Chiropractic injury expert, Dr. Alexander Jimenez looks at the human anatomy and biomechanics of the tibialis posterior, & outlines suitable examination protocols as well as the treatment and management alternatives for dysfunction.
The tibialis posterior tendon (TPT) is a major player in the best performance of foot biomechanics, especially since it provides stability to the lateral longitudinal arch (MLA)(1). Dysfunction not only poses as pain on the inside of the lower leg and ankle, but can also be a primary cause of horizontal feet in the event of tendon rupture -- or vice versa, with inherently flat feet causing tendon overload(two). Many health professionals are yet to fully appreciate the significance of the tibialis posterior tendon and its significant role in injury incidence, which makes it important to raise recognition of this condition(3).
Dysfunction Incidence
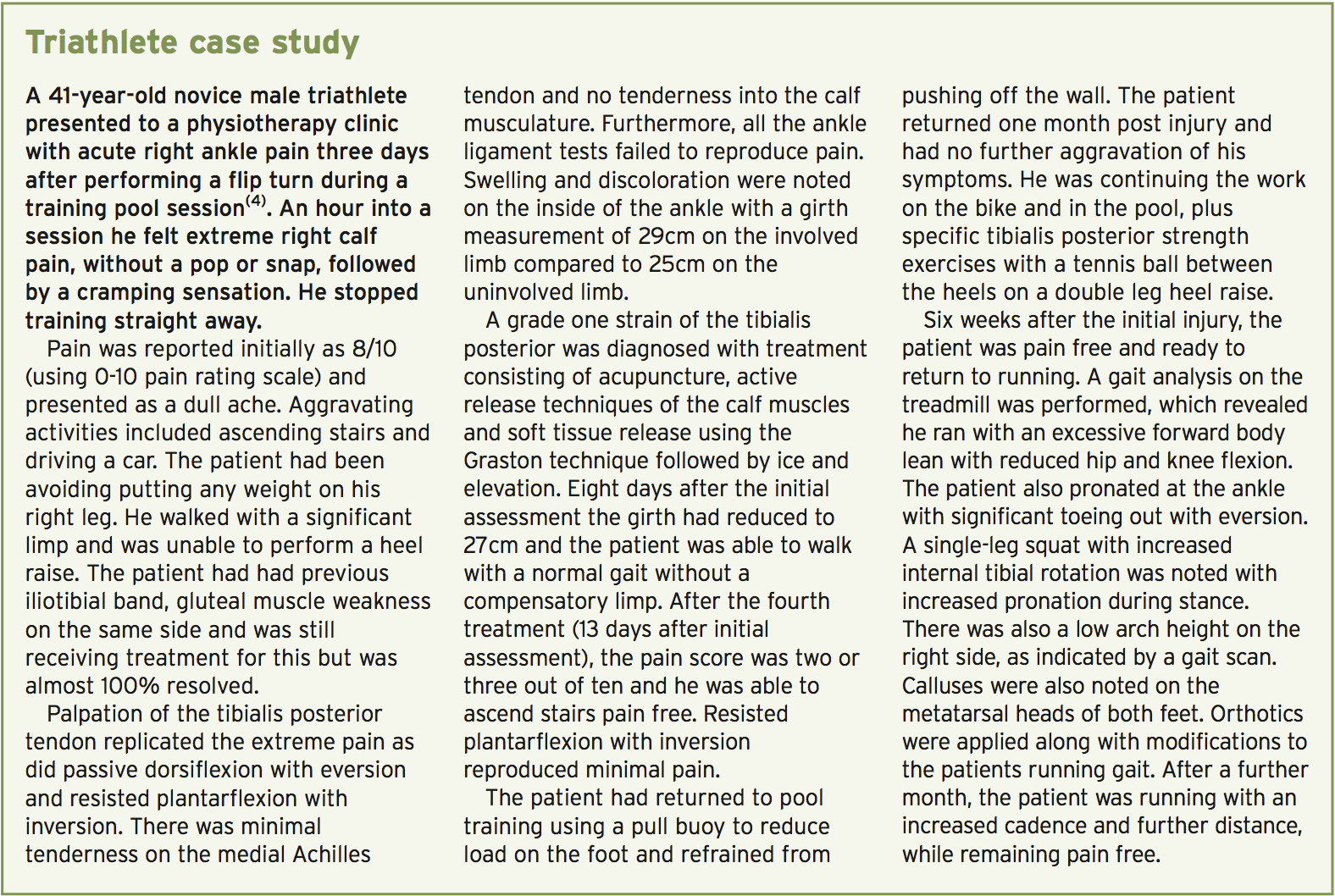
Lots of risk factors are identified in the incidence of tibialis posterior tendonitis dysfunction. Excess weight is a variable, with heavy middle-aged women being diagnosed in 10% of instances(2). Other aspects including pes planus (flat feet), steroid injections around the tendon, hypertension, diabetes and rheumatoid arthritis(3).Triathletes often present with this injury because of the persistent loading across both disciplines(4). The demands on this tendon from running are apparent; with poor biomechanics, it is easy to see how the tendon can become overloaded and breakdown occurs. In swimming, the requirements are not so obvious.
