In the first of this 2-part series, chiropractor Dr. Alexander Jimenez brings insight into the anatomy and biomechanics of the biceps brachii muscle, the mechanisms of injury, and the typical signs and symptoms that may alert a clinician to a biceps tendon rupture.
Athletes in contact and strength-based sports place an enormous amount of stress onto the distal bicep tendon. However injuries to the distal biceps tendon are not common in athletes, accounting for 10% of all bicep tendon ruptures, with the long head of the proximal insertion rupturing most frequently(1). If an injury to the distal bicep tendon does occur, it usually in the dominant arm of middle aged men (40-60yrs), suggesting a degree of degeneration must be present to rupture(1).
There have been a growing number of case reports in the media about these injuries – in particular athletes such as powerlifters and bodybuilders with a history of anabolic steroid use. More recent studies have shown that the incidence of this injury is increasing and the age group that sufferers is getting younger(1,2). It is believed that full tendon ruptures will require surgery to restore the biceps role as an elbow flexor and supinator of the forearm to prevent loss of strength in these movements(3).
There have been a growing number of case reports in the media about these injuries – in particular athletes such as powerlifters and bodybuilders with a history of anabolic steroid use. More recent studies have shown that the incidence of this injury is increasing and the age group that sufferers is getting younger(1,2). It is believed that full tendon ruptures will require surgery to restore the biceps role as an elbow flexor and supinator of the forearm to prevent loss of strength in these movements(3).
Anatomy & Biomechanics
