Dislocations of the patella are uncommon injury in athletes but have serious repercussions when they do occur. In the first of a two-piece Rehab Masterclass, chiropractor Dr. Alexander Jimenez discusses the anatomy and biomechanics of the patellofemoral joint, together with recommended assessment and imaging techniques to identify damage following injury.
Dislocation of the patella is a reasonably uncommon injury in athletes, accounting for only 2-3% of knee injuries,(1,2) with an annual incidence of 5.8 per 100 000 in the general population. In the younger age group however (10-17 years), the incidence rate jumps to 29 in 100 000(3).
The largest prospective study to date has identified that ‘first-time dislocators’ tend to be female adolescents in the second decade of life(4). In children, it is the most common reason for a traumatic knee haemarthrosis(5) and in the teenage cohort, it runs second to ruptures of the anterior cruciate ligament as the major knee injury in sports(6).
The rate of re-injury has been reported as being quite varied after non-surgical conservative management (15% to 44%) (3,7,8), while the re-dislocation risk is highest amongst girls aged 10-17 years (49%) compared to first time dislocators in adult women (17%)(3).
Stability of the patellofemoral joint (PFJ) is achieved through the complex interaction of four key factors:
1. static stabilisers (patellofemoral joint geometry)
2. active (VMO)
3. passive soft tissue stabilizers (ligaments)
4. Q angle
The largest prospective study to date has identified that ‘first-time dislocators’ tend to be female adolescents in the second decade of life(4). In children, it is the most common reason for a traumatic knee haemarthrosis(5) and in the teenage cohort, it runs second to ruptures of the anterior cruciate ligament as the major knee injury in sports(6).
