Headaches are a highly common afflicting, affecting approximately 66
percent of the general population, causing pain and discomfort which alters an
individual’s quality of life and work rate. Up to fourteen various forms of
headaches have been previously recorded by The International Headache Society.
Particularly, the classification of headache disorders can be greatly
beneficial when diagnosing an individual’s cause of headache.
The IHS classification of headache disorders can be categorized as
follows:
The primary types of headache disorders include, headaches without a
seemingly identifiable cause, for example, tension-type headaches, or TTH,
migraines, chronic daily headaches, medication overuse headaches and trigeminal
autonomic cephalagia, or cluster headache. The secondary types of headache
disorders include, headaches associated with secondary pathologies, for
example, cervicogenic headaches, TMJ, infection, brain tumors and stroke.
Cranial neuropathies, facial pains and other types of headache disorders
include, headaches related to neural disorders of the head and neck, for
example, trigeminal neuralgia.
Since each form of headache has a different pathological foundation and
because an incorrect differential diagnosis will often lead to treatment
failure, it is essential to properly diagnose the type of headache. This is of
particular importance for manual therapy interventions, alternatively, they are
unlikely to be effective for the majority of headache forms. When considering
the best clinical approach to athletes experiencing symptoms of headache, there
is a helpful tool, which can be utilized when contemplating the appropriate
management pathway.
Function of the Trigeminocervical Nucleus
(TCN)
The most
common form of headaches are tension-type headaches, or TTH, affecting up to 38
percent of individuals globally, as compared to migraines, which affect up to
10 percent of the population, chronic daily headaches, affecting 3 percent and
cervicogenic headaches, which affect from 2.5 to 4.1 percent of individuals. Cervicogenic
headaches primarily originate as a result of musculoskeletal dysfunction in the
upper three cervical sections. The prevalence is as high as 53 percent in the
general population or athletes with headache symptoms after experiencing
whiplash-associated trauma.
The mechanism underlying the pain involves the union between cervical
and trigeminal afferent nerve fibers or vessels in the trigeminocervical
nucleus, which travels down the spinal cord to the level of the vertebrae
segments, C3 and C4, in the cervical spine.
The trigeminocervical nucleus has anatomical and functional progression
with the dorsal grey columns of these spinal regions. For that reason, input
through a sensory afferent, particularly from any of the upper three cervical
nerve roots, may be incorrectly perceived as pain in the head, a concept best
referred to as convergence.
Convergence between cervical afferent nerve fibers or vessels, allows for
upper cervical pain to be guided to regions of the head innervated by cervical
nerves, including the occipital and auricular regions. Nonetheless, combining with
trigeminal afferents provides a standard guideline into the parietal, frontal,
and orbital regions. This can cause confusion when diagnosing the cause of
headaches.
Differentiating Headaches
Medically distinguishing the different forms of headache can be
challenging. The subjective information is absolutely crucial.
The following diagnostic criteria have been proposed by the Cervicogenic
Headache International Study Group as follows:
The signs and symptoms of neck involvement as a cause of headaches
includes the precipitation of headache by neck movement, postural changes
and/or pressure over the upper cervical/occipital region, along with the
restriction of neck range of motion, or ROM and the presence of ipsilateral
neck, shoulder or vague arm pain.
Head pain characteristics are described as moderate to severe,
non-throbbing and non-clustering, starting in the neck and spreading to the
head. These can have a varying duration and generally last longer than a
migraine headache with a long-term fluctuating pattern, becoming continuous
when chronic. As for migraines, these can occur most frequently on females, identified
by symptoms of nausea, photophobia and throbbing pain, following a crescendo
pattern.
Diagnosis is based on these subjective features as well as a physical
examination of articular, neural, and myogenic systems while understanding the
mechanisms of the symptoms. Exclusion of red and yellow flags at this stage is
also essential. There can be many structural causes of cervicogenic headaches.
The potential causes of cervicogenic headaches includes: psychosocial
co-morbidities, such as depression and anxiety, along with reported dysfunction
in the joints, muscles, neural tissues, vascular structures and others such as
damage or injury to the temporomandibular joint.