The long head of the bicep originates from the supraglenoid tubercle of the scapula, and the short head arises from the coracoid process. It is common for the muscle to course distally as two separate heads or bellies, with the fibres from the short head on the ulnar side of the arm and the long head on the radial side. However, the two bellies may interdigitate closer to the elbow(4,5).
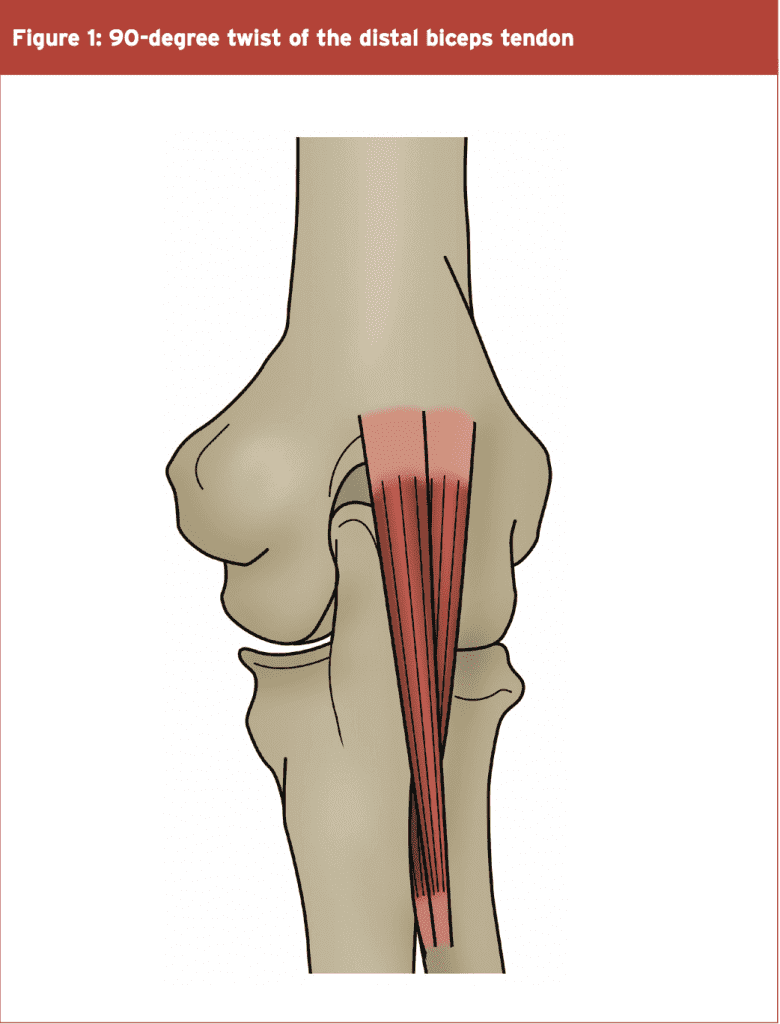
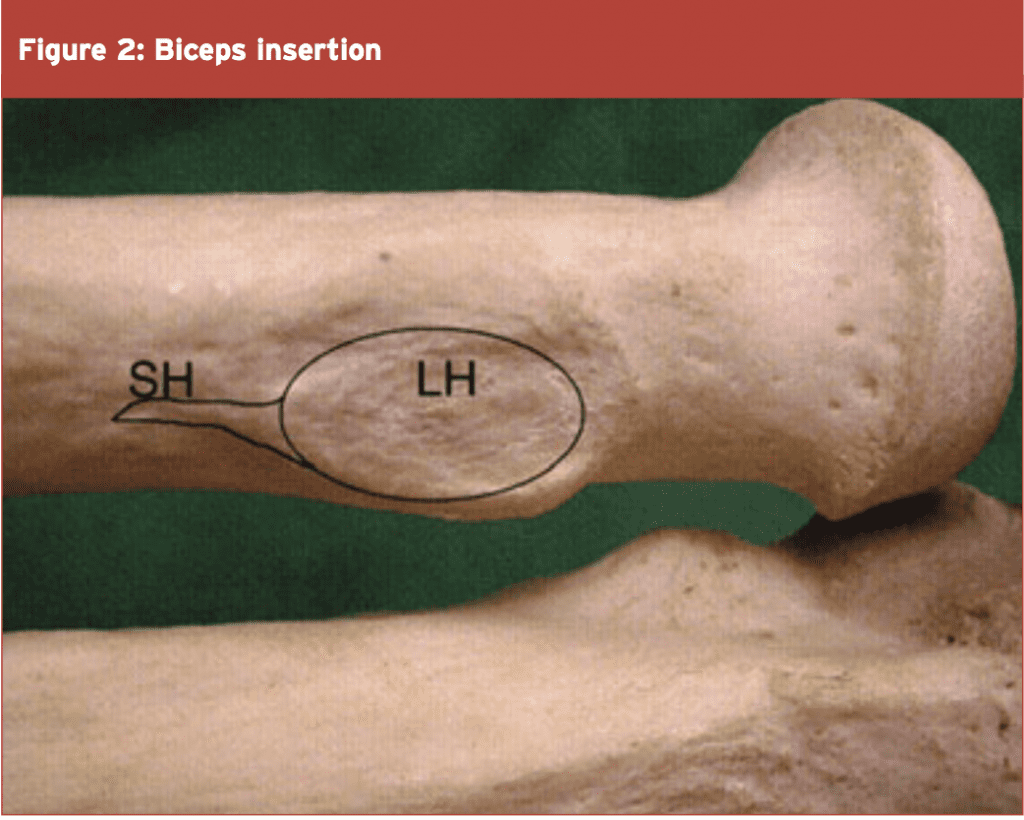
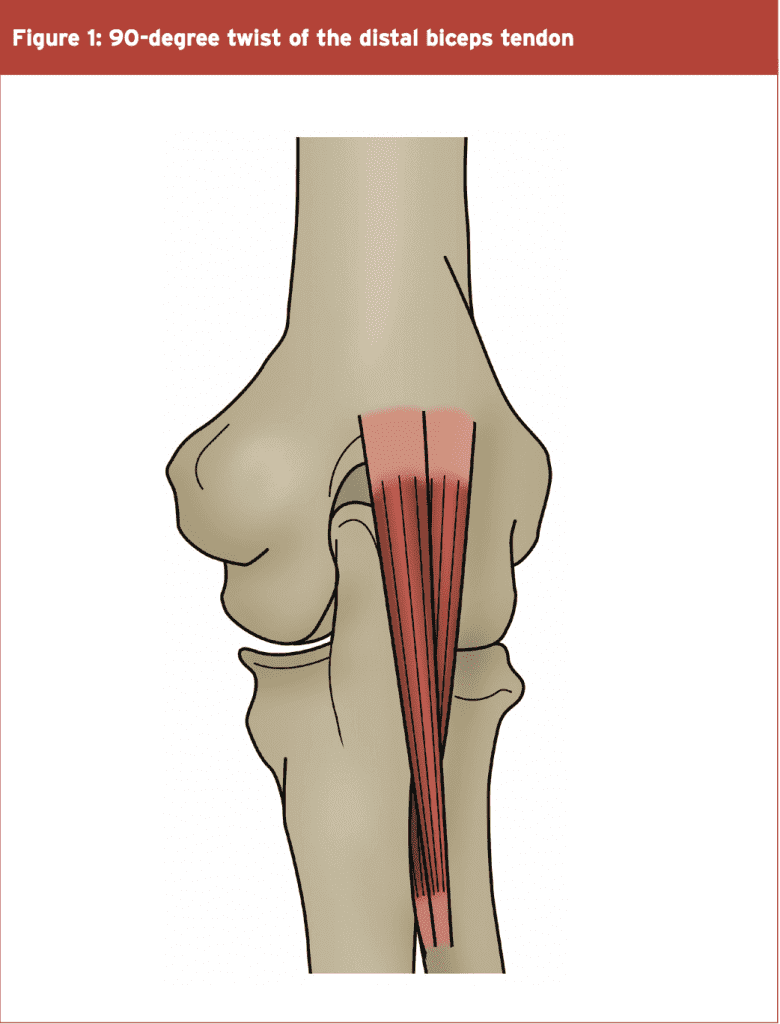
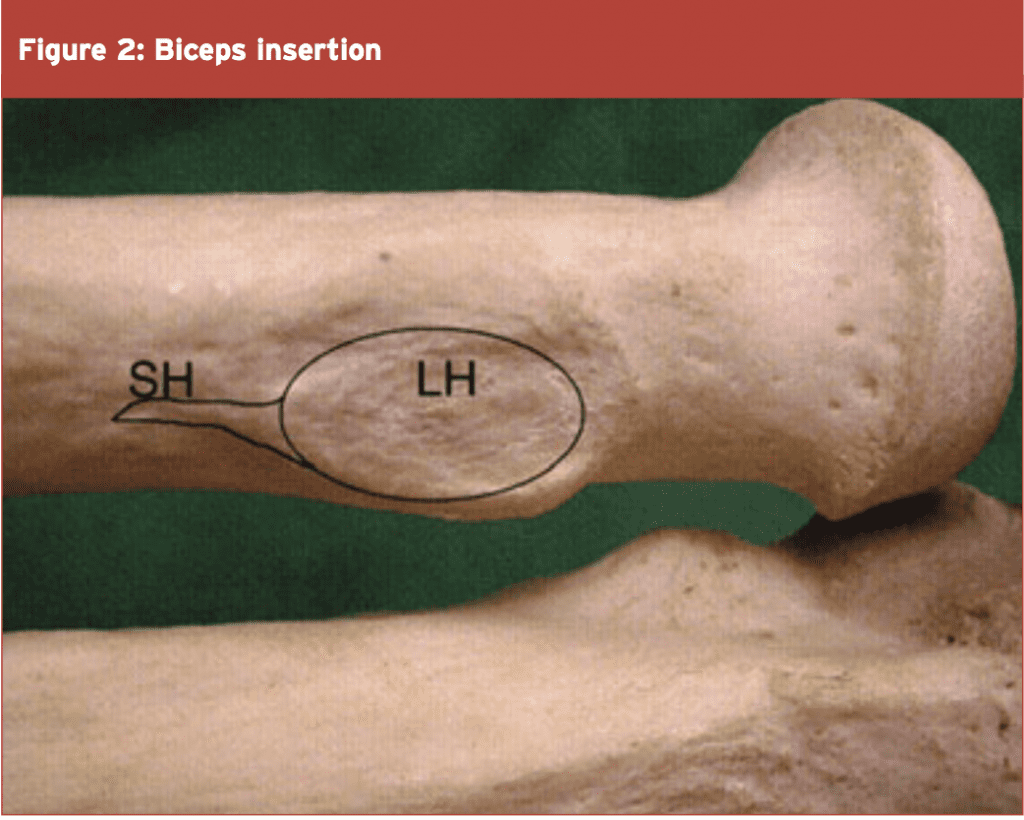
As the tendons course to the radial insertion, they twist counter clockwise in right arms, with the anteromedial fibres from the short head inserting inferiorly on the radial tuberosity, with the posterolateral long head inserting more superior on the tuberosity (see Figures 1 and 2)(5,6). It is suggested that this twisting arrangement differentiates the short head as primarily being an elbow flexor and the long head as a supinator(5).