The rate of re-injury has been reported as being quite varied after non-surgical conservative management (15% to 44%) (3,7,8), while the re-dislocation risk is highest amongst girls aged 10-17 years (49%) compared to first time dislocators in adult women (17%)(3).
Anatomy & Biomechanics
The patella is the largest sesamoid bone in the body and is located within the quadriceps and patellar tendon. The patella increases the mechanical advantage of the quadriceps by increasing the extensor moment around the knee, and this results in greater force production in the knee extension. Furthermore, the patella centralises the divergent forces of the quadriceps muscle and transmits the tension around the femur to the patellar tendon(9).Stability of the patellofemoral joint (PFJ) is achieved through the complex interaction of four key factors:
1. static stabilisers (patellofemoral joint geometry)
2. active (VMO)
3. passive soft tissue stabilizers (ligaments)
4. Q angle
These factors all contribute (to various extents) to patellofemoral joint stability through the range of knee flexion.
Static Stabilizers
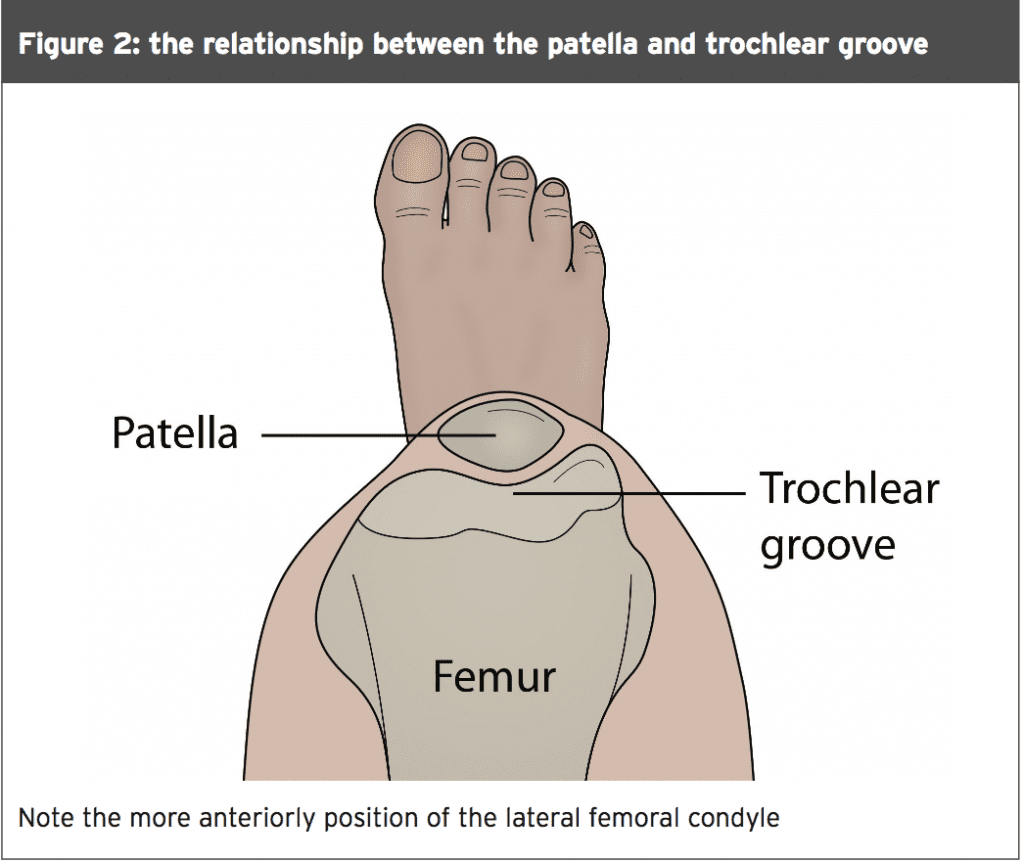
The patella has a convex articular surface and this congruity, along with the concave trochlea groove, provides some constraint to the PFJ(10,11). During knee flexion, the patella enters the confines of the trochlea at 20 degrees of knee flexion. The initial contact area of the patella is the distal and lateral patella facet.With further knee flexion, the contact area on the patella articular surface moves more proximally and the medial facet then makes contact. The patella exits the trochlear groove at around 90 degrees of knee flexion, with only the uppermost part of the patella in contact with the inferior femoral condyles (see Figure 1 below).
