In part I, chiropractor, Dr. Alexander Jimenez brought insight into the relevant anatomy and functional biomechanics of the distal biceps unit, the mechanisms of injury and clinical tests commonly used to diagnose distal bicep tendon ruptures. In part two, Dr. Jimenez outlines and explores the post-surgical rehabilitation of distal bicep tendon repairs…
The recent trend in postoperative rehabilitation of acute distal biceps tendon repairs has been towards pushing for early range of movement, as the risk of tendon retraction and postoperative complications is less(1,2). However, in chronic repairs, the exact protocol will depend on the quality of the tendon at the time of surgery, and if tendon grafting is needed. Often these chronic rupture repairs need a period of immobilization in a brace in flexion and neutral rotation from 2 weeks to 6 weeks(3-9).
The brace may initially start at 90 degrees flexion and be gradually opened over the 6-week post-operative period so that by week six, the patient can extend to 30 degrees elbow flexion. After the 6-week post-operative period the elbow is gradually stretched into full elbow extension and full pronation. Formal strength retraining is usually started at 2-3 months post-operative but return to sport and heavy lifting is delayed to 6 months following surgery.
The discussion below focuses on the rehabilitation schedule following an acutely repaired distal bicep tendon, and doesn’t discuss the complications of delayed repairs. It is assumed that in a professional and elite sport setting, the risk of ‘missing’ a rupture of the distal biceps tendon would not be as apparent as it may be in general practice. Elite athletes have access to a host of sports medicine practitioners who can push for diagnostics and imaging quite quickly. Therefore, the risk of missing a tendon rupture and subsequent delayed surgery would not be as prevalent as in the non-athletic population. These athletes are more likely to undergo acute repairs of the distal biceps tendon, thus negating the complications associated with delayed repairs.
Stages In The Post-Operative Schedule
As with any sports-related post-operative surgical procedure, the time to return to sport and competition is influenced not only by the healing capacities of the surgically repaired tissues (which usually follow predictable timelines) but also by the functional progressions of the athlete. As has been the theme with many of the discussions in the SIB Rehabilitation series, a list of ‘exit criteria’ has again been presented to help guide the sports therapist in progressing from one stage to the next. A common post-operative schedule in an acutely ruptured tendon is described below.Phase 1: Protection & Healing
(first 3 weeks post-operative)As with the majority of post-surgical rehabilitation programs, the first few weeks after the operation are crucial to allow a healthy healing environment to be created. This allows timely and optimal healing of the repaired tissues. Therefore, care and consideration must be taken to avoid large tensile forces on the bicep tendon through either passive over-stretching or strong muscle contraction. In the non-elite athlete, this may involve protected home stay for the first 3 weeks. However, in the elite strength athlete, measures must be taken to avoid a huge loss of range of motion at the elbow and the development of gross muscle atrophy in the biceps/triceps and forearm muscles. Therefore, the common approaches used are as follows:
- Some surgeons may brace the elbow immobile in a posterior elbow splint for the first week. Others may choose to apply a removable elbow splint, which is fixed to 90 degrees elbow flexion (the splint can be removed for washing and for exercises).
- A collar and cuff is used to support the arm during walking and standing.
- The elbow may be passively flexed and extended from 30 degrees to 130 degrees. This needs to be done in a controlled, slow fashion by the physiotherapist or athletic trainer – 20-25 repetitions, five times per day.
- Icing of the elbow crease is undertaken post exercise.
- Active shoulder abduction, flexion and external rotation may be performed with the elbow brace on – 2-3 sets of 10-15 reps is sufficient.
- Seated scapular retraction exercises are performed with the brace on and elbows supported on a pillow.
- Active wrist and finger flexion/ extension exercises are performed.
- Muscle stimulation using the atrophy mode for the bicep and triceps, and hypertrophy mode on the deltoids may be used at this stage.
- Cardio work would be limited to recumbent cycle or 1 arm rowing on a rowing ergometer.