The aponeurosis of the biceps (also called the lacertus fibosus – see Figure 3) originates at the level of the musculotendinous junction and attaches to the superficial fascia of the ulnar in three distinct layers, which envelope the forearm flexor muscles(5). It has been suggested that as the forearm flexors contract, they tense the aponeurosis and create a medial pull on the bicep tendon, possibly contributing to its rupture. An intact bicipital aponeurosis at the time of tendon rupture makes surgical repair much easier.

The common distal bicep tendon inserts onto the biceps tuberosity, which is around 25mm from the radial head(7). The ridge of bone that forms the tuberosity is usually a single ridge and is 22-24mm long and 12-15mm wide. It attaches into the most ulnar side of the tuberosity(8,9). The primary function of the biceps muscle is to supinate the forearm. Its action as an elbow flexor is secondary as the brachioradialis and brachilias can also perform elbow flexion.
The mechanical-stress theory relates to the compressive effect of the radius and ulnar on the distal biceps tendon in positions of supination and pronation. With the arm fully pronated, the space for the distal tendon between the lateral border of the ulnar and the radial tuberosity corresponds to the space available for the tendon. In full supination the space is 52% greater. It is suggested therefore that repeated and forced pronation may continually compress the tendon(10).
If surgical treatment of a complete distal biceps tendon rupture is delayed, a combination of muscle retraction, adhesion formation, distal tendon shortening, and degeneration can make anatomic reinsertion of the original tendon difficult(2,19,22). Outcome comparisons of acute and chronic repairs suggest a surgical delay greater than 10 days post-injury increases the risk of complications and the extent of anterior dissection required(23,24).
A host of studies have compared the relative success of 1-incision repairs and 2-incision repairs for regaining both elbow flexion strength and supination strength in post-operative complications such as nerve palsies and heterotrophic ossification. Overall, on the balance of evidence, it seems that with regards to functional outcomes and post-operative complications, the 1 and 2-incision repairs are equally successful(18,24-27,35-43).
References
1. Clin Orthop Relat Res. 2002;404:275-83
2. J Am Acad Orthop Surg. 1999;7:199–207
3. J Shoulder Elbow Surg. 2010;19:184–9
4. J Hand Surg. 2007;32-A: 1225–9
5. J Bone Jt Surg. 2007;89-A:1044–9
6. Clin Orthop. 2006;456:117–20
7. J Bone Joint Surg Am. 2010;92:2128-38
8. J Shoulder Elbow Surg. 2007;16:122–7
9. J Shoulder Elbow Surg. 2008;17:342–6
10. J Shoulder Elbow Surg. 1995;4:149-56
11. Bone Joint Surg 1989;71: 100–101
12. J Shoulder Elbow Surg. 2006;15:614–9
13. Clin Orthop Relat Res. 2005;437:128–31
14. Am J Sports Med. 2007;35:1865–69
15. J Bone Jt Surg. 1956;38:1365–8
16. Am J Surg. 1960;99:636–40
17. AJR. 2004;182:944–6
18. J Bone Jt Surg. 1985;67-A:414–7
19. J Bone Jt Surg. 1985;67-A:418–21
20. Injury. 2008;39:753–60
21. J Bone Jt Surg. 2009;91-A:2329–34
22. J Shoulder Elbow Surg. 2006;15:440–4
23. J Bone Joint Surg. 2000;82-A:1575–81
24. J Shoulder Elbow Surg. 2000;9:227–33
25. J Hand Surg. 2004;29-B:178–82
26. J Hand Surg. 2003;28-A: 496–502
27. J Shoulder Elbow Surg. 2003;12:484–90
28. Am J Sports Med. 2009;37:506–11
29. Am J Sports Med. 2009;37:989–94
30. Am J Sports Med. 2006;34:968–74
31. Am J Sports Med. 1999;27:128–32
32. J Shoulder Elbow Surg. 2003;12:607–11
33. Injury. 2006; 37:838-42
34. J Bone Joint Surg Am. 1961;43:1041-3
35. Am J Sports Med. 1993;21:114-9
36. Clin Orthop Relat Res. 1996;333:186-91