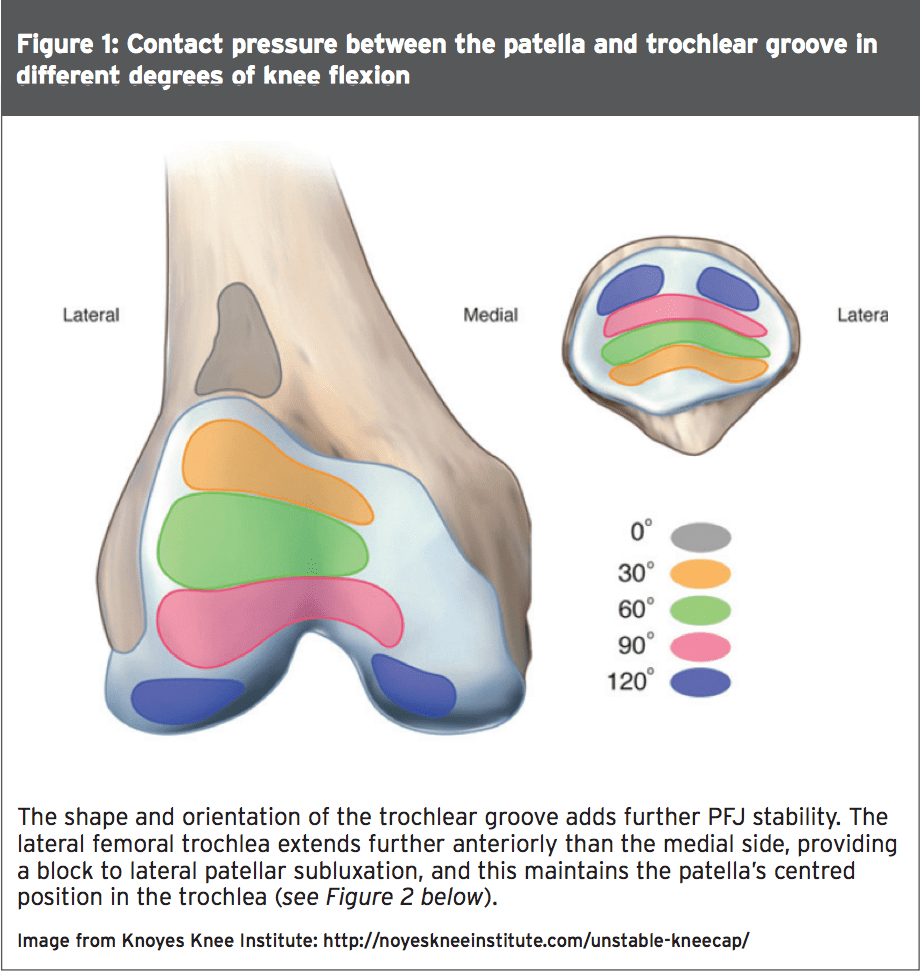
Furthermore, the lateral part of the trochlea extends further proximally than it does on the medial side, providing a mechanism for engaging the patella in early knee flexion and deflecting it medially to the centre. Several studies have identified the significance of trochlear geometry, and have demonstrated trochlear dysplasia (both decreased trochlea depth with a low lateral femoral condyle) as an important risk factor for recurrent patellar dislocation(12,13).
The height of the patella also plays a role in PFJ stability. Normal trochlear geometry is such that it encourages early ‘catchment’ of the patella during the flexion movement (usually at 20-30 degrees). With patella alta (high patella), engagement of the patella into the trochlear does not occur in the early phase of knee flexion, thus potentiating instability at the PFJ(14).
Active Stablizers
A significant amount of stability of the PFJ is provided by the quadriceps muscles. In summary, the key biomechanical factors in active PFJ stabilisation relate to the following(15):- The vastus medialis obliquus (VMO) and vastus lateralis muscle have distal portions that deviate from the parallel anatomical axis of the femur (see Figure 3).
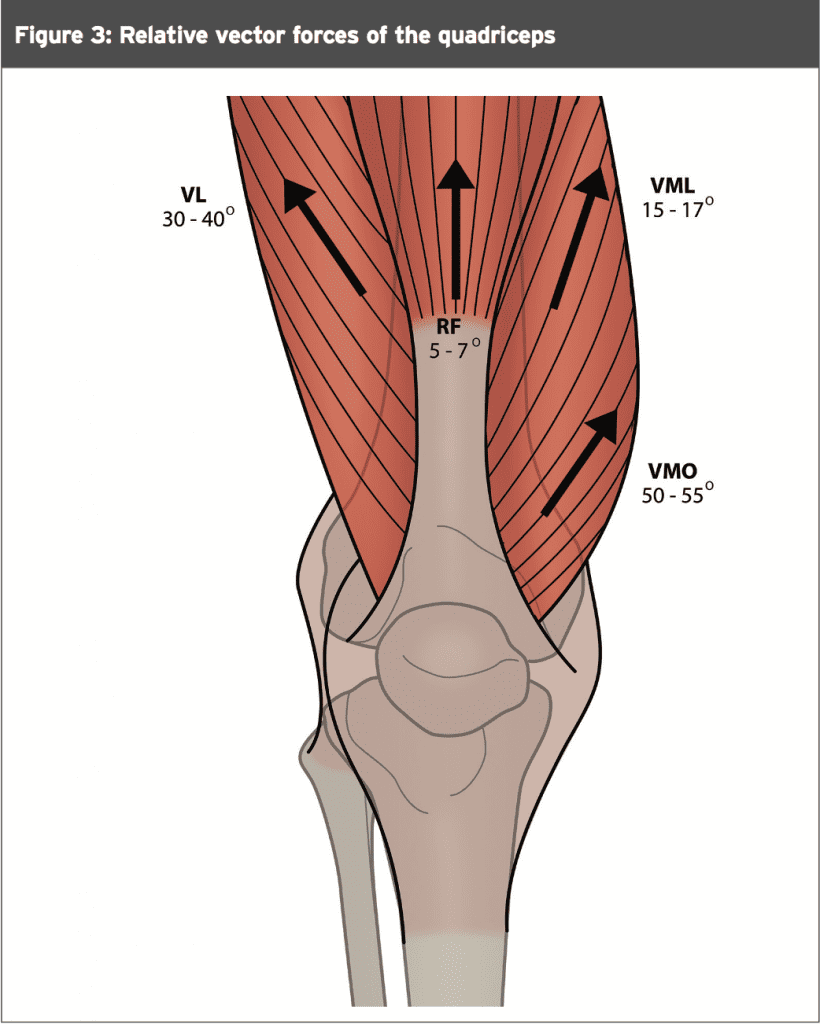
- The VMO muscle fibres have a pull of 47 ± 5 degrees from the femoral axis
- The vastus lateralis obliquus has a pull of 35 ± 4 degrees lateral from the femoral axis.