1. Pain-free passive elbow flexion from 30-130 degrees flexion.
2. Minimal swelling and no wound complications.
3. Normal skin sensation over forearm indicating no nerve damage intra- operatively.
4. Full passive forearm supination and pronation at 30 degrees elbow flexion.
Phase 2: Passive Range Of Movement (Weeks 3-6)
- From week 3, the brace is opened 10 degrees each week. In week six, the patient has full range of movement with the brace in situ. (This will differ with the delayed tendon repairs where they are protected over the first 6 weeks.)
- Active extension in the brace is allowed, but flexion is still passive and in the brace.
- Scar tissue massage to prevent adhesions at operative site is recommended. This can be done regularly throughout the day.
- Patients should continue with active wrist/shoulder exercises.
- Scapular retraction/depression exercises can be started in prone – if the position is tolerated.
- Patients should start light Theraband shoulder internal and external rotation exercises, with the brace on and locked at 90 degrees (from week five).
- Weighted wrist extension and flexion exercises, and ulnar/radial deviations can be performed with a weighted stick.
- Continued use of muscle stimulator to the bicep, tricep and deltoids is recommended.
Exit criteria for Phase 2 (weeks 3-6)
1. Full passive range of motion in flexion. Full active extension.
2. No swelling or inflammation at operative site.
3. Full active pronation in all positions. Full passive supination in all positions.
Phase 3: Early Strength Phase (Weeks 6-12)
1. Early active biceps muscle contraction.
This can be done as the following progression;
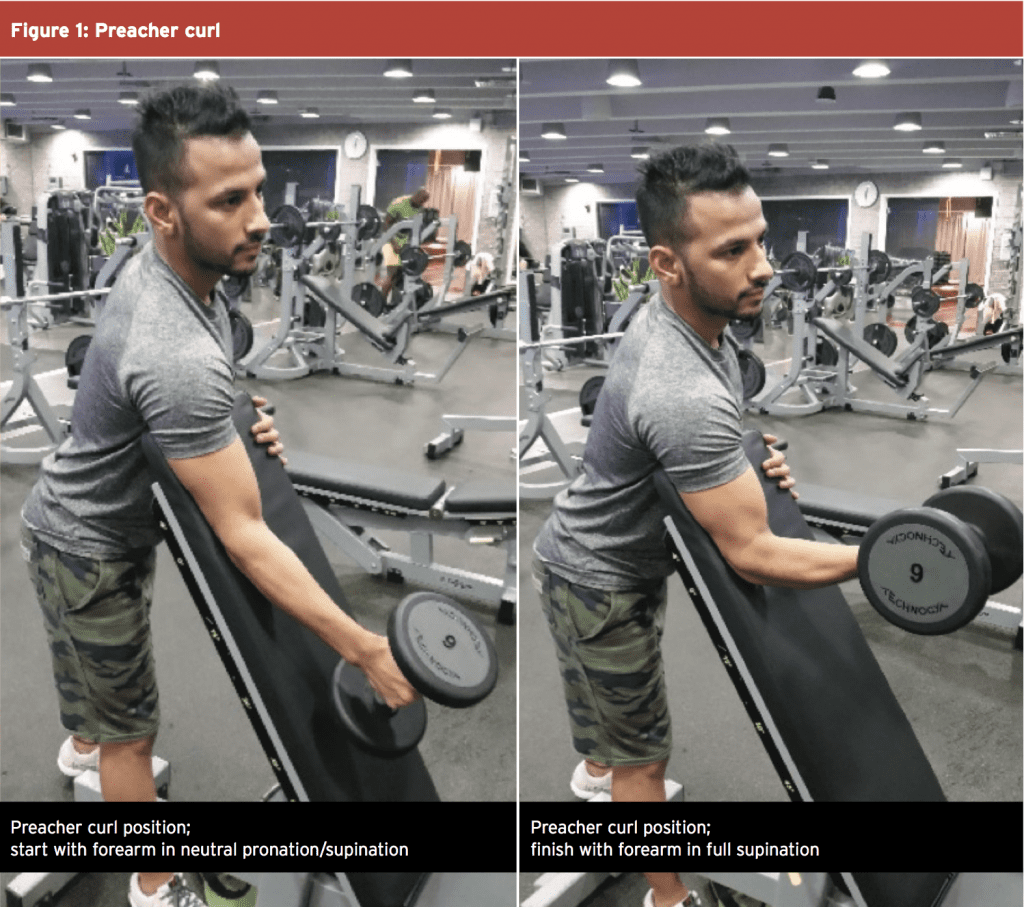
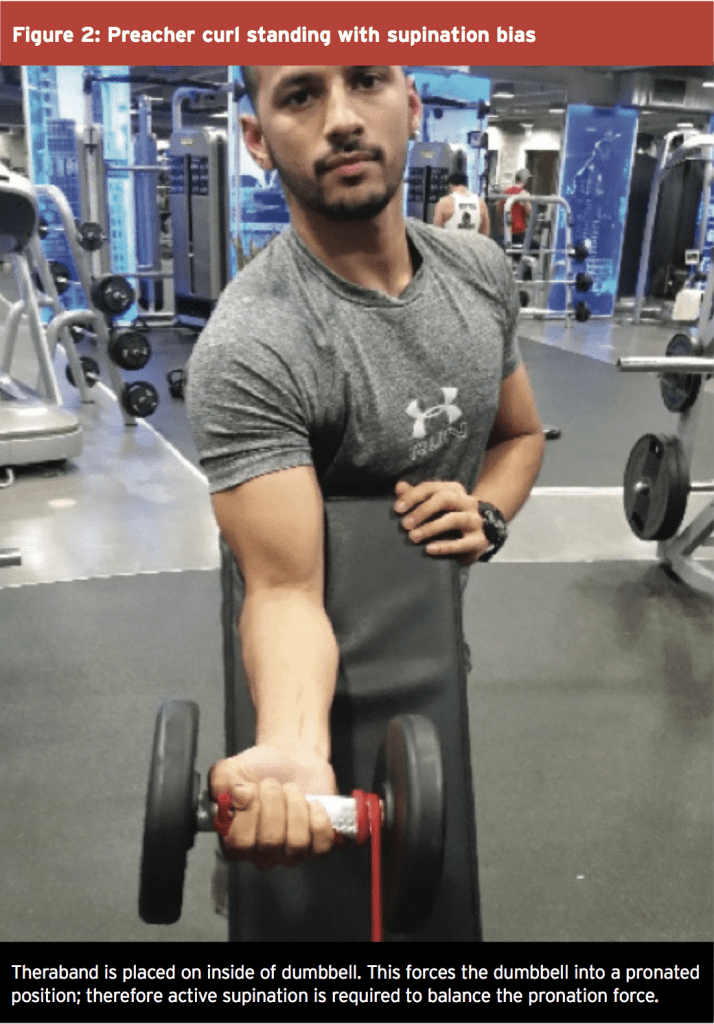
a. Protected range of movement (preacher curl position – see figure 1). Weeks 7,8. i. 3 x 15 reps neutral pronation to full supination (see diagrams below). ii. 3 x 15 reps full supination with isometric supination bias using Theraband. Theraband places a pronation force onto the forearm to create an extra supination effect on the bicep (see diagrams below).
iii. Note: full pronation is avoided initially as this increase compressive load on the distal radial insertion of the tendon.