37. Clin Orthop Relat Res. 1999;363:100-7
38. Am J Sports Med. 2008;36:1618-24
39. Clin Orthop Relat Res. 1996;322:116-9
40. J Shoulder Elbow Surg. 2005;14:302–6
41. J Shoulder Elbow Surg. 2007; 16:78-83
42. Arthroscopy. 2008;24:39-45
43. J Shoulder Elbow Surg. 2000;9:120-6
44. J Shoulder Elbow Surg. 2009;18:283–7
45. Am J Sports Med. 1998;26:428-32
46. Am J Sports Med. 2002;30:432-6
47. Am J Sports Med. 2004;32:406-10
48. J Bone Jt Surg. 2008;90-B:103–6
49. Am J Sports Med. 2007;35:252–8
50. J Shoulder Elbow Surg. 2004;13:648–51
51. Clin Orthop Relat Res. 1996;323:188–91
52. Am J Sports Med. 2000;28:538–40
53. J Bone Joint Surg. 2002;84-A:999–1005
54. J Hand Surg. 2009;34-A:545–52
55. Br J Sports Med. 1999;33:281–3
56. Acta Orthop Scan. 1977;48:280–2
57. Clin Orthop Relat Res. 2008;466: 2475–81

The common distal bicep tendon inserts onto the biceps tuberosity, which is around 25mm from the radial head(7). The ridge of bone that forms the tuberosity is usually a single ridge and is 22-24mm long and 12-15mm wide. It attaches into the most ulnar side of the tuberosity(8,9). The primary function of the biceps muscle is to supinate the forearm. Its action as an elbow flexor is secondary as the brachioradialis and brachilias can also perform elbow flexion.
Mechanism Of Injury
The most common mechanism of injury is a sudden elbow extension force applied whilst the elbow is flexed. This eccentric force produces a tensile stress that can suddenly rupture the distal tendon. Added to this may be the added compression of the tendon found in pronation(10) and with the forearm flexors contracted, which may tense the aponeurosis and displace the tendon medially(5), thus producing a torsional force to the tendon. It is a rare injury (1.2 ruptures per 100,000 patients per year) and the typical sufferer age is a male in his late 40s. The dominant arm is involved 86% of the time, and smokers have 7.5 times greater risk of injury(1).Pathogenesis
The two current theories for the pathogenesis of distal biceps tendon ruptures are hypovascularity in the tendon and mechanical stress. It has been found in cadaver studies that a consistent zone of hypovascularity and degeneration is found in an approximate 2.14cm diameter of the tendon(10), similar to the hypovascular zone seen in ruptured Achilles tendons that rupture(11). A lack of blood supply may also lead to poor healing capacity and tendency towards degeneration.The mechanical-stress theory relates to the compressive effect of the radius and ulnar on the distal biceps tendon in positions of supination and pronation. With the arm fully pronated, the space for the distal tendon between the lateral border of the ulnar and the radial tuberosity corresponds to the space available for the tendon. In full supination the space is 52% greater. It is suggested therefore that repeated and forced pronation may continually compress the tendon(10).
Signs & Symptoms
Patients with a distal biceps tendon injury typically experience a tearing sensation or ‘twanging’ and an acute onset of pain after an unexpected or massive extension force has been applied to the flexed elbow. Typically, there is pain and deformity with weakness of supination. Gross swelling may develop over the cubital fossa in the hours following. If the biceps aponeurosis remains intact, the rupture may be clinically missed(7,12). Two tests have been proposed to assess for a ruptured bicep tendon:
1. Biceps squeeze test – With patient sitting and arm bent to 60-80 degrees, squeeze the bicep with both hands. If the forearm does not supinate this is indicative of a full bicep tendon rupture(13). This test has been found to be 96% sensitive to tendon rupture.