- The more obliquely aligned VMO provides a mechanical advantage to promote a medial stabilising force to the patella.
- The VMO overlies and merges with the medial patellofemoral ligament (MPFL), acting together to provide both active and passive stabilisation of the patella.
- In vitro studies have found that complete VMO relaxation reduced the patellar lateral stability significantly, especially at 20° flexion where stability was least(13,16).
- Dejour et al (1994) correlated VMO insufficiency to patellar tilt. Lateral patellar tilt (as defined by the intersection angle made from a line along the lateral slope of the trochlea groove and with a line through the widest diameter of the patellar on axial views) greater than 11° proved to be the most sensitive measure, and occurred in 93% of patients with objective patellar instability(14,17).
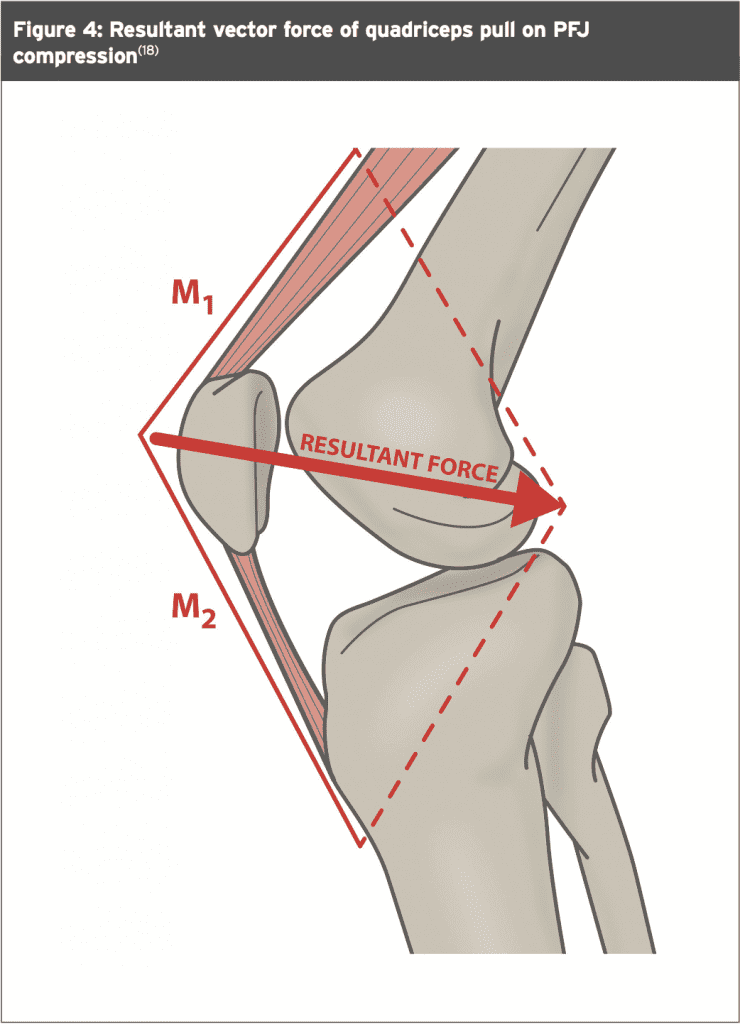
- As well as influencing the patella in a lateral-medial direction, the vastii muscles contract to also exert a posterior force vector. This force stabilises the patella within the trochlear groove during loaded knee flexion movements (such as stair
- walking and squats – see Figure 4(18)).