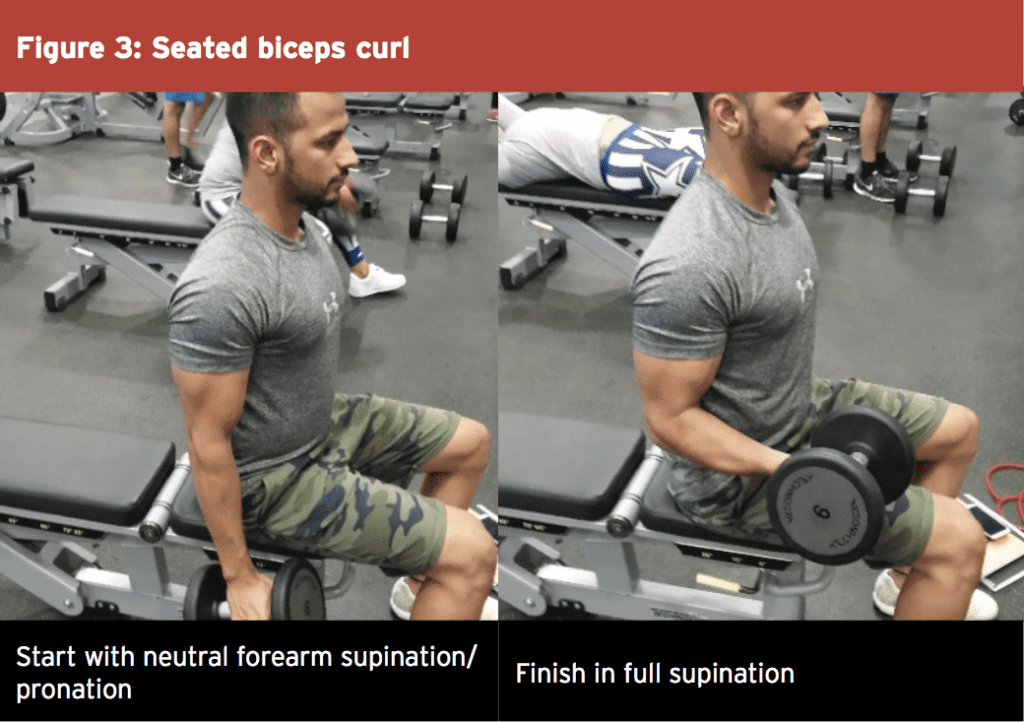
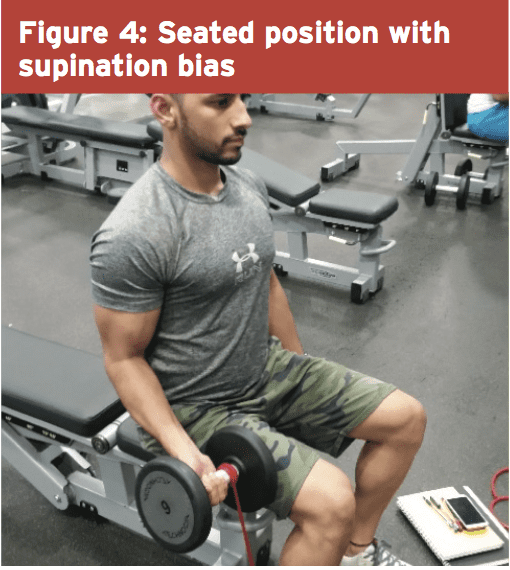
b. Neutral Range of Movement (upright sitting). Weeks 9,10
i. 3 x 15 reps full supination with isometric supination bias (Theraband – figure 2).
ii. 3 x 15 reps neutral pronation to full supination.
iii. Note: full pronation is avoided initially as this increase compressive load on the distal radial insertion of the tendon.