But, putting the ankle in plantar flexed position (by simply pointing the feet from freestyle swimming) raises the muscle shortening on the calf complex. Additional to this is the repetitive pushing off the wall at pool swimming. Also as poor foot biomechanics, some of the more frequent factors can lead to tendon overload such as raising training volume/load fast, hill reps, erroneous fitting footwear(4).
During a triathlon consequently, the calf muscle shortening in the swim and the high force production during the bike ride are joined when penetrating the run, which means the run begins with the calf muscles having already been loaded greatly, causing additional fatigue. Thus effective training with good recovery protocols is essential for preventing this sort of injury in triathletes.
Anatomy & Biomechanics
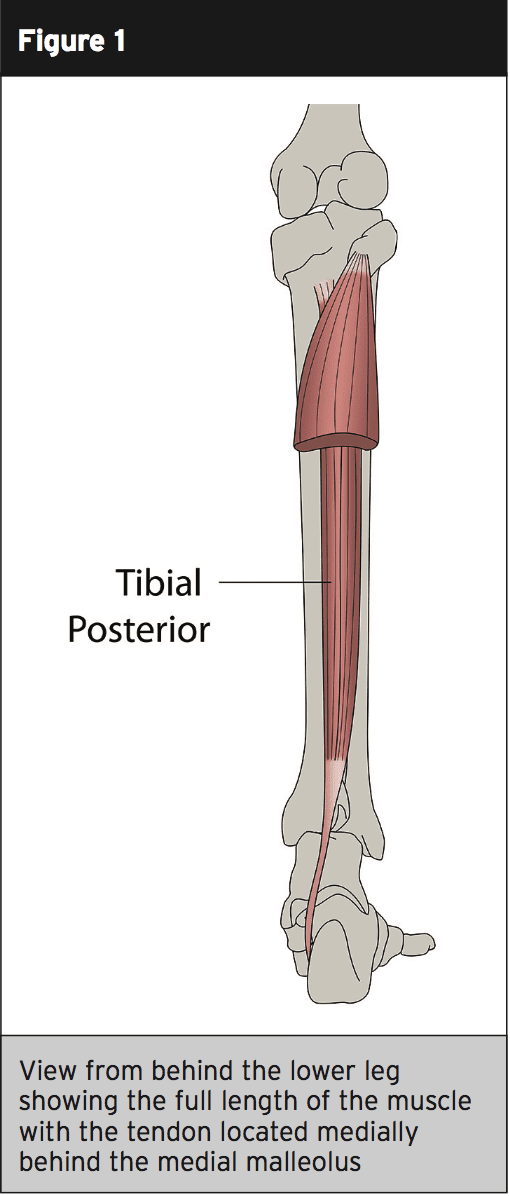
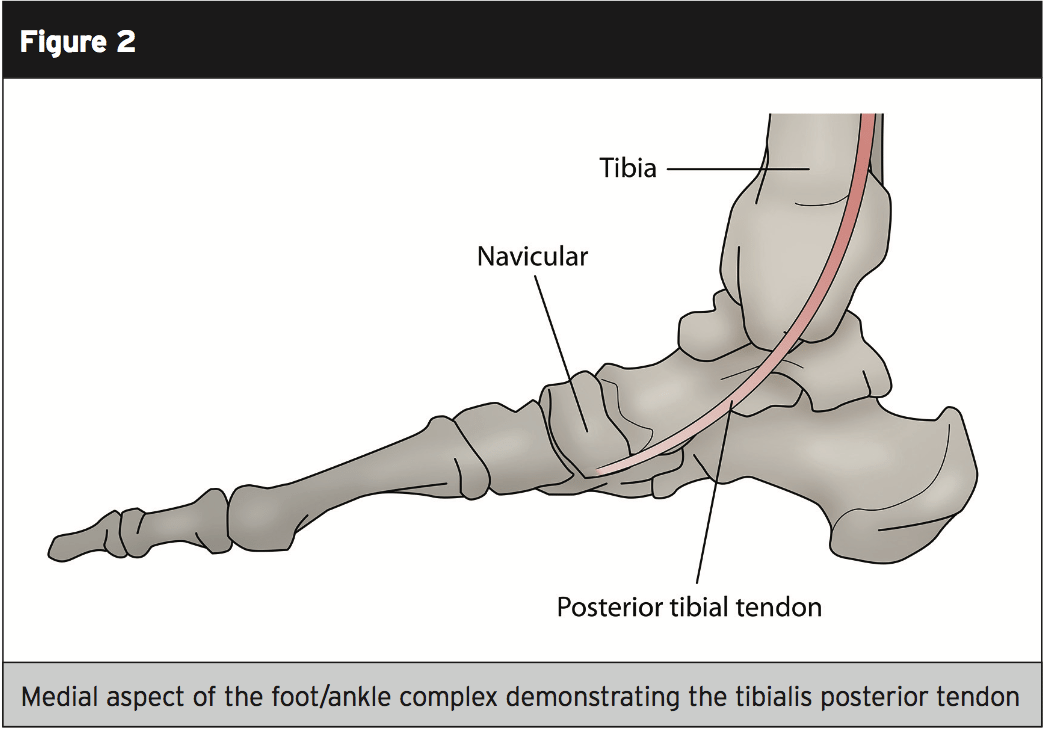
The tibialis posterior (also known as the anterior tibial tendon) originates in the posterior surface of the tibia on the external component, with a muscular attachment to the medial surface of the fibula, and the interosseous membrane between the tibia and fibula(2). It paths through the deep posterior compartment of the lower leg, together with the more dominant calf musculature of the gastrocnemius and soleus, and goes behind the lateral malleolus of the ankle. It is at this stage (just behind the medial malleolus) that the blood supply is diminished(2).At the distal attachment, then the tibialis posterior divides into three sections with the