2. Hook test – With patient sitting and elbow bent to 90 degrees and fully supinated, the examiner uses their fingers to hook the tendon from the lateral side. If the tendon is intact, the tendon is easily ‘hooked’. In a ruptured tendon there is no palpable tendon structure(14). This test is reported to have 100% sensitivity and specificity, and is better than MRI for assessing tendon rupture.

2. Hook test – With patient sitting and elbow bent to 90 degrees and fully supinated, the examiner uses their fingers to hook the tendon from the lateral side. If the tendon is intact, the tendon is easily ‘hooked’. In a ruptured tendon there is no palpable tendon structure(14). This test is reported to have 100% sensitivity and specificity, and is better than MRI for assessing tendon rupture.

Imaging
Imaging is usually quite limited for an effective diagnosis of a complete rupture. Often, performing the hook test and squeeze test should be enough to confirm a full rupture. However, radiograph X-rays can be useful to visualise enlargement or irregularity at the radial tuberosity(15) or an avulsion of the radial tuberosity(16). MRI can be useful to visualise the integrity of the tendon and any intrasubstance degeneration. The best position to MRI the tendon is in the FABS position. The arm is held with 90 degrees elbow flexion, 180 degrees of shoulder abduction and supination of the forearm(17).Management Of Biceps Tendon Ruptures
It is generally accepted that operative repair leads to better functional outcomes versus non-operative repairs. To summarise some of the leading studies on non-operative versus operative management:- Operative repair leads to better supination strength and elbow flexion strength and endurance(18,19).
- An untreated biceps tendon rupture can result in 40% loss of supination power, with 30% loss in elbow flexion strength(3).
- There are better subjective outcomes and objective isokinetic testing following operative repairs(20).
- Retrospective studies of non-operative versus operative repair show that at 5 years post injury, supination strength was only 74% to that of operated tendons. Flexion strength was 88% compared to repaired tendons(21). The difference was even more pronounced if the dominant arm was injured.
If surgical treatment of a complete distal biceps tendon rupture is delayed, a combination of muscle retraction, adhesion formation, distal tendon shortening, and degeneration can make anatomic reinsertion of the original tendon difficult(2,19,22). Outcome comparisons of acute and chronic repairs suggest a surgical delay greater than 10 days post-injury increases the risk of complications and the extent of anterior dissection required(23,24).
Surgical Treatment
The literature describes anatomic versus non-anatomic repairs, single incision repairs and two incision repairs using bone anchors, suture tunnels, suture anchors, cortical buttons and interference screws to attach the distal tendon to the radial tuberosity(24-30).
Number Of Incisions
It was initially believed that the use of two incisions reduces the post-operative complications such as nerve damage, heterotrophic ossification, loss of forearm pronation and wound infection(34). In view of the difficulty and complications of a direct anterior approach such as a radial nerve palsy, Boyd and Anderson described a dual-incision technique where the tendon is retrieved anteriorly and passed through the forearm bones to be reattached through a posterior approach to the radial tuberosity, exposed by pronation of the forearm(34).A host of studies have compared the relative success of 1-incision repairs and 2-incision repairs for regaining both elbow flexion strength and supination strength in post-operative complications such as nerve palsies and heterotrophic ossification. Overall, on the balance of evidence, it seems that with regards to functional outcomes and post-operative complications, the 1 and 2-incision repairs are equally successful(18,24-27,35-43).