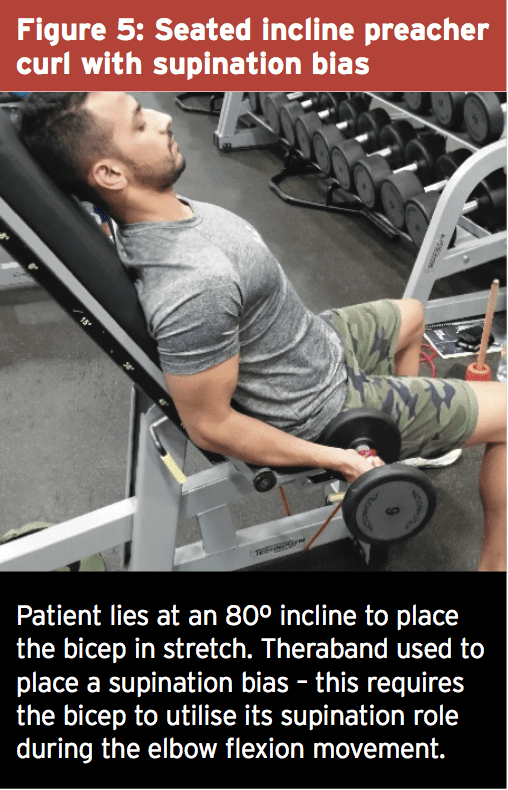
c. Stretch Position (80 degree incline). Weeks 11,12.
i. 3 x 15 reps full supination with isometric supination bias (Theraband).
ii. 3 x 15 reps neutral pronation to full supination.
iii. Note: full pronation is avoided initially as this increase compressive load on the distal radial insertion of the tendon.
2. Commence all pushing movements (bench press, shoulder press). These movements are unrestricted; however use logical progressions based on time away from weight lifting.
3. No deadlifts, cleans or other pulling movements requiring elbow flexion such as chin ups, seated rows. Patients can perform straight arm pulldowns and straight arm reverse flyes.
4. Commence straight line running drills/ technique and build up speed work.
5. Commence running based fitness drills.
6. Continue passive range of movement and scar tissue massage as needed.
7. Superior radioulnar joint mobilisations if required.
Exit criteria
1. Equal isometric elbow-flexion strength. Tested at 90 degrees flexion. Full supination and neutral pronation positions.
2. Straight line speed. Back to pre-injury speed levels.
Phase 4: Advanced Sports-Specific Strength & Skill Acquisition
(weeks 12-18)1. Increase load on 80-degree incline bicep curls, from full pronation to full supination.