major section attaching to the navicular tuberosity (bony prominence) on the inside of the foot(2). The plantar segment attaches to the second, third and fourth metatarsals, second and third cuneiforms, and the cuboid bone. The third section referred to as the recurrent portion attaches to the sustentaculum tali of the calcaneus (see figures 1 and 2).
Pathophysiology
A substantial period of time in an air cast boot or pot might lead to weakness of this tendon and a reduced height of the MLA. A complete rupture of the tendon in the foot attachment does not have to occur to get a flat foot deformity to occur. Therefore, a rehabilitation program must include strengthening exercises of the foot inverters. Whether this strength work is not carried out then the tibialis posterior tendon can become vulnerable and repeated micro trauma can cause the tendinosis to occur.As the tendon degenerates it is substituted with fibrotic tissue, and this frequently occurs in areas with inadequate blood flow in areas like supporting the lateral malleolus(2). Bubra and colleagues have stated that because of the rear foot valgus affects, a contracture can occur of the achilles tendon resulting in changes into the forces applied at the back foot(2). These modifications in applied forces can lead to pain because of the touch of the fibula and the lateral calcaneum. A further biomechanical factor linked to changes in the back foot is that the contracture of the peroneus brevis, which causes a mechanical force exerted to the opposing tibialis posterior tendon.
