Chiropractor Dr. Alexander Jimenez brings insights and explores the causes of cervicogenic dizziness in athletes, how to diagnose and effective treatment options.
Dizziness is a very common complaint in clinical practice, affecting approximately 20-30% of the general population(1). It can manifest as faintness, unsteadiness, a perception of spinning, and disorientation(2). The mechanisms causing these symptoms are multiple, and can involve several different organ systems. In particular, dizziness can be experienced from disturbances of the ear, nose and throat; cardiovascular system; and central nervous system (CNS)(1,3).
More commonly in sport however, is the association of dizziness in 20-58% of athletes who sustain a traumatic cervical flexion-extension injury or ‘whiplash’ injury(1,2,4). This can occur due to dysfunction in the upper cervical spine and sensorimotor control disturbances(1,5). This specific type of dizziness is referred to as cervicogenic dizziness (CGD)(2).
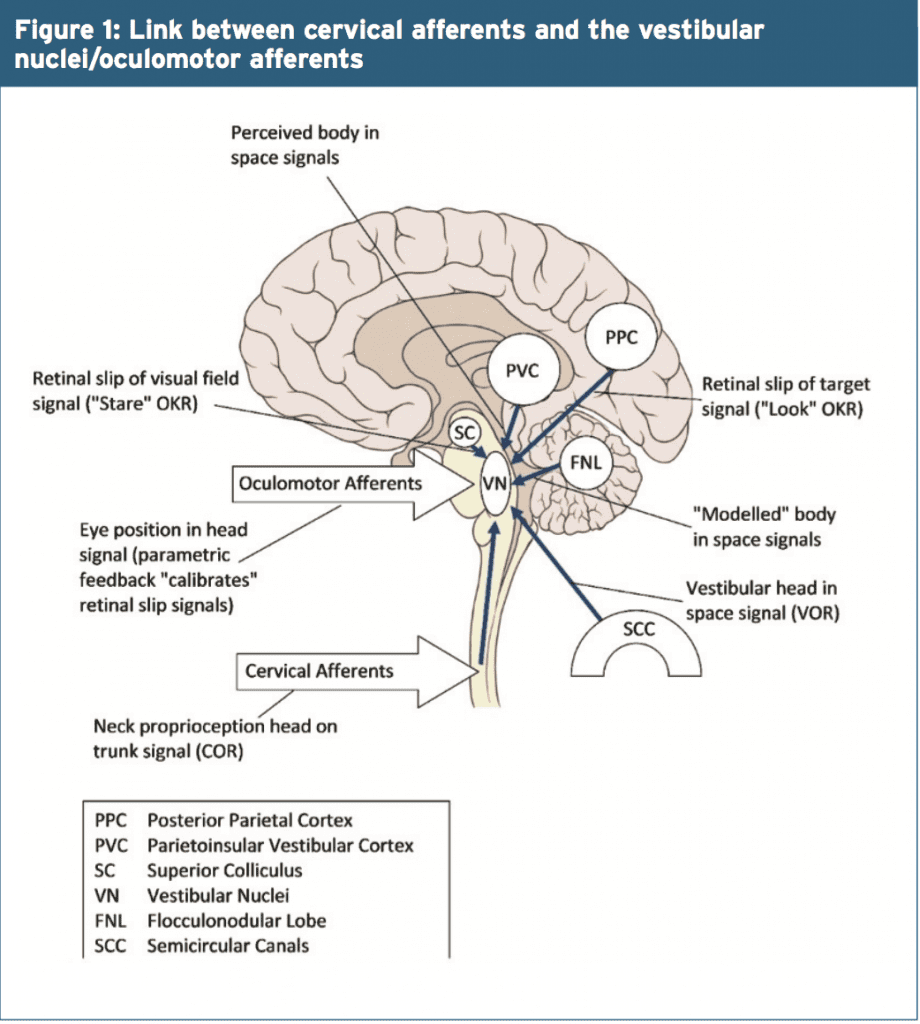
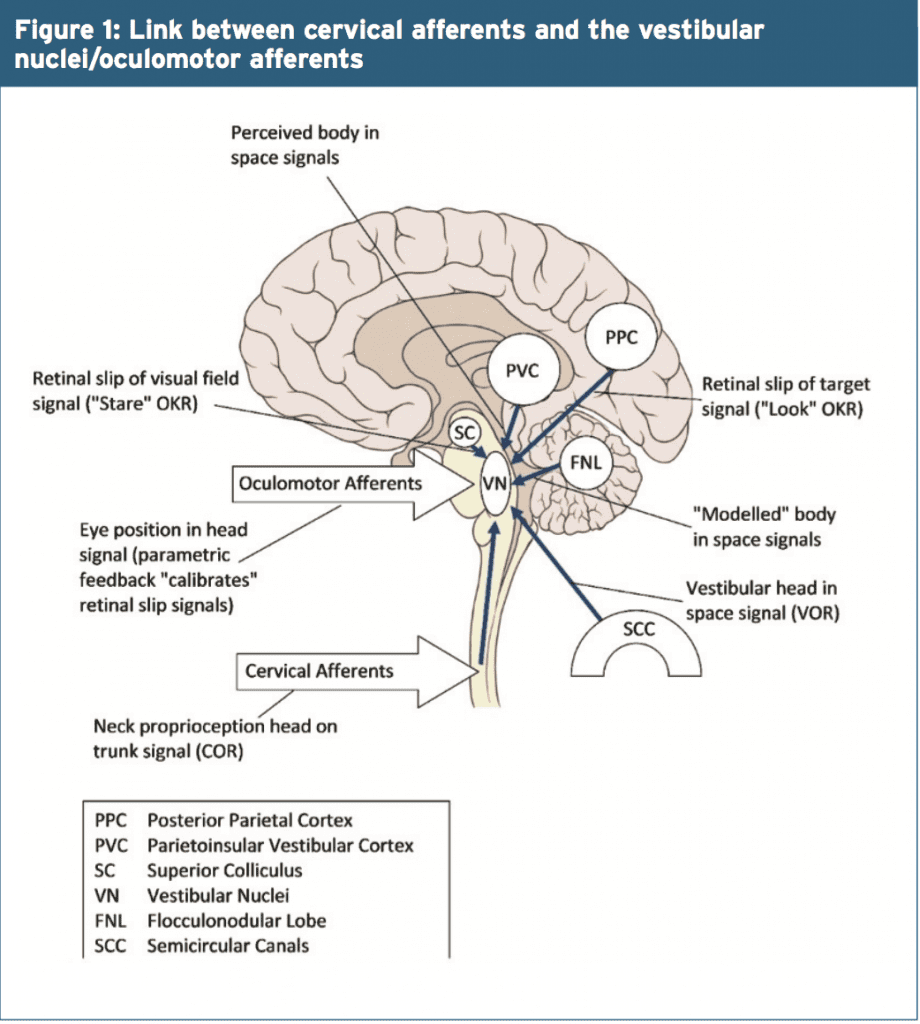
The proposed mechanism for the above- mentioned characteristics are a result of changes to excitation levels of cervical somatosensory receptors. This is caused by neck pain or trauma, and leads to a sensory