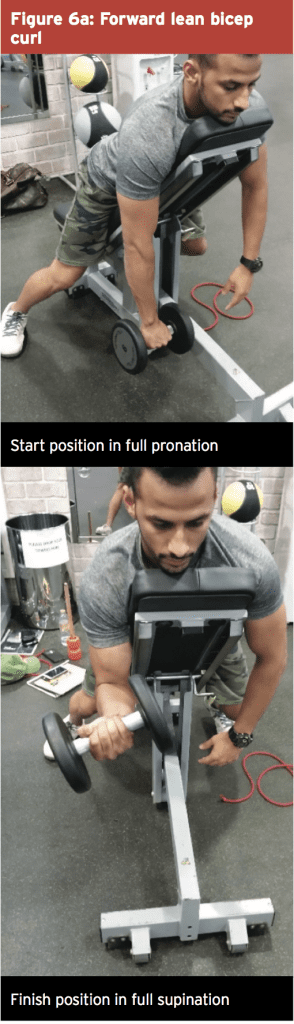
2. Forward lying incline curls with full supination (see figure 6 illustrations below).
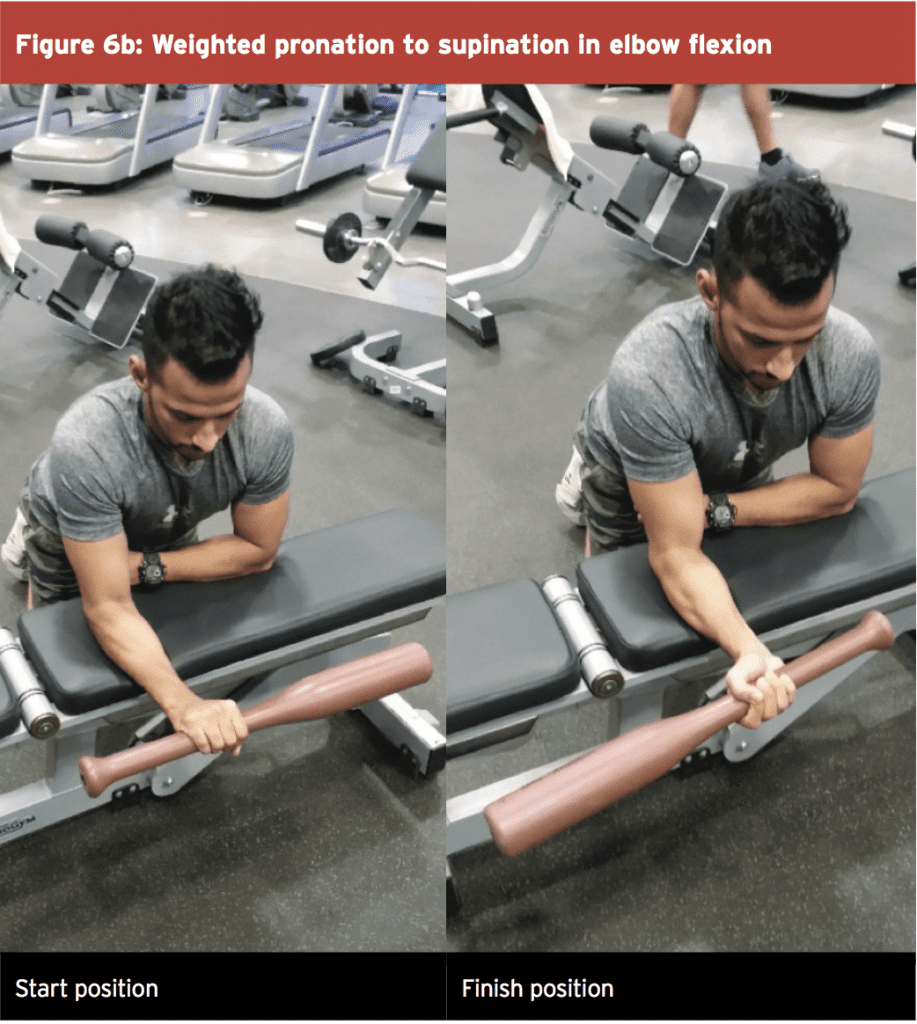
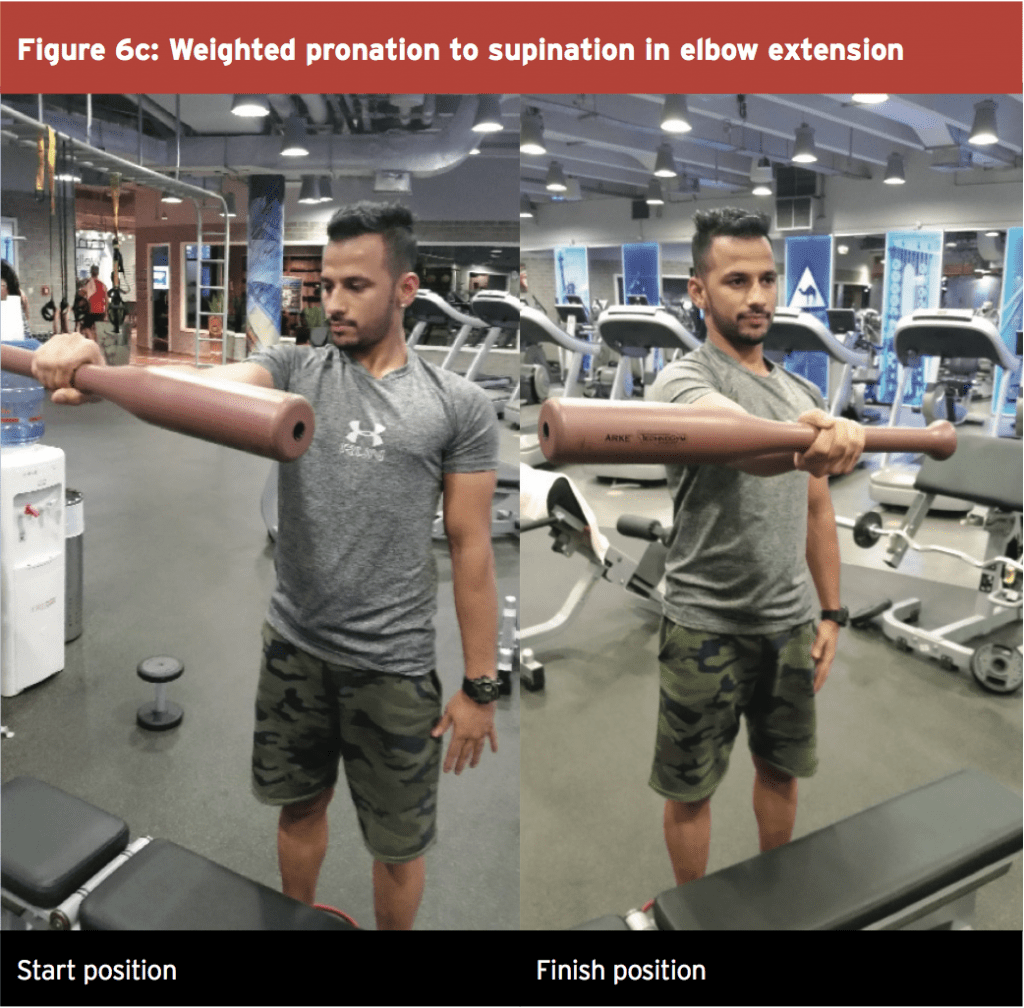
3. Weighted pronation to supination movements. Performed in both elbow flexion and elbow extension, using a weighted bat or hammer. The forearm is taken from full pronation to neutral position (this requires active supination) and then taken down to full supination (this requires an eccentric contraction of the pronators). The weight is then taken back to neutral (pronation contraction) and dropped down to the start position (controlled eccentrically by the bicep).
4. Start sport-specific weight lifting in progressive overload fashion – deadlifts, clean and jerk, all pulling movements (chin ups, seated rows).
5. Return to non-contact skill acquisition.
Exit Criteria
1. Confidence with elbow flexion in strength tasks.
2. Elbow flexion strength 90% compared with unaffected side.
3. Confidence with bicep tendon with skill based efforts.
Phase 5: Return To Competition Phase (Weeks 18-24)
1. Advanced strength and conditioning content.2. Elbow flexion strength 95% compared with unaffected side.
3. Full contact skill if in contact sport.
Conclusion
Distal bicep tendon ruptures in athletes are rare but potentially debilitating if not managed correctly. Surprisingly, a lot of literature exists on the ‘best practice’ management for these injuries. The supporting evidence on the types of different surgeries is quite varied, and the best approach therefore will be determined by the treating surgeon.Irrespective of the type of surgery and fixation used, the rehabilitation process can be quite protracted to ensure the athlete returns to competition with an anatomically sound distal bicep tendon attachment. It also allows elbow flexion strength and supination strength return to the best levels possible.
References
1. J Shoulder Elbow Surg. 2005; 14:516–8.
2. Am J Sports Med. 2009; 37:989–94.
3. J Shoulder Elbow Surg. 2006; 15:614–9.
4. J Shoulder Elbow Surg. 2000; 9:227–33.
5. Am J Sports Med. 2000; 28:538–40.
6. J Bone Joint Surg. 2002;84-A:999–1005.
7. J Hand Surg. 2009;34-A:545–52.
8. Clin Orthop Relat Res. 2008;466: 2475–81.
9. J Shoulder Elbow Surg. 2002;11:633–6.