Fixation & Grafting
Numerous studies have looked at the relative benefits of the different fixation methods such suture anchors, trans- osseous tunnels, cortical button repairs, interface screw fixation(27,29,30,44-49). The consensus is that cortical button fixation methods are superior to suture anchors, sutures in bone tunnels and interface screws(27,38,48,49). As for tendon grafting, this technique is usually reserved in cases whereby the biceps tendon repair has been delayed, and the tendon has retracted a distance making direct repair very difficult. Due to the retraction, there is a need to restore tendon length to actually achieve a fixation onto the radial tuberosity. Typical grafts used are semitendinosis (22,50,51), flexor carpi radialis(52), Achilles tendon(12,52,53), tensor fascia lata (55,56), and palmaris longus, plantaris and long toe extensors autografts(57).Conclusion
Distal biceps tendon ruptures are reasonably uncommon injuries in athletes. However, if they do occur then early surgical treatment is almost always necessary to restore the biceps attachment so the athlete does not lose strength and endurance in elbow flexion and forearm supination. Multiple surgical techniques exist all with their own strengths and weaknesses. In part two this Rehab Masterclass article, we will look in detail at the most effective rehabilitation protocols following surgical repair of the distal biceps tendon.References
1. Clin Orthop Relat Res. 2002;404:275-83
2. J Am Acad Orthop Surg. 1999;7:199–207
3. J Shoulder Elbow Surg. 2010;19:184–9
4. J Hand Surg. 2007;32-A: 1225–9
5. J Bone Jt Surg. 2007;89-A:1044–9
6. Clin Orthop. 2006;456:117–20
7. J Bone Joint Surg Am. 2010;92:2128-38
8. J Shoulder Elbow Surg. 2007;16:122–7
9. J Shoulder Elbow Surg. 2008;17:342–6
10. J Shoulder Elbow Surg. 1995;4:149-56
11. Bone Joint Surg 1989;71: 100–101
12. J Shoulder Elbow Surg. 2006;15:614–9
13. Clin Orthop Relat Res. 2005;437:128–31
14. Am J Sports Med. 2007;35:1865–69
15. J Bone Jt Surg. 1956;38:1365–8
16. Am J Surg. 1960;99:636–40
17. AJR. 2004;182:944–6
18. J Bone Jt Surg. 1985;67-A:414–7
19. J Bone Jt Surg. 1985;67-A:418–21
20. Injury. 2008;39:753–60
21. J Bone Jt Surg. 2009;91-A:2329–34
22. J Shoulder Elbow Surg. 2006;15:440–4
23. J Bone Joint Surg. 2000;82-A:1575–81
24. J Shoulder Elbow Surg. 2000;9:227–33
25. J Hand Surg. 2004;29-B:178–82
26. J Hand Surg. 2003;28-A: 496–502
27. J Shoulder Elbow Surg. 2003;12:484–90
28. Am J Sports Med. 2009;37:506–11
29. Am J Sports Med. 2009;37:989–94
30. Am J Sports Med. 2006;34:968–74
31. Am J Sports Med. 1999;27:128–32
32. J Shoulder Elbow Surg. 2003;12:607–11
33. Injury. 2006; 37:838-42
34. J Bone Joint Surg Am. 1961;43:1041-3
35. Am J Sports Med. 1993;21:114-9
36. Clin Orthop Relat Res. 1996;333:186-91
37. Clin Orthop Relat Res. 1999;363:100-7
38. Am J Sports Med. 2008;36:1618-24
39. Clin Orthop Relat Res. 1996;322:116-9
40. J Shoulder Elbow Surg. 2005;14:302–6
41. J Shoulder Elbow Surg. 2007; 16:78-83
42. Arthroscopy. 2008;24:39-45
43. J Shoulder Elbow Surg. 2000;9:120-6
44. J Shoulder Elbow Surg. 2009;18:283–7
45. Am J Sports Med. 1998;26:428-32
46. Am J Sports Med. 2002;30:432-6
47. Am J Sports Med. 2004;32:406-10
48. J Bone Jt Surg. 2008;90-B:103–6
49. Am J Sports Med. 2007;35:252–8
50. J Shoulder Elbow Surg. 2004;13:648–51
51. Clin Orthop Relat Res. 1996;323:188–91
52. Am J Sports Med. 2000;28:538–40
53. J Bone Joint Surg. 2002;84-A:999–1005
54. J Hand Surg. 2009;34-A:545–52
55. Br J Sports Med. 1999;33:281–3
56. Acta Orthop Scan. 1977;48:280–2
57. Clin Orthop Relat Res. 2008;466: 2475–81