Evaluation
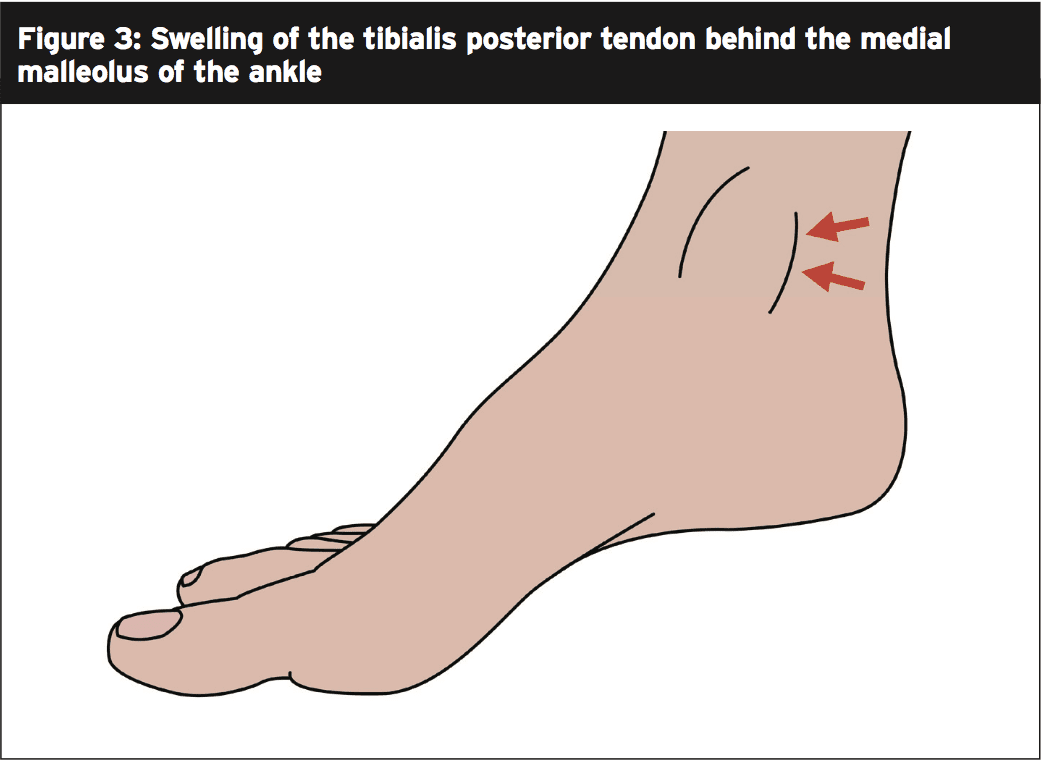
It's critical to formulate a thorough examination protocol when you suspect tibialis posterior tendinosis may be a potential. The first thing to check to get is any swelling behind the medial malleolus of the ankle (figure 3), and when combined with changes in foot shape, has been proven to have 100% accuracy for tibialis posterior tendon dysfunction diagnosis(3).