mismatch between vestibular and cervical input(2,7). Literature supports the presence of a strong connection between cervical dorsal roots and the vestibular nuclei (see Figure2) particularly at levels C2 and C3 (3,4).
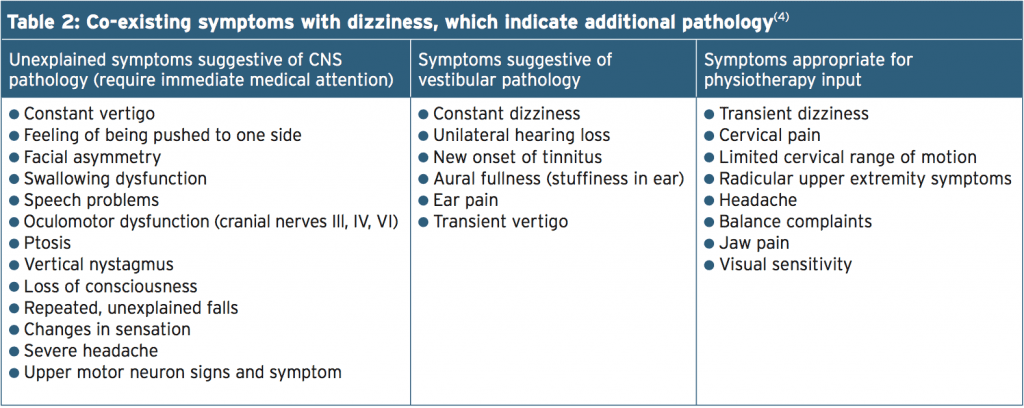
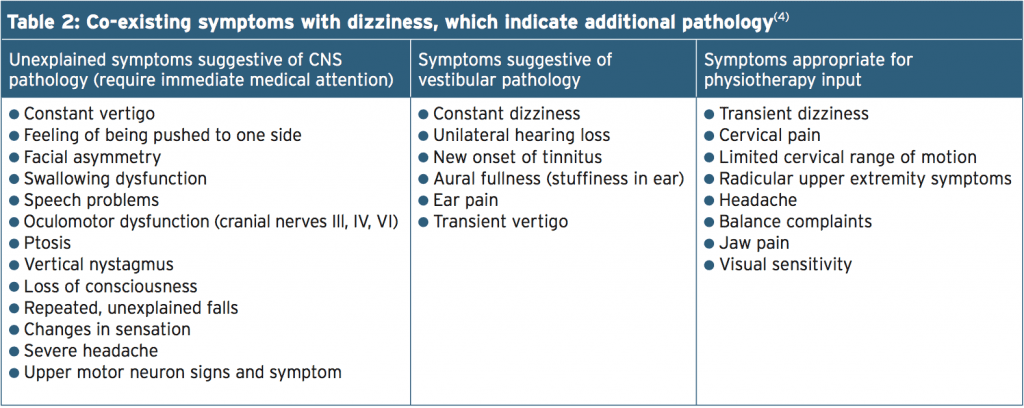
Table 2 lists co-existing symptoms that should be explored further because they are suggestive of CNS or inner ear (vestibular) pathology. Such symptoms would require further investigation and would not be appropriate for physiotherapy treatment(4).
Another pathology which can cause dizziness and unsteadiness, and which should not be misdiagnosed is damage to the vertebral artery or vertebrobasilar arterial injury. This can be present following head and neck trauma(4,5). If there is any suspicion of vascular involvement, a clinical framework has been proposed providing an accurate guideline for assessment and management(9). Likewise, it is worth noting that dizziness can be caused by elevated anxiety and medication intake as well(5).
The purpose of this scale is to identify difficulties that someone may be experiencing because of dizziness. Although this assessment is not specific to athletes, it can be helpful as a valid and reliable outcome measure(5,7,10).