Passive Soft Tissue Restraints
On the medial side of the knee, three ligaments constrain lateral patella motion and contribute to PFJ stability (see Figure 5):
1. Medial patellofemoral (MPFL)
2. Patellomeniscal (MPML)
3. Patellotibial (MPTL)
The most significant of these is the MPFL, which is a continuation of the deep retinacular surface of the VMO(19). The MPFL runs transversely between the proximal half of the medial border of the patella to the femur between the medial epicondyle and the adductor tubercle, forming the second layer between the superficial medial retinaculum and the capsule. The MPFL contributes an average of 50-60 % of the total restraining force against lateral patellar displacement(20-22).
A tear to the MPFL has been considered the ‘essential lesion’ of acute patella dislocation(23). Many studies on adults have identified the relationship between acute patella dislocation and subsequent MPFL tear. It has been demonstrated that an overwhelming number (95-98%) of acute patella dislocations involve rupture of the MPFL(24-26), thus potentiating the risk of future patella dislocation. Interestingly however, this consistent correlation of acute patella dislocation to MPFL tear in adults does not seem to hold true for the pediatric and adolescent population(5,27). It remains unclear why paediatric populations have a lower incidence of MPFL tear after APD compared with adult counterparts.
Opposing this medial soft tissue force are the ligaments on the lateral side of the knee. These include:
1. The superficial layer, which is anterior and comprised of the fibrous expansion of the vastus lateralis and the superficial oblique retinaculum further posteriorly.
2. The deep layer, which mirrors the medial structures (mentioned above) and consists of the epicondylopatellar ligament, the deep transverse retinaculum and the patellotibial band. This structure attaches directly to the distal pole of the patella and sends fibres both into the lateral meniscus and into the underlying tibia(28).
3. The epicondylopatellar ligament, often referred to as the lateral patellofemoral ligament, which is not attached to the femur except indirectly via the proximal and distal attachments of the iliotibial band (ITB).
4. The distal ITB, which divides into the iliotibial tract (ITT) and the iliopatella band (IPB). The superficial oblique deep transverse layers of the lateral retinaculum attach from the IPB(29,30). It follows that tightness of the ITB (dynamic stabiliser) will influence the lateral stability force inferred by the lateral retinacular structures.
The medial and lateral retinacular structures are most effective stabilisers within the range of 20 degrees of flexion and full extension. This is where the PFJ is most vulnerable due to the lack of resistance offered by other stabilising structures(18,28).
