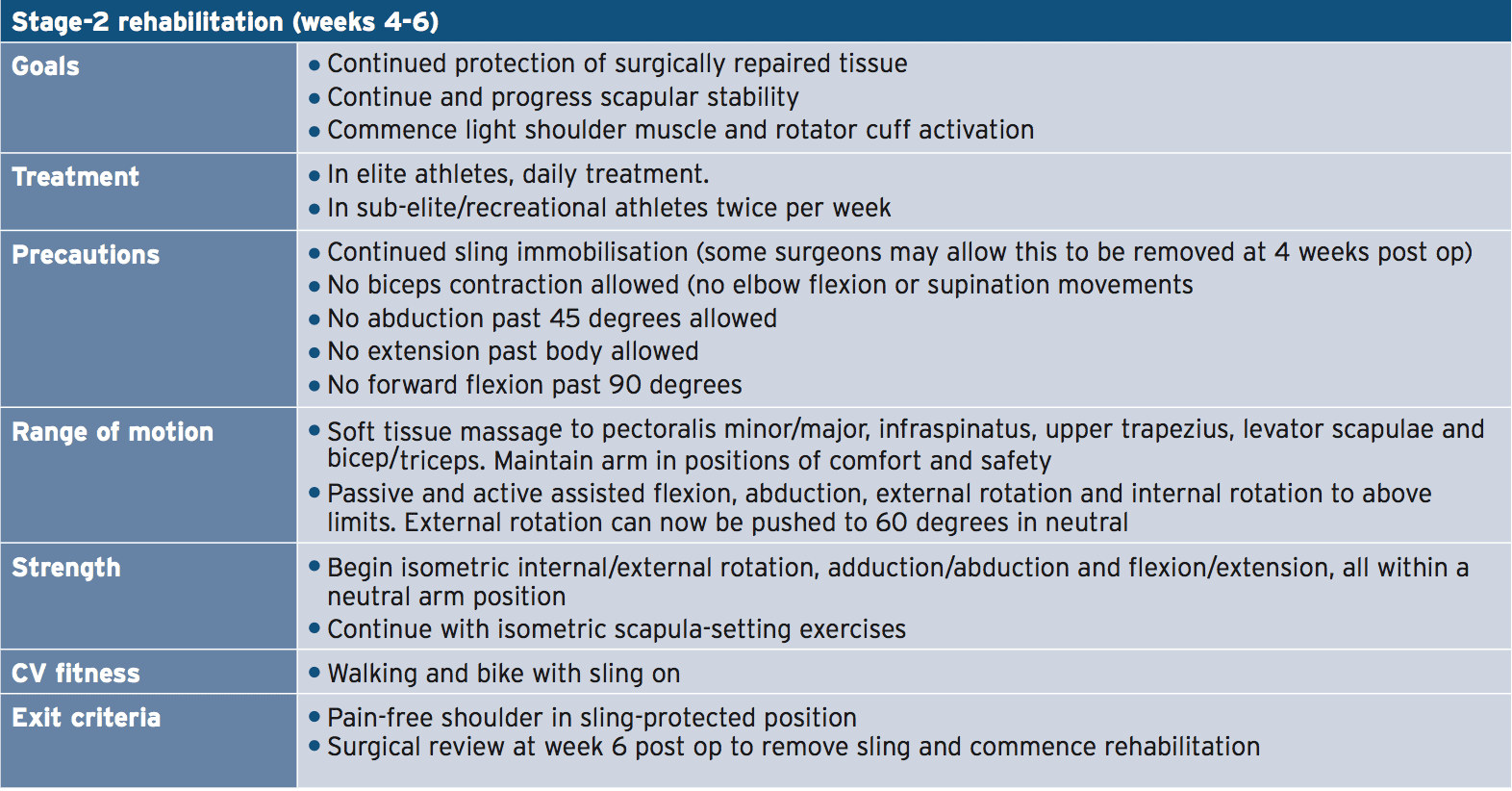
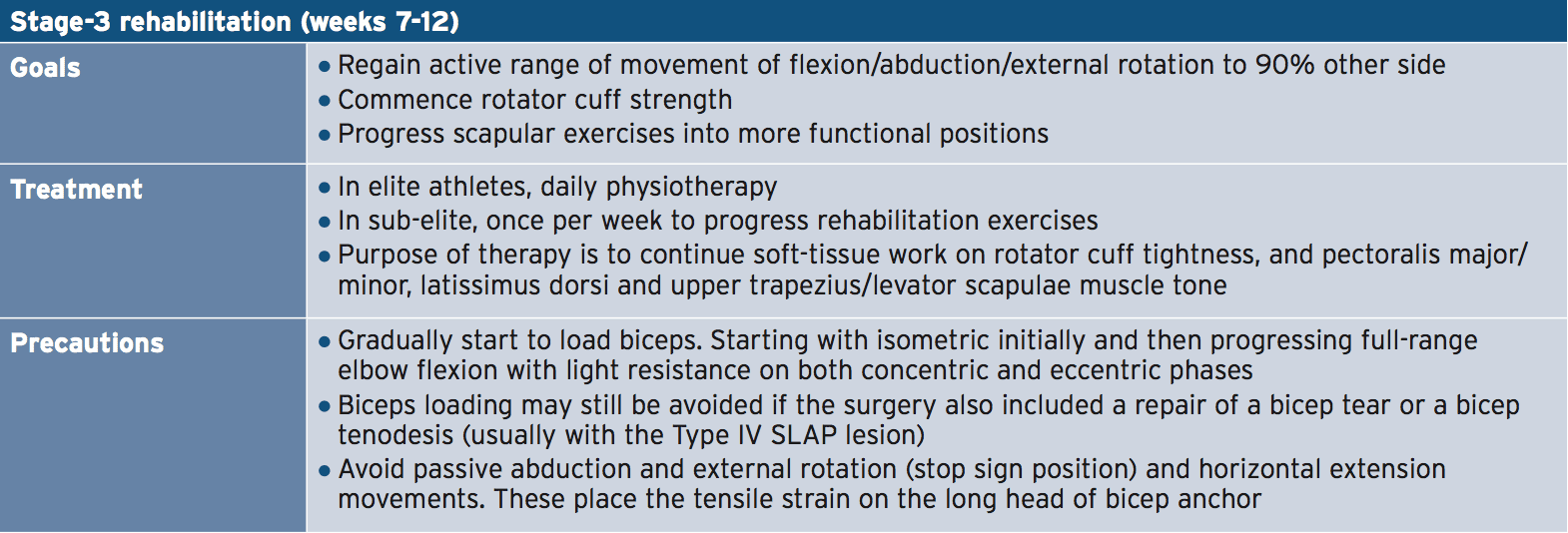
A number of guidelines have been proposed when managing post-operative SLAP lesions based on the original mechanism of injury(8). These include:1. In injuries sustained due to a compressive mechanism, subjects need to avoid weight bearing exercises on the limb in the early stages to avoid the compression and shear effect on the labrum.
2. In injuries sustained due to a sudden traction, subjects need to avoid any heavy eccentric biceps load to minimise the traction effect on the biceps anchor.
3. In injuries sustained due to a ‘peel- back’ mechanism, subjects need to avoid excessive shoulder external rotation in the early post-surgical period.