Other measurable outcomes for symptoms can include a 5-point scale for intensity of dizziness (0=no, 1=mild, 2=moderate, 3=severe, and 4=very severe(6). Similarly, frequency of dizziness can be measured on a 6-point scale (0=no dizziness, 1=dizziness less than once per month, 2=1-4 episodes of dizziness per month, 3=1-4 episodes per week, 4=once daily, and 5=more than once per day or constant)(7).
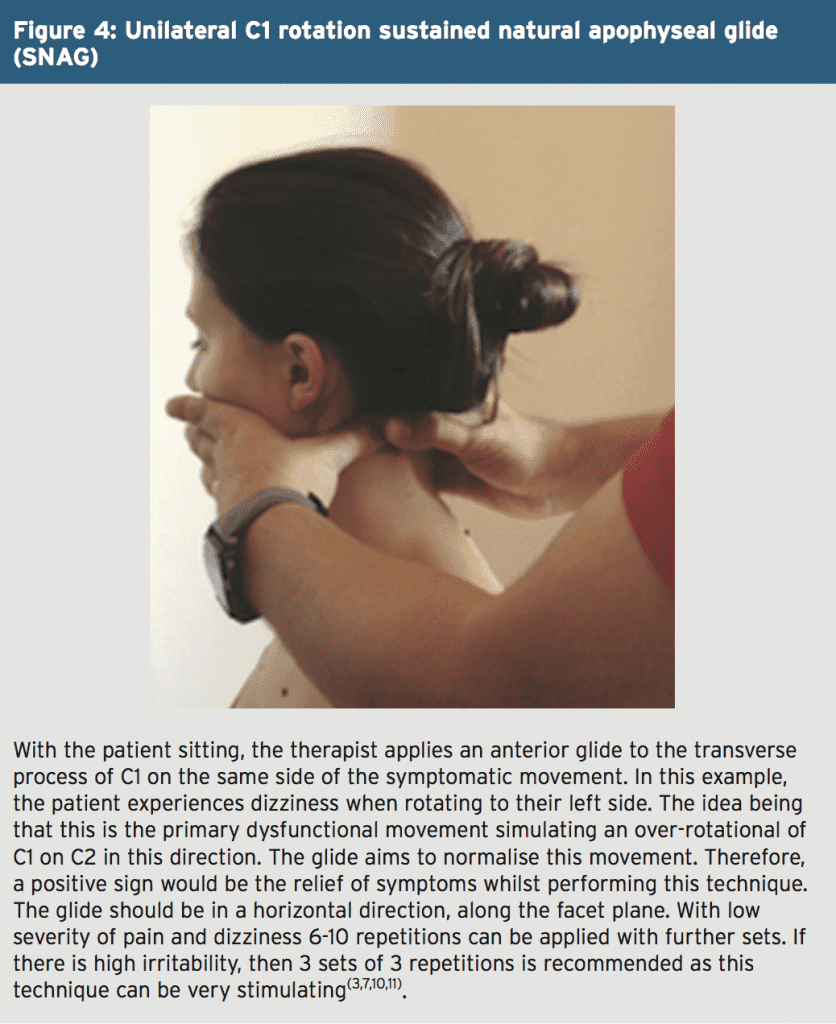
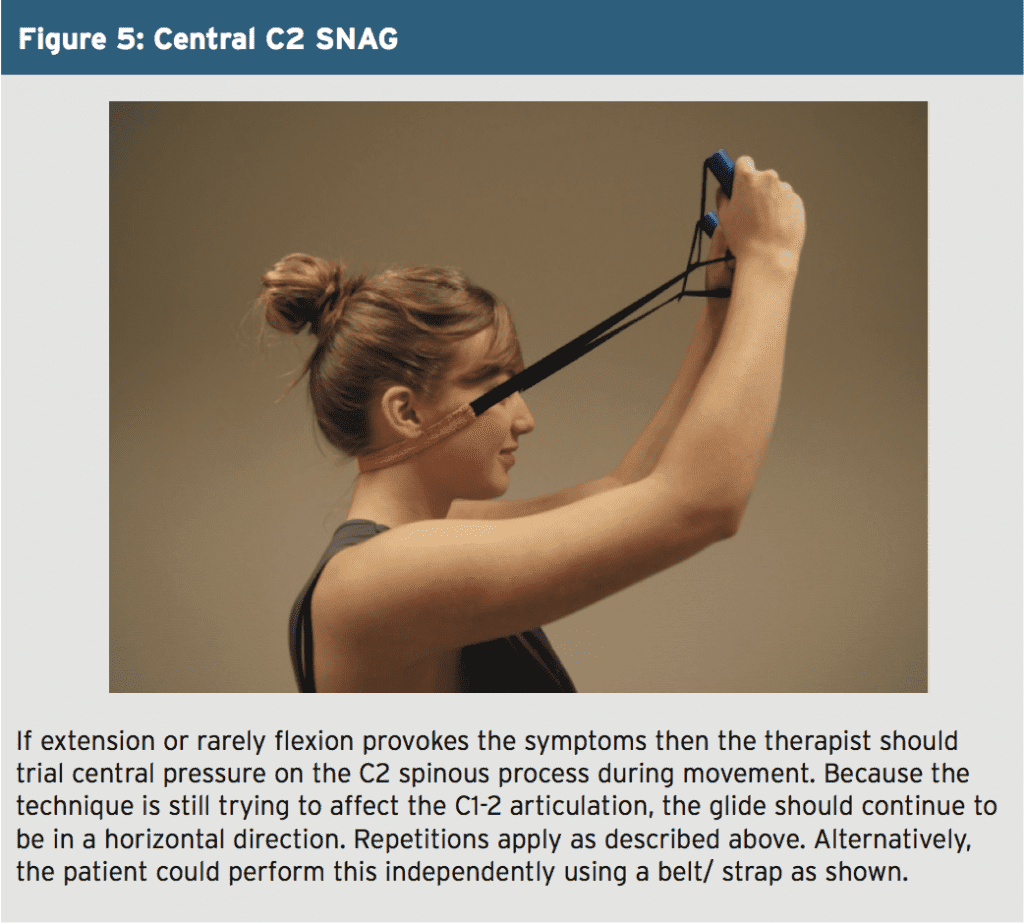
With this in mind, cervical spine mobilisation techniques (sustained natural apophyseal glides, and Maitland mobilisations) have been shown to be effective in restoring normal movement of the zygapophyseal joints. The benefits include a reduction in pain and muscle hypertonicity, which helps re-establish normal proprioceptive and biomechanical functioning to the cervical spine(1,3,10).