Q Angle
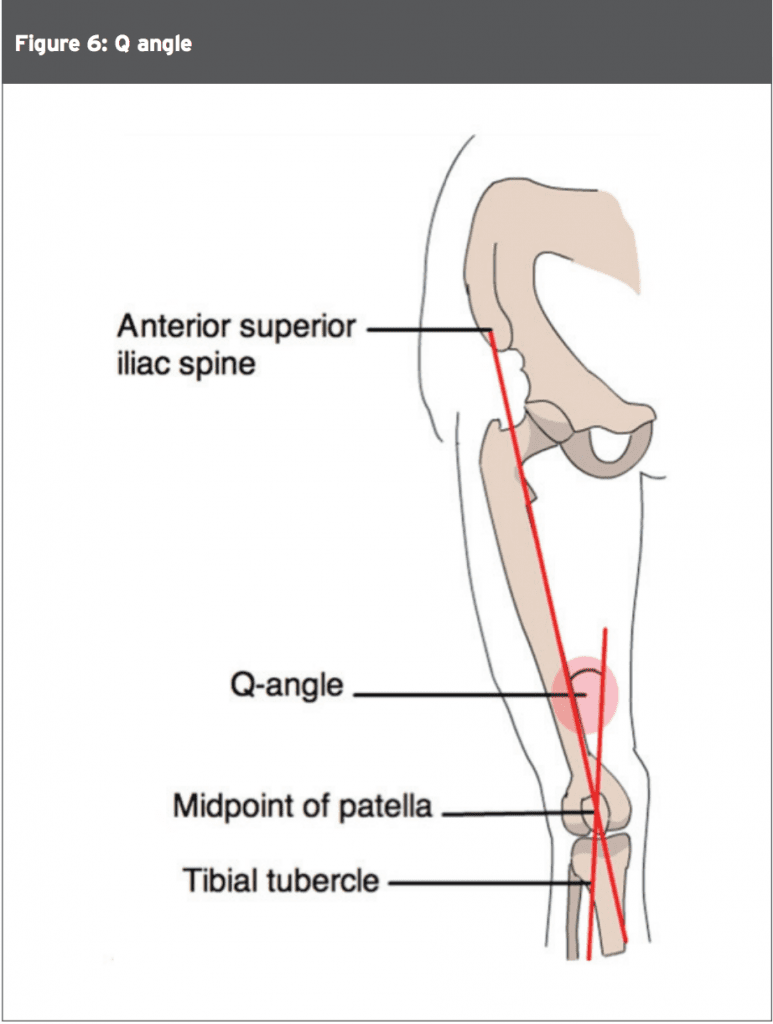
The importance of the ‘Q angle’ has been well documented(30). The Q angle is measured as the angle between the pull of the quadriceps and the axis of the patella tendon. In males, the Q angle is 8 to 10 degrees and in females it is around 15 degrees ± 5 degrees. An increase in the Q angle results in an increased valgus vector, and a potential lateral shear force may be imposed on the patella. Genu valgum, increased femoral anteversion, external tibial torsion and/or a lateralised tibial tuberosity can all ultimately affect patella tracking.
Mechanisms Of Injury
The patella is usually dislocated laterally, and subsequently it may rupture the MPFL in about 95% of the patients(24-26). Two common activities that can result in patellar dislocation are sports (61%) and dance (9%). The usual mechanism of injury is a sudden valgus force on the knee as the quadriceps are contracted, such as is encountered in cutting and pivoting type movements.As mentioned at the beginning, the rate of re-injury has been reported as being quite varied after non-surgical conservative management, being 15% to 44%(3,7,8). The risk factors for recurrent dislocation are as follows(27):
1. Patella alta (high patella)
2. Increased tibial tubersoity-trochlear groove distance
3. Trochlear dysplasia
4. Torsional abnormalities of the lower limb
As well as creating an acutely painful knee with subsequent gross haemarthrosis and joint dysfunction, other internal structures may be damaged during the dislocation episode. In a study investigating the arthroscopic examination of the articular surfaces of 39 primary patellar dislocators, a large number (95%) demonstrated an articular cartilage injury, with 23% being patellar cracks and the remaining 72% involving osteochondral or chondral fracture. Interestingly, 31% involved a cartilage injury to the lateral femoral condyle(32).
Assessment
Correctly diagnosing acute patella dislocation can be difficult as the displaced patella usually relocates spontaneously, with only 10% of patients presenting with fixed lateral dislocation(33,34). The usual findings on physical examination include:1. A large effusion, with tenderness about the medial retinaculum. This finding is not specific, so careful examination should be undertaken for ACL, PCL, collateral, and rotational laxity, as well as joint line tenderness.
2. A large, tense effusion following acute patella dislocation is likely to be a hemarthrosis. If such an effusion exists, an aspiration may be performed to relieve pain, to facilitate the examination (by reducing guarding), and to determine if a hemarthrosis exists. The presence of a hemarthrosis raises the likelihood that a significant osteochondral fracture has occurred(35).