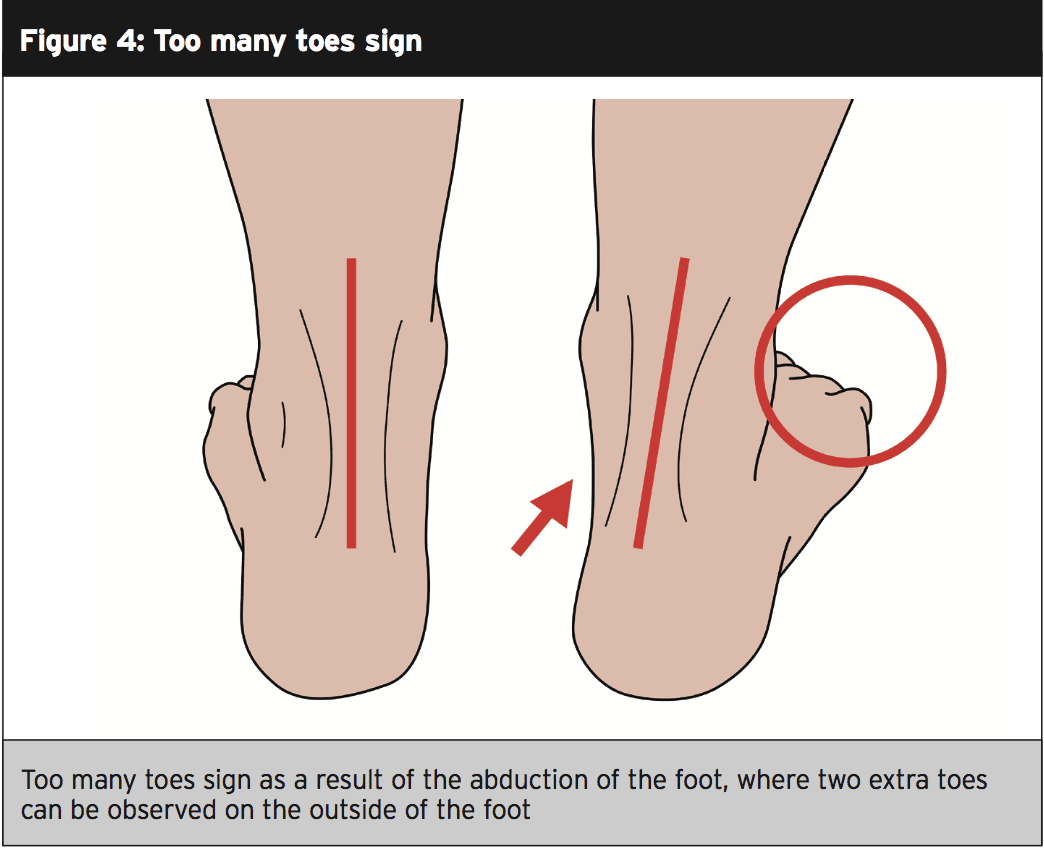
Patients presenting with stage-one tendon degeneration typically present with vague medial foot pain on the inside of the foot, and with swelling behind the ankle(3). These patients have no history of trauma. Observe the lower leg from behind using the ‘too many toes sign’ (figure 4), which if positive indicates rear foot valgus deformity that coincides with flattening of the MLA and compensatory forefoot abduction(2).
The ability of the muscle-tendon unit can be analyzed by resisting from a dorsiflexed/ everted position into plantarflexion- inversion, which follows the actions the muscle actively eases(3).
An X-ray taken of the two lower limbs is utilized to observe the individual in standing. The radiographs are best taken in the front and also the outside of the ankle to best view for the presence or lack of degenerative changes in the subtalar and talocrural joints. Even though a radiologist may further request an MRI scan or ultrasound scan, researchers at the Royal National Orthopedic Hospital, UK, have contended that clinical evaluations for tibialis posterior thoracic pain are adequate for forming a diagnosis(3).