If these techniques described above are successful then a self-SNAG (as described in issue 159) can be recommended for the patient to try at home using a towel or belt/ strap. In general, it has been proposed that these techniques should be utilised over a course of four to six sessions, which should produce a long-term reduction in symptoms(3,7,10). Combining these manual techniques with sensorimotor control rehabilitation, as described previously, is recommended by the majority of literature(1,5,6,8);however, remains inconclusive in a minority of research(2).
When diagnosed correctly, there is good support for the use of manual therapy techniques to produce a long-term reduction in symptoms. Given the prevalence of sensorimotor control disturbances associated with dysfunction to the upper cervical spine, the addition of sports-specific rehabilitation focusing on regaining this control can be clinically justified.
References
1. Pain Phys. 2015. 18: 583-595
2. Chiro & Man Th. 2011. 19-21
3. Man Th. 2005. 10: 4-13
4. JOSPT 2000. 30(12): 755-766
5. Man Th. 2008. 13: 2-11
6. Dis & Rehab. 2007. 29(15): 1193-1205
7. Man Th. 2008. 1-11
8. Arch Phys Med Rehabil. 1996. 77: 874-882
9. Manual Th. 2014. 19: 222-228
10. Phys Th. 2014. 94(4): 466-476
11. JOSPT. 2010. 40(4): 225-229
More commonly in sport however, is the association of dizziness in 20-58% of athletes who sustain a traumatic cervical flexion-extension injury or ‘whiplash’ injury(1,2,4). This can occur due to dysfunction in the upper cervical spine and sensorimotor control disturbances(1,5). This specific type of dizziness is referred to as cervicogenic dizziness (CGD)(2).
Presentation
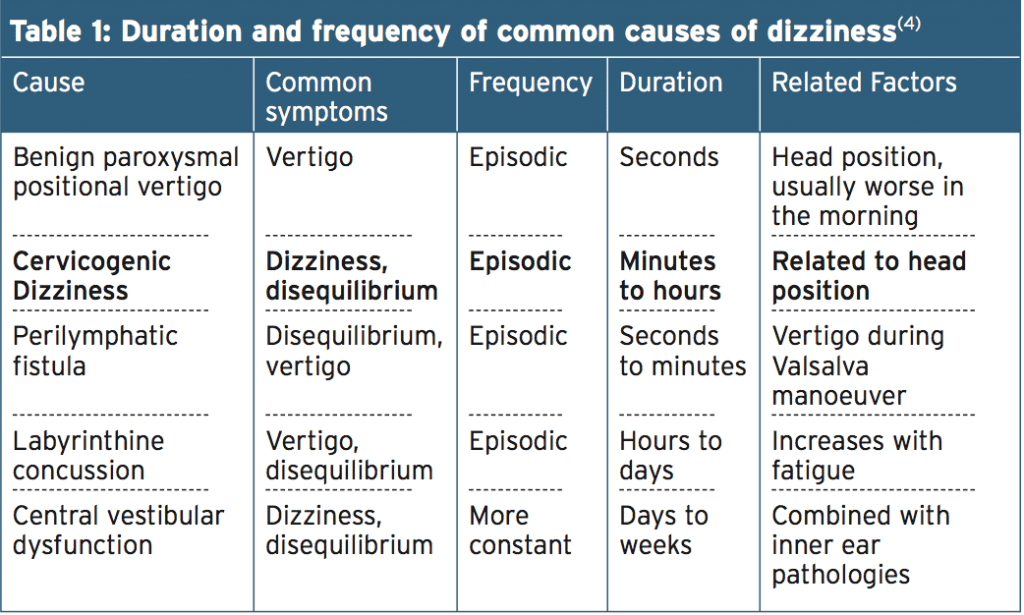
Table 1 gives an idea of how to distinguish dizziness with cervicogenic origin from that of other causes. In addition, common distinguishing features of CGD include associated neck pain, restricted cervico- thoracic range of motion, and headaches(4,6). Furthermore, hypertonicity to dorsal soft tissue (particularly suboccipital musculature) and positive pain provocation with palpation to cervical zygapophyseal joints are likely(6). Further disturbances with cervical joint positional sense, postural stability, and oculomotor control, such as altered smooth pursuit and saccadic eye movements, can also present with this disorder(5).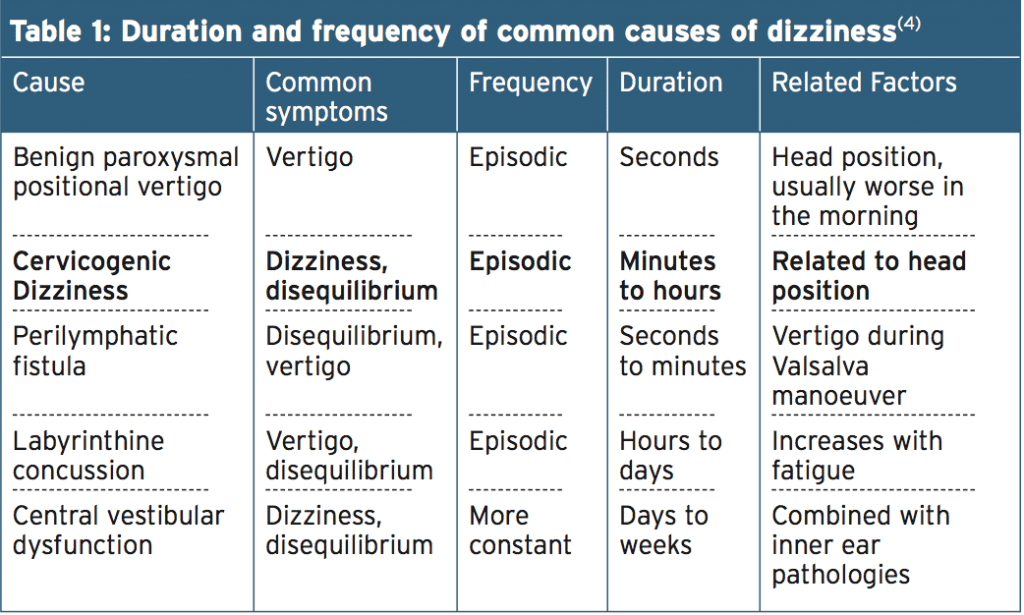
The proposed mechanism for the above- mentioned characteristics are a result of changes to excitation levels of cervical somatosensory receptors. This is caused by neck pain or trauma, and leads to a sensory mismatch between vestibular and cervical input(2,7). Literature supports the presence of a strong connection between cervical dorsal roots and the vestibular nuclei (see Figure2) particularly at levels C2 and C3 (3,4).