Assessing Cervicogenic Headaches
The goal of the assessment is to reproduce the pain of headache from the
structures surrounding the cervical spine with evidence of an associated
dysfunction. By assessing the articular, neural, and muscular structures during
the evaluation, one can be certain that the source of the individual’s
cervicogenic headaches can be found. Subsequently, if pain cannot be
reproduced, then the involvement of the cervical spine can be dismissed and
other causes of headaches will need further evaluation.
The prevalence of neural tissue pain disorders has been proclaimed among
7 to 10 percent of individuals with cervicogenic headaches. In this case, pain
reproduction can be used as a tool to distinguish neural tissue involvement
when evaluating posture, upper cervical active range of motion, neural
provocation tests combined with upper cervical range of motion, nerve palpation
and neurological examination. In the same manner, if the presence of vascular
involvement is suspected, a clinical framework can be suggested to allow an
accurate guideline for assessment and management, primarily focusing on the
diagnosis and treatment of cervicogenic headaches with articular cause.
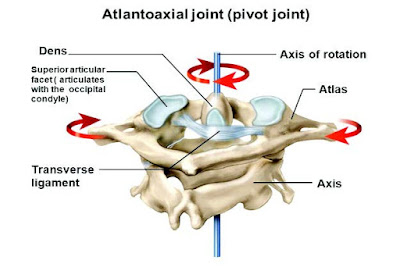
Trauma involving forced cervical flexion, rotation, or side flexion is
very common in sports and physical activities. Similar to testing ligament
stability in the knee joint following trauma, screening for craniovertebral
instability should be prevalent in the assessment.
The Sharp Purser (Transverse Ligament) Test
When screening for craniovertebral instability, it's essential to observe that these tests are most appropriate for diagnosing cervical imbalances. Healthcare specialists must remain aware that other cervical-related complications can also cause pain, such as facet joint disorders, therefore, these should also be assessed accordingly.
To perform this test, the individual must be in a sitting position where the healthcare professional will proceed to place the base of their index finger over the C2 spinous process. The upper cervical spine is flexed. There will be an attempt to translate the affected individual's head posteriorly with the C2 fixed. A positive test is demonstrated by a change in symptoms; a clunk sensation and/or movement of the C1 back towards the index finger on C2.
The Tectorial Membrane (Posterior Longitudinal Ligament) Test
To perform this test, while the individual is sitting, a healthcare
professional will craddle the occiput and head. Fixing the C2 spinous process with
the base of the index finger in a downward directio. The direction of force is
an axial distraction one, attempting to lift the head up on the neck to
separate the two. Normal distraction should not exceed 1-2 mm.
Alar Ligament Test
For this test, in sitting, the individual or athlete’s head will be
craddled while the bific spinous process of the C2 is fixed with the index
fingeer and the thumb. Side flexion down to the C2 is performed by moving the
individual’s head. Any movement of the head without movement of the C2 spinous
process indicates laxity of the alar ligament complex and a positive test.
Flexion/Rotation
The C1-C2 motion segments of the cervical spine accounts for 50 percent
of the rotation in the cervical spine. Therefore, pain originating from an
impairment of this region is a common finding in individuals with cervicogenic
headaches. The flexion-rotation test, or FRT, is an easily applied clinical
test developed to identify dysfunction at the C1-C2 motion segment of the spine.
The Average flexion-rotation test results of the range of motion in the neck of
healthy individuals is 44 degrees. The test is positive if there is pain or
restriction at 10 degrees in the range of motion of the neck on either side.
Due to the lack of intervertebral disc and altered biomechanics of the
high cervical spine, combined movements are assessed differently. The primary
movement available at C0-C1 is flexion and extension at 3 degrees, with the
majority of movement occurring in extension at 21 degrees. Due to the sliding
movement of the occipital condyles, flexion will stress the posterior capsules
on the right and the left at C0-C1. The addition of ipsilateral rotation will
add further pressure to the posterior capsule on the same side. This can be a
nice diagnostic tool for assessing the involvement of C0-C1 as a cause for
cervicogenic headaches.