Treatment & Management
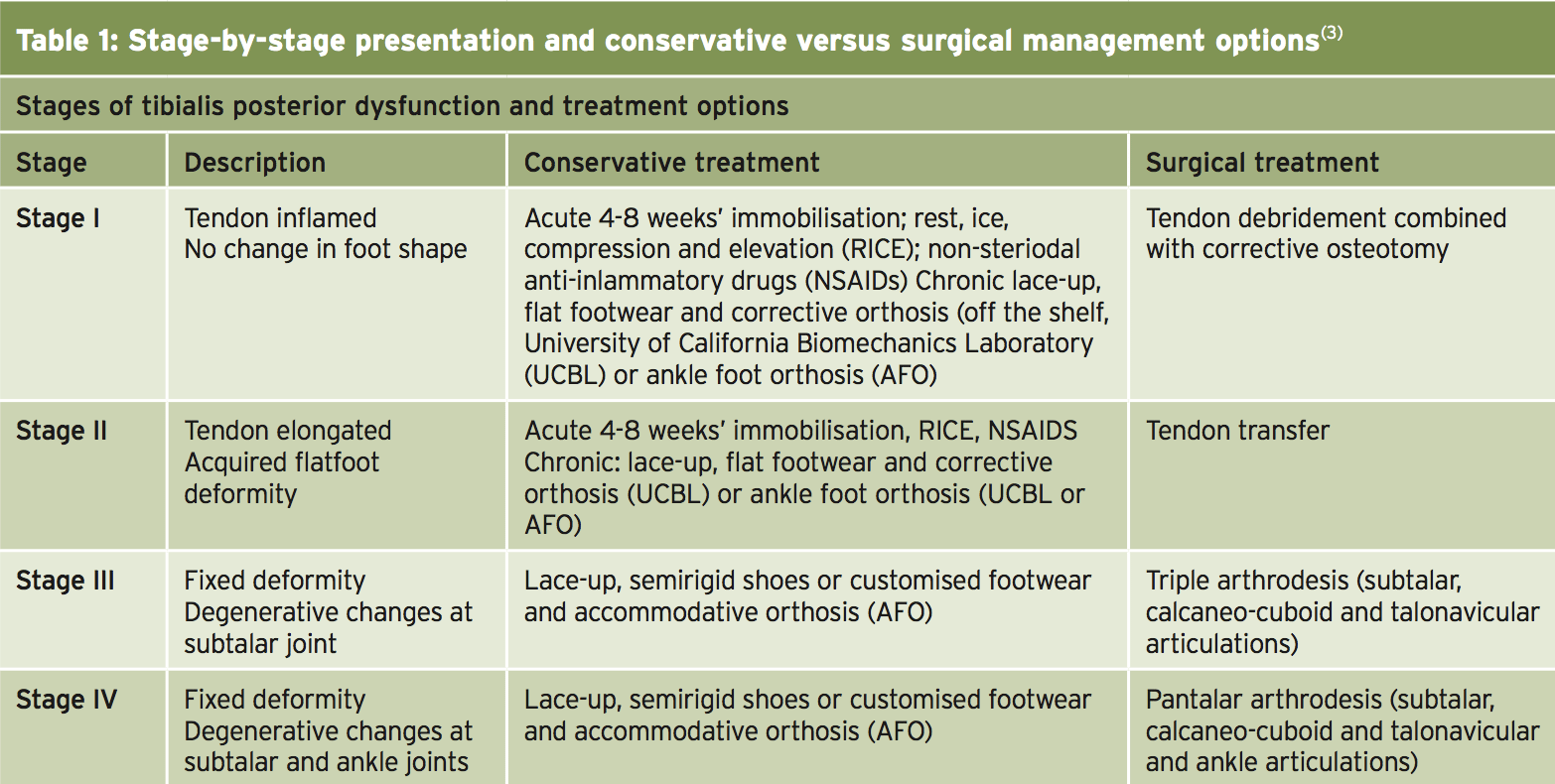
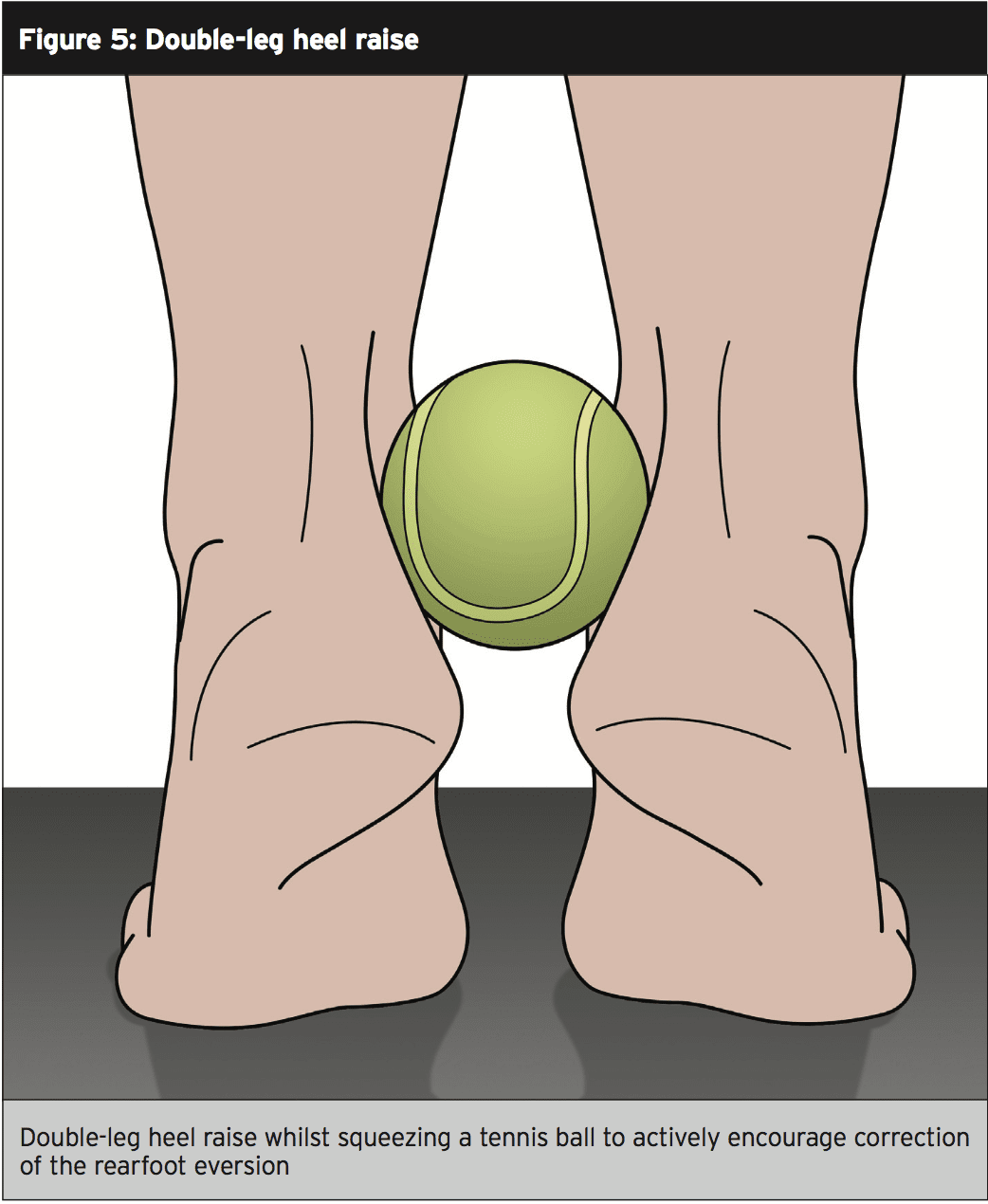
Tendon degeneration can be simplified into four different phases (Table 1), and the proper therapy at each phase will therefore largely be dependent on the stage of injury. Stages three and four are less commonly observed in athletes, however, at the same time, it is important to acknowledge the progression tendon degeneration can take.Summary
A variety of conditions exist as risk factors in the occurrence of tibialis posterior tendon disorder, and these should be regarded as part of the examination. It is important to apply emphasis on the successful rehabilitation of ankle injuries either acutely, or after surgery, to make sure that prior injury does not cause tendon dysfunction later on. Successful screening should take place among an athletic squad to make sure that nobody is present with abnormal foot biomechanics that may cause tendon degeneration.References
1. Blasimann – J Foot and Ankle Res, 2015, 8, 37
2. Bubra – J Family Med Prim Care, 2015, Jan, 4, 1, 26-29
3. Kohls-Gatzoulis – BMJ, 2004, 329, 1328–1333