The cervical afferents are also involved in three reflexes influencing head, eye, and postural stability/proprioception: the cervico-collic reflex, the cervico-ocular reflex, and the tonic neck reflex(5). In addition, there is an abundance of mechanoreceptors in the ‘y-muscle’ spindles of the deep segmental upper cervical muscles, which if sensitised by trauma, leads to alterations of proprioceptive signalling to the CNS (Figure 1)(1,8). With this in mind, it is understandable that injury or trauma of the neck may be associated with a sense of dizziness or disequilibrium.
Diagnosis
As a result of the previously mentioned competing pathologies, it can be difficult to diagnose the primary cause of dizziness. Obtaining a thorough history from a patient presenting with dizziness is therefore critical to making a decision regarding appropriate care(2,4,5,8). To entertain a diagnosis of CGD, the therapist must be able to correlate the onset and diagnosis of the dizziness symptoms with the neck pain or dysfunction (ie with cervical movements(4). Commonly, the most provocative cervical movement is extension; however, CGD can be reproduced with rotation or (more rarely) flexion(7).Table 2 lists co-existing symptoms that should be explored further because they are suggestive of CNS or inner ear (vestibular) pathology. Such symptoms would require further investigation and would not be appropriate for physiotherapy treatment(4).
Another pathology which can cause dizziness and unsteadiness, and which should not be misdiagnosed is damage to the vertebral artery or vertebrobasilar arterial injury. This can be present following head and neck trauma(4,5). If there is any suspicion of vascular involvement, a clinical framework has been proposed providing an accurate guideline for assessment and management(9). Likewise, it is worth noting that dizziness can be caused by elevated anxiety and medication intake as well(5).
The purpose of this scale is to identify difficulties that someone may be experiencing because of dizziness. Although this assessment is not specific to athletes, it can be helpful as a valid and reliable outcome measure(5,7,10).
Other measurable outcomes for symptoms can include a 5-point scale for intensity of dizziness (0=no, 1=mild, 2=moderate, 3=severe, and 4=very severe(6). Similarly, frequency of dizziness can be measured on a 6-point scale (0=no dizziness, 1=dizziness less than once per month, 2=1-4 episodes of dizziness per month, 3=1-4 episodes per week, 4=once daily, and 5=more than once per day or constant)(7).