C0-C1 Flexion/Rotation Assessment
In order for the individual to stretch the right posterior capsule, the
healthcare professional must first stand on the right of the patient and fix
the mandible with their right hand while the left hand supports the occiput.
Then, the specialist should retract into upper cervical flexion and add
rotation using both hands. The goal is pain provocation.
In comparison, upper cervical extensions can stress the anterior
capsules of the C0-C1. The addition of contra-lateral rotation will place
additional pressure to the anterior capsule on the opposite side of the
movement.
C0-C1 Extension/Rotation Test
To stretch the right anterior capsule, the healthcare specialist must
previously be standing on the right of the individual being tested, using the
right elbow, the test will begin by fixing the individual’s trunk. Grasping the
mandible with the right hand to control the head with the left. Protract into
upper cervical extension, followed by left rotation using both hands. The goal
is pain provocation.
Treating Cervicogenic Headaches
Supporting
evidence has suggested that manual therapies are effective for cervicogenic
headaches, specifically spinal adjustments and manipulation from qualified
healthcare professionals, such as a chiropractor, including mobilization
techniques with exercise. This is particularly accurate for cranio-cervical
muscle strengthening and scapula positional re-training. However, further
research is required to determine the effectiveness of manual therapy for
headaches associated with migraines. Several effective treatments and therapy
techniques for cervicogenic headaches can be utilized to relieve the symptoms
of head pain as follows.
Headache Sustained Natural Apophyseal Glide (SNAG)
For a healthcare professional to perform this test, the specialist will
stand by the affected individual’s side and stabilize the head with their right
hand. The little finger is placed on the posterior aspect of the spinous
process of C2. Horizontal pressure is applied to the little finger by the
thenar eminence of the opposite hand along the upper cervical facet plane. This
must be sustained for 10 seconds and repeated 6 times. Pain should be reduced
during this procedure.
Intermittent Pain: C1-C2 Self-SNAG
If the restriction of pain occurs with a right rotation, the strap can
be placed on the posterior arch of the C1 on the left side precisely below the
mastoid process. The left hand will secure the strap and the right hand will
pull on the strap to force rotation at the C1-C2 motion regions. Repeat this
test twice, two times a day.
Intermittent Pain: C2-C3 Self-SNAG
If pain develops from below the region of the C2, then, a different form
of SNAG may be utilized. In this case, the facet plane is towards the affected
individual’s eyes, approximately 45 degrees. The towel edge can be used if a
strap is not accessible. Sustain for 20 seconds, repeat 6 times.
Cervicogenic Headaches and Chiropractic
If a healthcare professional suspects trigeminocervical nucleus
sensitivity, studies have demonstrated that properly managing sleep, stress and
anxiety as well as following a balanced diet with moderate intensity exercise,
can be beneficial for the individual’s specific type of headache. To help those
affected by the dysfunction understand the concept of trigeminocervical
nucleus, or TCN, sensitization, a bucket analogy can describe the concept. When
the trigeminocervical nucleus is overloaded with data, this is similar to a
bucket being overfilled with water. When the TCN receives too much information
at once, the bucket overflows, hence, causing they symptoms of a headache. If
an athlete can control the level of incoming information, they can control the
level of trigeminocervical nucleus sensitization.
Treatment relies on the diagnostic criteria, but where appropriate,
alternative treatment options, such as chiropractic care, can be beneficial to
assess and treat headaches, including cervicogenic headaches. In particular,
manual therapy has good evidence to support its foundation in treating and
managing cervicogenic headaches. Chiropractic care focuses on musculoskeletal
injuries and conditions, including dysfunction of the nervous system. With the
use of chiropractic adjustments, a chiropractor can carefully re-align the
structures of the spine, helping to reduce the pressure of the tissues as a
result of irritation and swelling, ultimately improving the individual’s
symptoms.
Before treatment however, the athlete should always be aware of vascular
involvement and test for craniovertebral instability, particularly after trauma
in specific sports and physical activities.
By Dr. Alex Jimenez