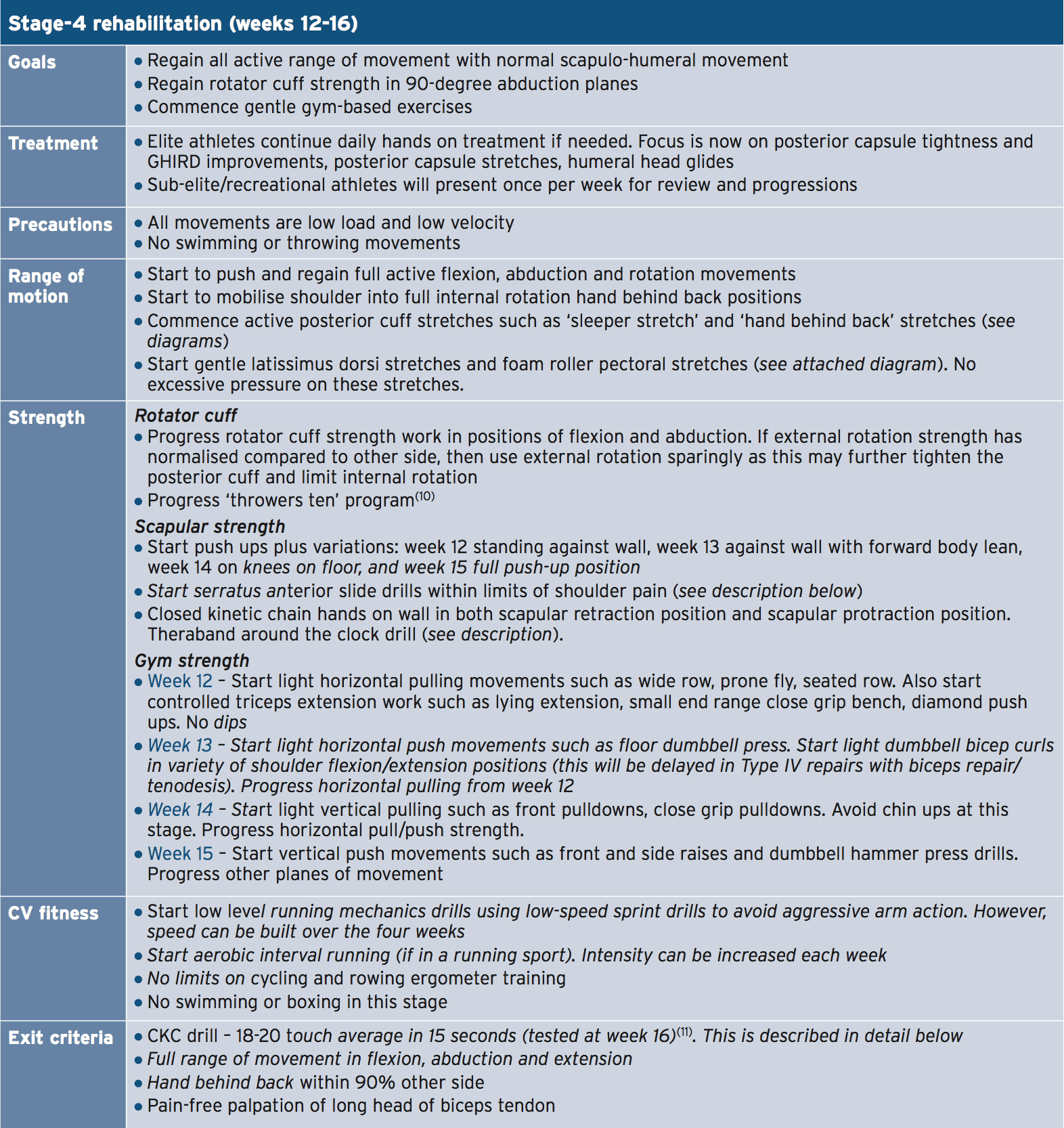
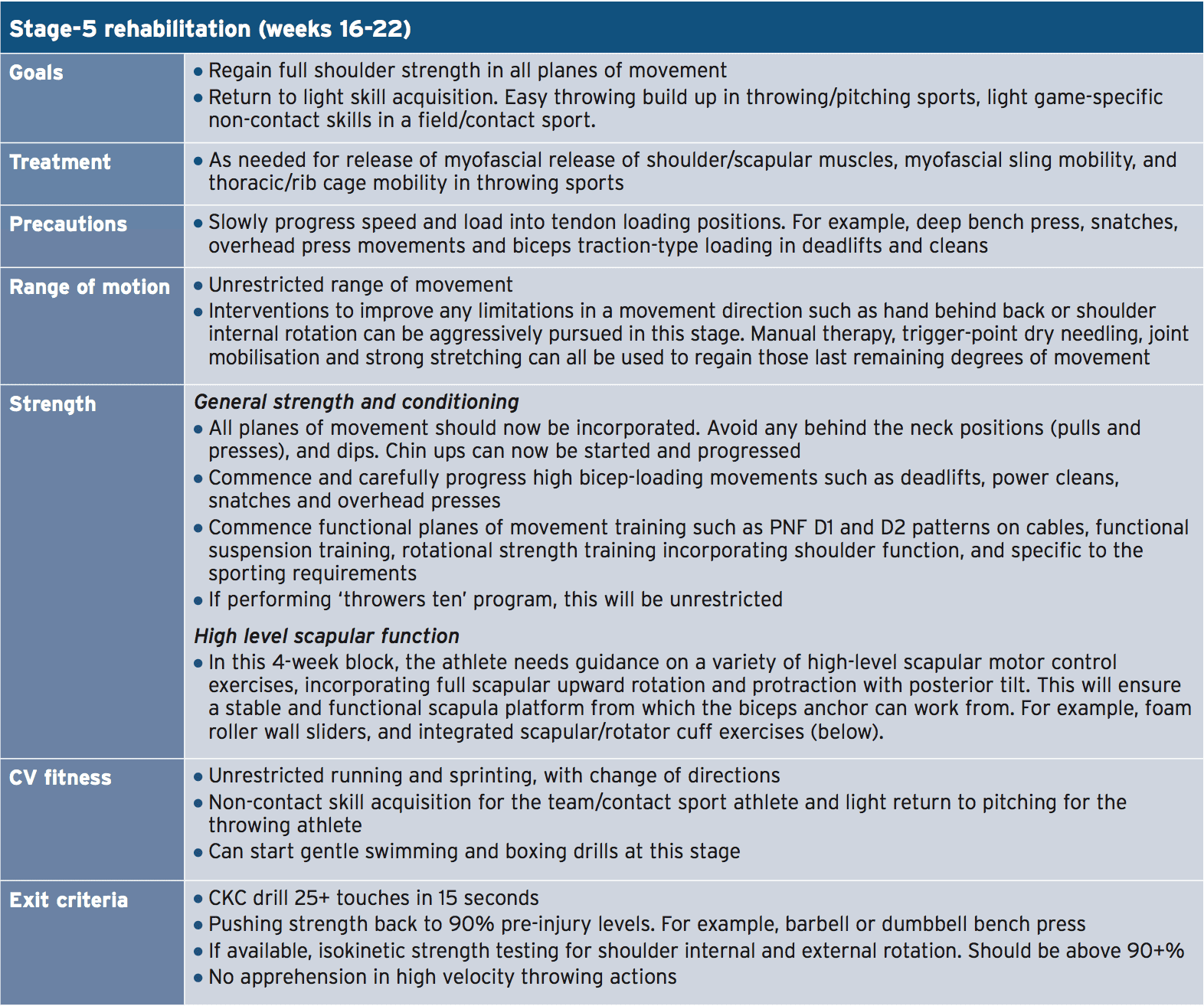
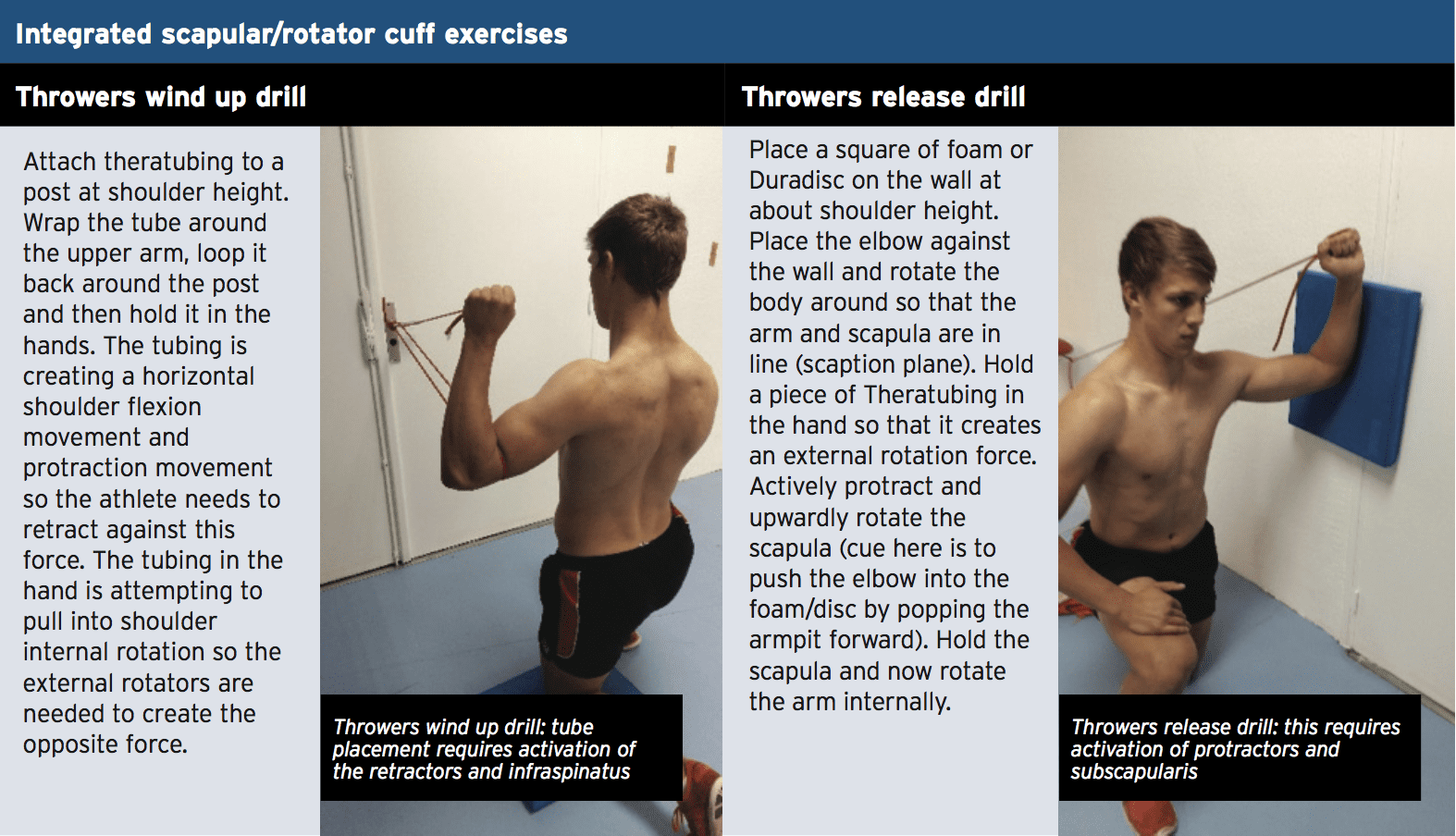
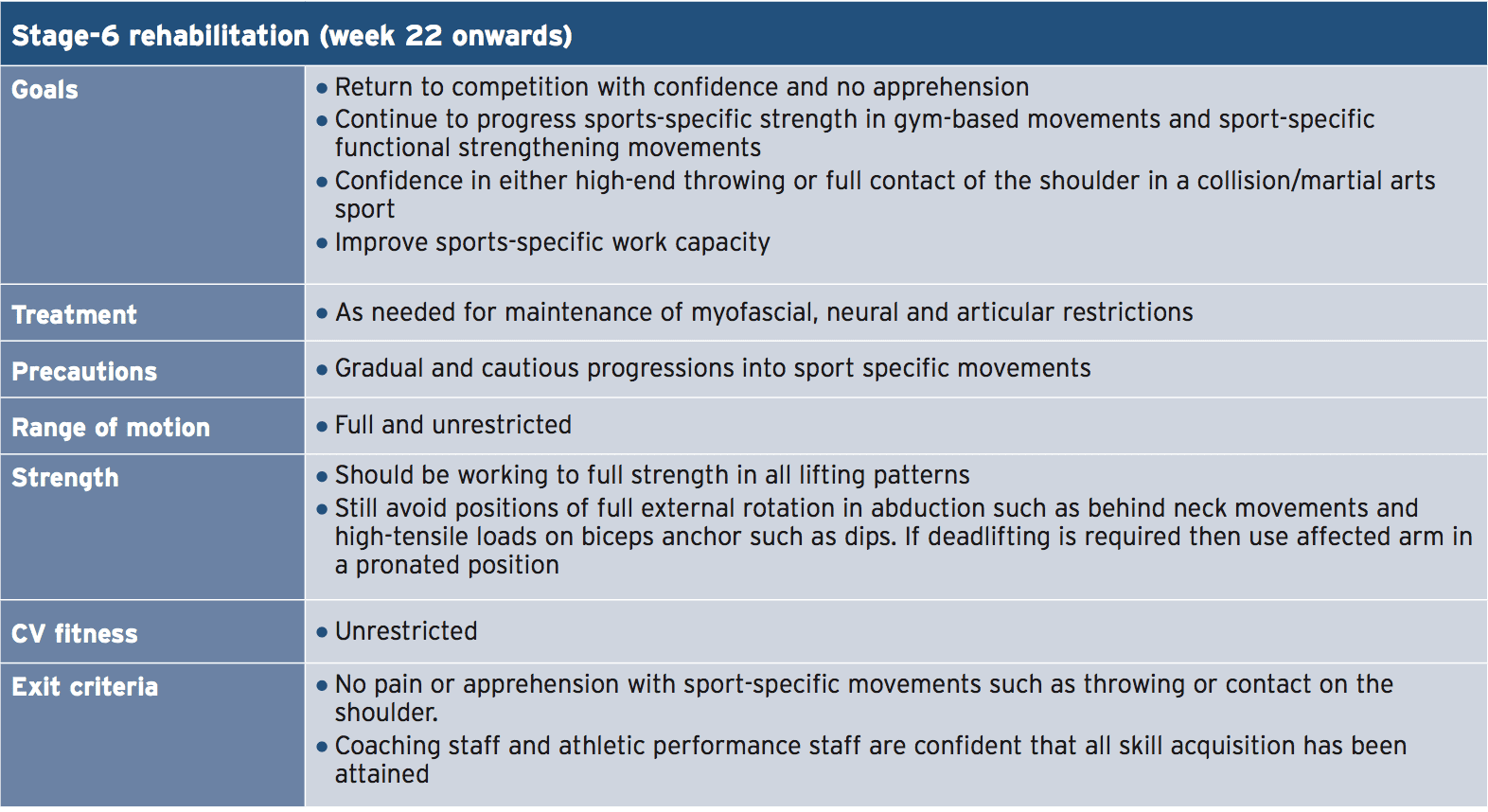
With these guidelines in mind, the general rehabilitation plan is staged over six phases. Although time frames have been approximated for each stage, the key decision to move from one stage to the next is the achievement of the exit criteria listed at the end of each stage. In general terms, throwing and contact sport athletes will usually return to competition at 6-9 months post-surgery, depending on the athlete and the sport.
Summary
SLAP lesions are a reasonably common injury in the throwing athlete and can also be a source of shoulder pain in the contact athlete. Type II SLAP lesions are more common and will usually require surgical intervention. The rehabilitation program following this type of injury may be quite lengthy and detailed and most athletes will return to sport at six to nine months following surgery.References
1. Am J Sports Med 2003; 31: 798-810
2. Clin Orthop Relat Res 2001; (390): 73-82
3. Am J Sports Med 1995; 23: 93-98
4. Am J Sports Med 2012; 40: 1144-1147
5. J Bone Joint Surg Am. 2009;91:1595-603
6. Clin Sports Med. 2004;23(3):321-334, vii
7. Clin J Sport Med. 2007;17(1):1-4
8. The Int J of Sports Phys Th. 2013. 8(5). Pp 579-600
9. N Am J Sports Phys Ther. 2008. 3 (2): 95–106
10. Phys Sportsmed.2011;39(4):90-7
11. North American Journal of Sports Physical Therapy. 2007. 2(3); 159-163