Assessment
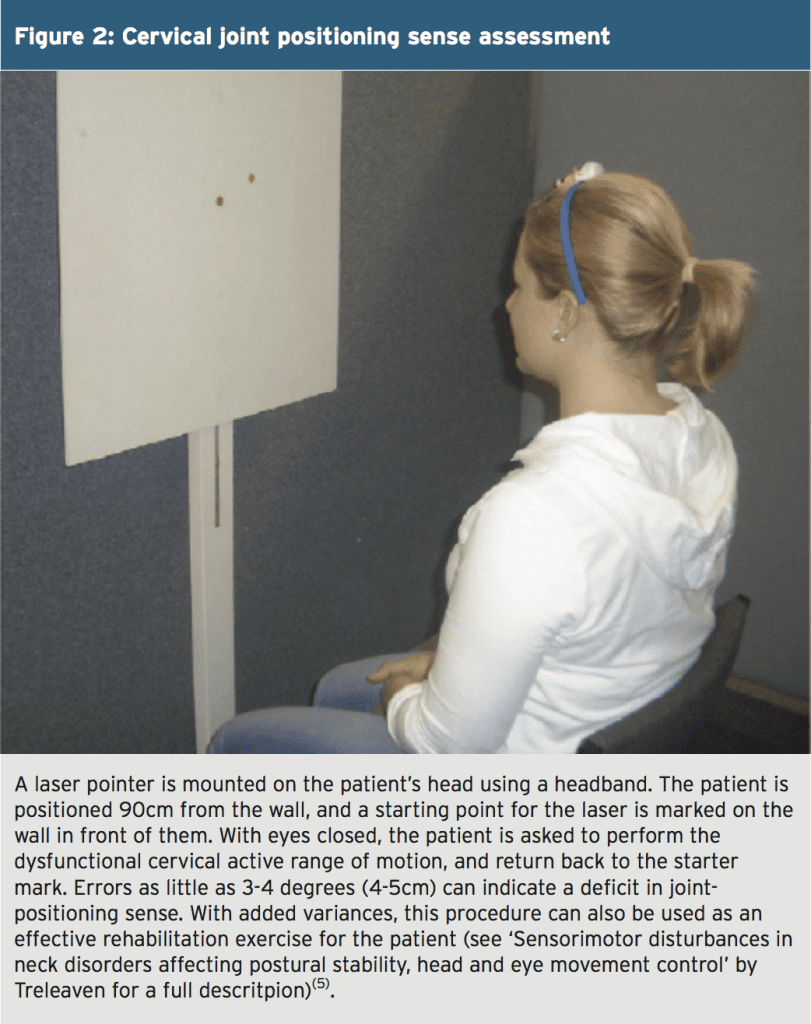
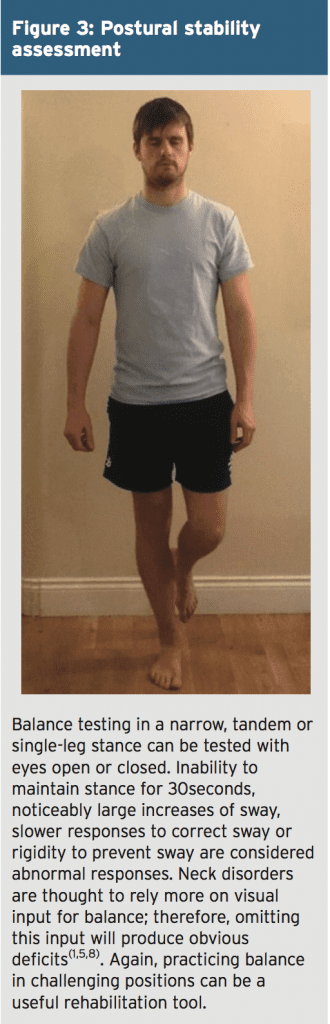
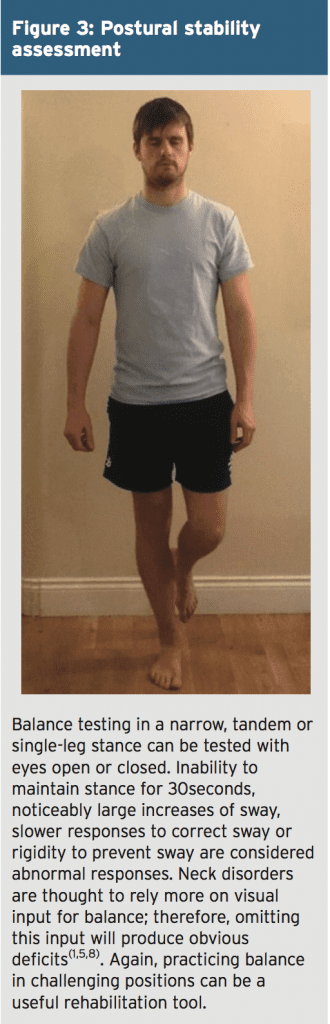
Pain provocation and disruptions to cervico-thoracic range of movement can be assessed using a neuromusculoskeletal objective assessment, while the effect on CGD symptoms is monitored. To gauge any additional sensorimotor control disturbances however, clinical assessment of cervical joint position sense (Figure 2), oculomotor control, and postural instability or balance/ proprioception can be very useful(1,2,4,5).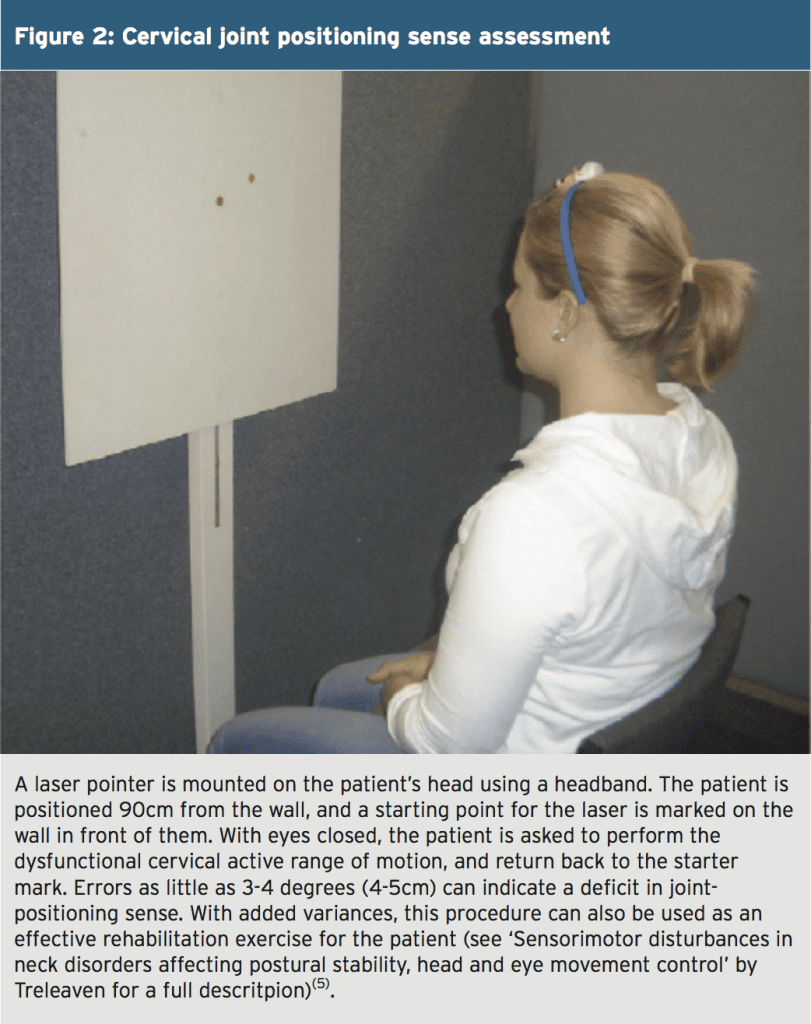
Oculomotor Control Assessment
This includes gaze stability (the ability to maintain gaze of a target while the head is moving), smooth pursuit (eyes follow a target whilst keeping the head still), saccadic eye movements (eyes fixed on a target that is moved quickly), and eye/head coordination (maintaining gaze when both the head and eyes are moving in between two targets – leading with the eyes first). Symptom provocation is a positive test, as well as, noting any abnormal coordination of the task(5). Similarly, these tests can be used for rehabilitation, and with appropriate adaptation, can be made more functional to sporting tasks.Treatment
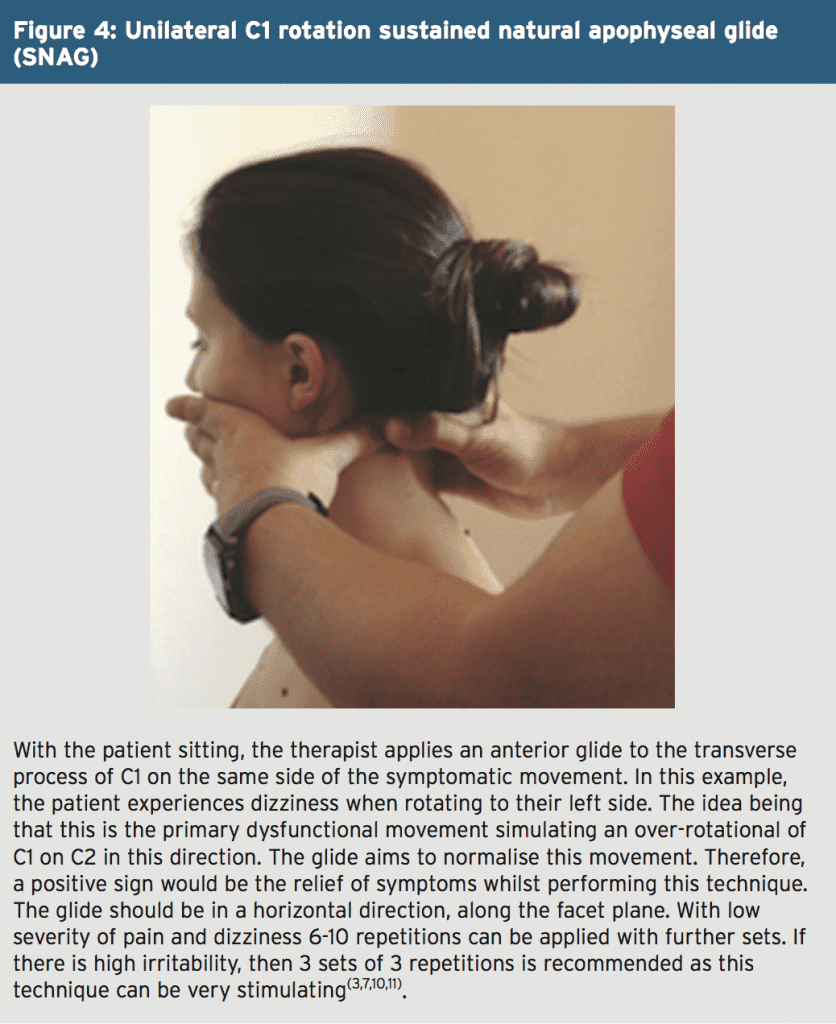
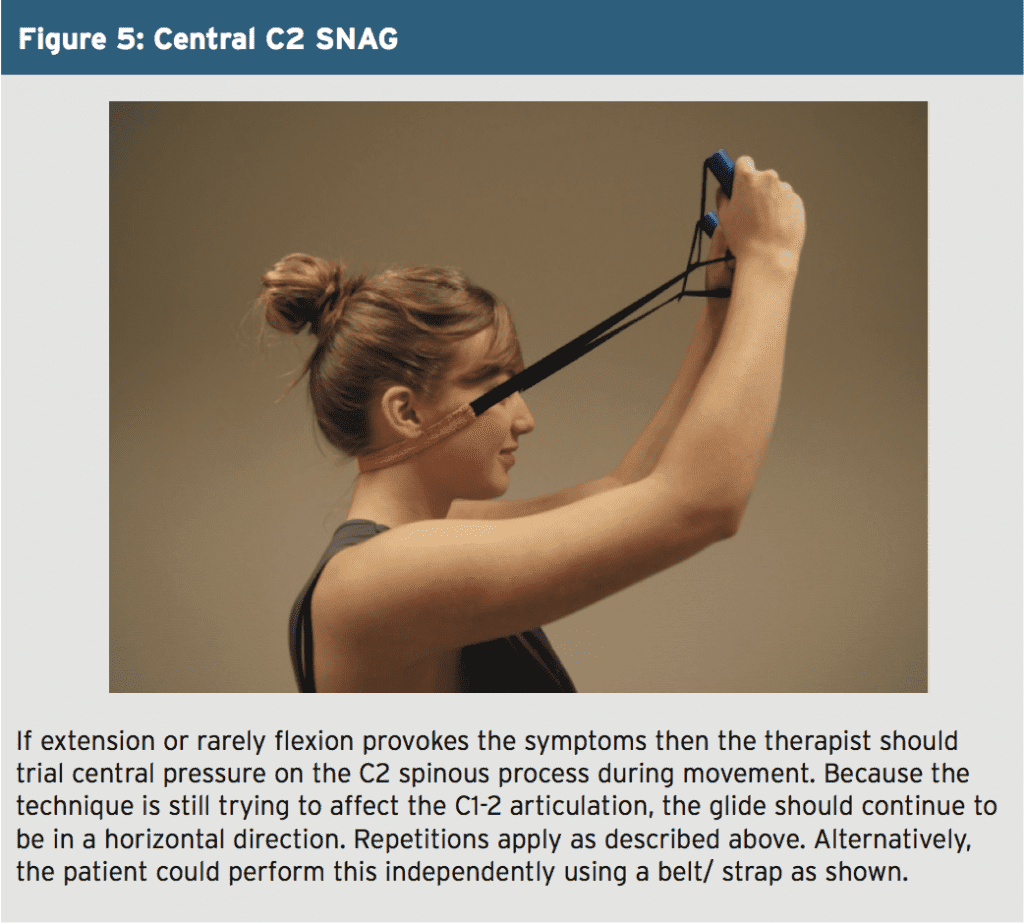