3. Palpation of the patella may reveal a conspicuous defect at the medial patellar margin and tenderness along the course or at the insertion of the MPFL. If VMO disruption has occurred, there may be visible atrophy of this muscle.
4. The patella is often small and sits high, with evidence of hyper mobility in the lateral and medial directions(36).
5. The most reliable test for patellofemoral instability is the ‘apprehension test’. The examiner holds the relaxed knee in 30 degrees of flexion and manually subluxes the patella laterally. When the test is positive, the patient complains of pain and anxiety, resisting any further lateral motion of the patella.
Imaging (Plain Radiographs)
The first line of investigation following an acute patella dislocation is a plain X-ray. Three views are usually taken such as anteroposterior, lateral, and axial (Merchant and Laurin views). Although X-ray imaging has limitations, it is necessary to exclude osteochondral fractures, osteoarthritis of the tibiofemoral joint and loose bodies.Such a fracture visible on conventional X-rays is likely to represent a significant cartilage lesion. Even when the radiographs are normal, an osteochondral fracture may have occurred. If a hemarthrosis is present, the likelihood of a significant osteochondral fracture increases, and an MRI is indicated for further evaluation(35).
The principal radiological method of analysing the trochlear groove geometry is by means of skyline patellar views, pioneered by Merchant(37), and from this the sulcus angle can be measured. The congruence angle of Merchant is used to identify lateral translation(35), and the lateral patellofemoral angle of Lauren used to identify lateral tilt(38).
Lateral radiographs provide information relating to patella height, which can be quantified using measures such the Insall- Salvati(39), Blackburne Peel 40) and Caton Deschamps(41) indices or by using Blumensaat’s line(42). The discussion on this is beyond the scope of this article, so the reader is therefore directed to the relevant references for further information. Trochlear depth can be measured from true lateral views, with reports of 85% sensitivity for this measurement in cases of objective patellar instability(17). Trochlear dysplasia can be defined by the ‘crossing sign’ (present in 96% of cases), which is a line represented by the deepest part of the trochlear groove crossing the anterior aspect of the condyles(12, 14, 26). This is quantitatively expressed by the presence of a trochlear bump greater than 3mm (present in 66% of cases), which is indicative of trochlear dysplasia.
Imaging (MRI)
Magnetic resonance imaging (MRI) scans should be considered the gold standard investigation in acute patella dislocation. They provide not only reliable images of cartilage lesions but also associated soft tissue damage. The primary lesions that can be found on MRI include:- Chondral and osteochondral defects
- Contusions of the medial patella and lateral femoral condyle
- Knee joint effusion
- Patellar and trochlear dysplasia(43)
- Tilting of the patella and patella height(44) Avulsion fragments
- Integrity of the retinacular or patellofemoral ligamentous structures (predominantly the MPFL)(45-47)
- Sulcus angle(49)
- Dysplasia of the trochlea(14, 50) (increased trochlear dysplasia is described as a risk factor for patellar instability(24), and the shape of the trochlear groove and degree of trochlea dysplasia are considered similar in pediatrics and adults(2)
- Depth and facet asymmetry of the trochlea(44, 51)
- The Insall-Salvati index(39, 52)
- Tibial tuberosity-trochlear groove distance(53)
Imaging (CT Scans)
Computed tomography (CT) can provide a three-dimensional view of the PFJ. Images can be created at different angles of knee flexion, as well as performing dynamic investigation. Studies have reported CT scans to be accurate and sensitive in detecting abnormal tracking, tilt and subluxation(54, 55). Their main advantage lies in the assessment of lower limb alignment, femoral anteversion, and lateralisation of the tibial tubercle (tibial tubercle to trochlear groove offset). A tibial tuberosity offset greater than 9 mm has been shown to identify patients with patellofemoral malalignment with a specificity of 95 % and a sensitivity of 85%(56). A tibial tubercle-to-trochlear groove distance of greater than 20mm is virtually always associated with patella instability.Conclusion
Acute patella dislocation is an uncommon traumatic injury in the athlete, mostly occuring in the younger teenage athlete. Associated lesions such as cartilage defects and MPFL rupture may be the end result of this injury and these will need to be identified on a radiological work up including X-ray, CT scanning and MRI. Part two of this series in the next issue will discuss the efficacy of repair in first time dislocators, and the host of possible surgeries available to repair the dislocated patella. It will also outline the post- operative rehabilitation required to restore the athlete to full knee function.References