Researchers have argued that once a confident diagnosis has been achieved, management of CGD should be the same as for cervical pain, supporting the role of manual therapy for long-term benefits(1-4,6-8,10). Following trauma, it is thought that type 1 cervical articular mechanoreceptor and proprioceptors from dysfunctional joints results in a loss of normal afferent input. This leads to aberrant information being sent to the vestibular nuclei, thus formulating symptoms similar to vestibular disturbances, such as dizziness(3).With this in mind, cervical spine mobilisation techniques (sustained natural apophyseal glides, and Maitland mobilisations) have been shown to be effective in restoring normal movement of the zygapophyseal joints. The benefits include a reduction in pain and muscle hypertonicity, which helps re-establish normal proprioceptive and biomechanical functioning to the cervical spine(1,3,10).
If these techniques described above are successful then a self-SNAG (as described in issue 159) can be recommended for the patient to try at home using a towel or belt/ strap. In general, it has been proposed that these techniques should be utilised over a course of four to six sessions, which should produce a long-term reduction in symptoms(3,7,10). Combining these manual techniques with sensorimotor control rehabilitation, as described previously, is recommended by the majority of literature(1,5,6,8);however, remains inconclusive in a minority of research(2).
Summary
CGD is a diagnosis characterised by dizziness and disequilibrium, which is associated with neck pain, most commonly following neck trauma, such as forced cervical flexion-extension mechanisms in sport. The diagnosis relies on the basis of history and examination, and should prioritise the exclusion of other possible causes of dizziness, including involvement of the CNS, cardiovascular, and vestibular systems. Physiotherapy intervention is not appropriate if there is any suspicion of these systems being the source of symptoms. In this instance, onward referral to a clinical specialist should take precedence.When diagnosed correctly, there is good support for the use of manual therapy techniques to produce a long-term reduction in symptoms. Given the prevalence of sensorimotor control disturbances associated with dysfunction to the upper cervical spine, the addition of sports-specific rehabilitation focusing on regaining this control can be clinically justified.
References
1. Pain Phys. 2015. 18: 583-595
2. Chiro & Man Th. 2011. 19-21
3. Man Th. 2005. 10: 4-13
4. JOSPT 2000. 30(12): 755-766
5. Man Th. 2008. 13: 2-11
6. Dis & Rehab. 2007. 29(15): 1193-1205
7. Man Th. 2008. 1-11
8. Arch Phys Med Rehabil. 1996. 77: 874-882
9. Manual Th. 2014. 19: 222-228
10. Phys Th. 2014. 94(4): 466-476
11. JOSPT. 2010. 40(4): 225-229