1. Clinical Sports Med. 2003. 21(3); 499-519
2. Eur J Radiol. 2011;79(3):415–20
3. Am J Sports Med. 2004; 32:1114-1121
4. Am J Sports Med. 2000; 28:472-479
5. Pediatr Radiol. 2006; 36:1163-1170
6. J Pediatr Orthop. 2012;32(8):760–4
7. J Trauma. 1977; 17:526-531
8. Am J Sports Med. 1986; 14:117-120
9. Curr Orthop. 2008; 22(2):132–138
10. J Orthop Sports Phys Therapy. 1998;
28:286–29
11. Knee Surg Sports Traumatol Arthroscopy.
2006; 14:235–240
12. Rev Chir Orthop Reparatrice Appar Mot.
1990; 76:45-54
13. J Orthop Research. 2003; 21:780–786
14. Knee Surg Sports Traumatol Arthrosc.
1994;2(1):19–26.32
15. J Orthop Res. 1998; 16:136–14
16. J Bone J Surg. 2005; 87:577–582
17. Knee Surg Sports Traumatol Arthroscopy.
2006; 14(3):264–27
18. Fulkerson JP (2004). Disorders of the
Patellofemoral Joint. Lippincott Williams & Wilkins
19. Orthopedics. 2008 Apr;31(4):306, 407-408
20. Am J Sports Med. 1998; 26:59–65
21. Clin Orthop. 1998; 349:174–182
22. J Bone J Surg Br. 2005; 87:36–
23. Knee. 2003; 10:215-220
24. Arthroscopy. 2010;26:926-935
25. J Bone Joint Surg Am. 2009; 91:263-273
26. Knee. 2011;18:185-188
27. Am J Sports Med. 2004; 32(6):1509–1513
28. Clin Orthop . 1980; 153:183–188
29. Am J of Sports Med; 1986. 14; 39-45
30. Arthroscopy. 2007; 23. 269-274
31. Acta Orthop Scand. 1964; 68 (suppl 68):1–14
32. Arthroscopy. 2003; 19:717-721
33. J Am Acad Orthop Surg. 1997; 5: 47-57
34. Orthop Clin North Am. 2003; 34:385-396
35. Sports Health. 2011; 3(2). 170-174
36. Sports Med Arthrosc Rev. 2007; 15:95–104
37. J Bone J Surg Am. 1974; 56:1391–1396
38. J Bone J Surg Am. 1978; 60:55–6
39. Radiology. 1971; 101:101–104
40. J Bone J Surg Br. 1977: 59(2):241–242
41. Rev Chir Orthop Reparatrice Appar Mot.
1982; 68(5):317–325
42. Ergebnisse der Chirurgie und Orthop. 1938;
228 (31):149–22
43. Turk J Med Sci. 2004;34:165-169
44. Acta Orthop. 2005;76(5):693–8.39
45. J Bone J Surg Br. 2007; 89:709–716
46. AJR Am J Roentgenol. 1997;168(1):117–22.29
47. Knee Surg Sports Traumatol Arthrosc.
2012;20:1575-1580
48. Knee Surg Sports Traumatol Arthrosc.
2013;21(3):683–9.14
49. J Bone J Surg Br. 2006; 88:688–69
50. Int Orthop. 2010; 34(2):311–316
51. Radiology. 2000;216(3):858–64
52. AJR Am J Roentgenol. 1996;167:339-341
53. Knee. 2006;13:26-31
54. Arthroscopy. 1992; 8:327–334
55. Can J Surg. 1994; 37(4):319–323
56. Skeletal Radiology. 1995; 24(7); 505-509




